4
Traumatic Injuries of the Pediatric Craniocervical Junction
Traumatic injuries of the pediatric craniocervical complex occur at a high frequency. Therefore, we dedicate a separate chapter to considering the various injuries that can occur. Each injury or injury pattern is discussed in detail, starting with its definition, clinical presentation, radiographic diagnosis, and treatment, so that pediatric spine surgeons may better understand the nature of these injuries.
As discussed in earlier chapters, injury to the pediatric spine differs from injury to the adult spine in several important ways. These include the anatomical and biomechanical features of the pediatric spine, the mechanism of injury, injury pattern, criteria for determining instability, and outcome. The pediatric craniocervical complex is particularly susceptible to injury. There are four major injury patterns in the pediatric craniocervical junction: (1) longitudinal subluxation with failure of the major stabilizers across the occiput–C2 (O–C2) unit, (2) translational atlantoaxial subluxation, (3) atlantoaxial rotatory fixation, and (4) fractures. There are also four major injury patterns in the pediatric subaxial spine: (1) ligamentous and soft tissue disruption, (2) bony anterior column injuries, (3) bony posterior column injures, and (4) combined anterior and posterior column, injuries. Each injury pattern is discussed in turn, with relevant details provided for the management of complex injuries in the craniocervical complex in children.
 Craniovertebral Junction Injuries
Craniovertebral Junction Injuries
Longitudinal Occiput–C2 Subluxation
Injury Description Longitudinal subluxation results in the separation of the occiput to C1 or C1 to C2 or both. The former pattern is more common, and the injury is commonly referred to as atlanto-occipital (A-O) dislocation. Autopsy studies of children with fatal atlanto-occipital dislocations often reveal disruption of all ligaments connecting the occiput to the atlas and axis as well as transection of the spinal cord or brain stem.1–3 Rupture of either or both the tectorial membrane and alar ligaments invariably occurs with rupture of the joint capsule. The posterior cervical and suboccipital musculature is sprained or lacerated, and the prevertebral fascia is infiltrated with blood. There are usually no fractures. In older children and adults, stronger ligaments can result in avulsion fractions at the ligamentous attachment of the occipital condyle or the base of the clivus as opposed to rupture of the ligaments themselves.3–5
The exact vectors of impact that create this injury are not known. The incidence of associated facial injuries, particularly submental lacerations and mandibular fractures, is high.3 Posterior atlas fractures with posterior atlanto-occipital dislocations have also been observed in adults.6 These findings are consistent with a hyperextension injury. Furthermore, nine of 12 victims of atlanto-occipital dislocation in Adams’s autopsy study sustained pontomedullary lacerations,3 which are associated with hyperextension7,8 and rotational injuries.9 Approximately 25% of reported atlanto-occipital dislocations, however, have coexistent atlantoaxial subluxation or separation of the posterior elements of atlas and axis, suggesting a hyperflexion injury.10 Autopsy studies also reveal spinomedullary contusions or transections adjacent to the dens where the tectorial membrane is disrupted, as if the dens protrudes through the tectorial membrane during extreme flexion.3,11 Lateral flexion and extreme rotation are also thought to play a role in this injury type.12–14 Taken together, these reports suggest that atlanto-occipital dislocation can probably occur as a result of either hyperflexion or hyperextension that tears the tectorial membrane, in combination with extreme rotation, lateral flexion, and distraction that disrupts the alar ligaments.
Clinical Presentation In the past, atlanto-occipital dislocation was considered a rare and usually fatal injury.15 More recently, a larger number of survivors, especially children, have been reported.14–19 Several factors may contribute to the increase in survival, including quicker response times to the scene by emergency medical teams, better initial cervical spine immobilization, and earlier diagnosis of injury.
Children with traumatic atlanto-occipital dislocation usually present with cardiorespiratory instability and neurological findings indicating brain stem, spinal cord, and cranial nerve injuries. In several studies, 30% of children who survived atlanto-occipital dislocation were apneic or in full cardiorespiratory arrest at the accident scene.15,16,19–24 Neurological findings indicating brain stem injury include pupillary abnormalities, rotatory nystagmus, ocular bobbing, and decerebrate posturing. Motor deficits vary depending on the level and degree of injury. The caudal six pairs of cranial nerves are frequently injured. Axial traction of the medulla may stretch or avulse the lower cranial nerves from their exit foramen at the base of the skull.25 Subsequent difficulty with aspiration and swallowing confers significant morbidity. Positive computed tomographic (CT) scans of the head in children with atlanto-occipital dislocation most commonly show diffuse swelling, with subarachnoid blood in the basal cisterns or intraventricular blood in the III and IV ventricles. Acute and delayed hydrocephalus with syringomyelia have been observed.21,26
Radiographic Diagnosis The diagnosis of atlanto-occipital dislocation requires diligent analysis. This injury may be suspected in high-speed trauma victims, especially those with facial injuries and cardiorespiratory instability. Longitudinal O–C2 dislocation on plain radiographs of survivors may be subtle and is frequently missed. Early diagnosis is crucial to prevent additional devastating neurological injury. The first clue is often widening of the retropharyngeal space beyond 7 mm seen on lateral cervical radiographs. Several criteria based on the relationship of key anatomical landmarks have been proposed to recognize O–C2 instability; these are outlined in the discussion of craniovertebral biomechanics in Chapter 2.

Figure 4–1 Disruption of ligaments in atlanto-occipital dislocation. The long arrow shows magnetic resonance imaging evidence of a tear in the tectorial membrane. The short arrow shows evidence of blood layering posterior to the dura.
All patients with suspicious findings on plain radiographs, based on any of the described criteria, should undergo CT and magnetic resonance imaging (MRI) from the occiput to C2 with reconstructed sagittal and coronal images. In cases of atlanto-occipital dislocation, a sagittal CT reconstruction through the atlanto-occipital joint often demonstrates an abnormal separation or translation of the cup-shaped articulation. In subtle cases of longitudinal separation, the adjacent joint diastasis serves as a comparison. MRI can delineate the disruption of the ligaments with a complete tear or bowing of the tectorial membrane (Fig. 4–1). Furthermore, the extent of brain stem and spinal cord damage and the presence of associated structural compression can be seen with MRI. In cases where atlanto-occipital dislocation is reduced at presentation, plain films and CT may fail to demonstrate any bony abnormality. These injuries have been reported to become apparent only with traction, a precarious situation.27
Traynelis and colleagues have classified atlanto-occipital dislocation into three types (Fig. 4–2).10 Type I is characterized by the anterior displacement of the occiput relative to the atlas; type II is characterized by a longitudinal separation between the two structures; and type III is associated with the posterior displacement of the occiput. In addition to these three types, isolated examples of pure lateral dislocation as well as pure rotatory subluxation have been reported in children, the latter with atlantoaxial rotatory fixation.28–30 The majority of traumatic atlanto-occipital dislocations in children are type I. Given the highly unstable nature of this injury in children, the direction of occipital displacement may be more a function of patient positioning than of the mechanism of injury. As a child lies on a flat board, the larger head relative to the thorax will flex the neck. If atlanto-occipital dislocation exists, the displacement will tend to be anterior. In 1948, Farthing reported the only case of traumatic type III dislocation seen in a child where the child’s neck was extended on presentation.31 Because axial stabilization of the entire O–C2 unit is supplied by the ligaments from the occiput to C2, longitudinal abnormalities at the C1–C2 articulation can be considered a different manifestation of the same injury.32 Anderson and Montesano propose that this injury is a variant of type II atlanto-occipital dislocation (type IIb).33
Treatment Management of atlanto-occipital dislocation begins with rapid cardiorespiratory resuscitation. Immobilization must be provided immediately and maintained until definitive stabilization. The use of cervical traction or failure to provide immobilization can have catastrophic consequences. Immobilization should be provided with a cervical collar until halo orthosis can be applied. Neutral positioning alone during initial immobilization in a cervical collar can help reduce atlanto-occipital dislocations without the need for traction. As mentioned, the larger head of the child relative to the torso tends to flex the neck and maintain an anterior dislocation. Elevation of the thorax with firm padding or blankets with the child placed in the cervical collar can eliminate the size discrepancy and help reduce the dislocation. An oversized collar can exacerbate longitudinal distraction, even with the child in a neutral position. The reverse Trendelenburg position with elevation of the head in a proper collar can correct a type II dislocation.

Figure 4–2 Traynelis classification of atlanto-occipital dislocation. (A) Normal; (B) type I (anterior); (C) type II (vertical); (D) type III (posterior).
Definitive stabilization requires surgical fusion. Although spontaneous fibrous fusion with immobilization alone has been reported in children,12,26,34 persistent instability is generally the rule because purely ligamentous spinal injuries heal poorly.14,16,31,35 In such cases, fusion across the entire O–C2 unit must be strongly considered. Although overt C1–C2 separation from disruption of the O–C2 connections may be visualized, covert C1–C2 instability cannot be separately elicited in the presence of O–C1 separation. In fact, C1–C2 longitudinal instability may be assumed, given the failure of the ligaments from the occiput to C2.
Atlantoaxial Rotatory Subluxation
Injury Description Atlantoaxial rotatory subluxation (AARS) consists of a spectrum of rotational abnormalities involving the atlas and the axis, including atlantoaxial rotatory fixation (AARF). This spectrum ranges from mild abnormalities of rotation to absolute fixation with no motion. AARS may arise from several potential mechanisms. In some cases, physiological hypermobility of the atlantoaxial articulation in children may lead to rotatory subluxation during sudden and vigorous turning of the head.36 This can occasionally cause a true bony lock. In other cases, the redundant synovial folds in children may become trapped in joint spaces at the extreme of rotation and cause a jam during counterrotation. Concurrent muscle spasms may then exacerbate this fixation.
Clinical Presentation AARS often occurs with little or no preceding trauma.37,38 This injury has been described after infections of the head and neck, such as pharyngitis, otitis media, retropharyngeal abscesses, or tumors.39 Torticollis after pharyngeal inflammation has been called Grisel’s syndrome. Traumatic AARS occurs in only 30% of cases of AARS, and the trauma is usually minor. Children present with neck pain, with the neck maintained in lateral flexion and the chin rotated to the contralateral side (a “cock-robin deformity”). The neurological examination is usually normal, Rarely, patients present with myelopathy or C2 radiculopathy.40,41 Since its first description in 1830,42 several reports of this condition have been published, but the diagnostic criteria are under debate.
Radiographic Diagnosis Fielding and Hawkins devised a classification scheme for AARS based on analysis of plain films.41 In their study, four types of AARS are described. Type I rotatory subluxation is characterized by rotatory fixation without anterior shift of the atlas. This is the most common type described in children and is the most stable because the transverse ligament should remain intact. Type II consists of rotatory subluxation with an anterior shift of greater than 3 mm but less than 5 mm. This type involves compromise of the transverse ligament and is more dangerous. Type III involves rotatory subluxation with an anterior shift of greater than 5 mm. Type IV is a rare and usually fatal injury that involves rotatory fixation with a posterior shift. The relationship of C1 to C2 can be well visualized with three-dimensional CT scans (Fig. 4–3). Recent studies using dynamic CT have also successfully visualized AARS and AARF.39,43 Lee and Pang have used deviation from the normal C1–C2 motion curve described in Chapter 2 to diagnose AARS.44
Treatment The treatment for AARS may consist of conservative therapy alone, nonsteroidal anti-inflammatory drugs, muscle relaxants, use of a soft collar or hard cervical collar, halter traction, cervicothoracic orthosis, halo traction, and cervical fusion. The majority of patients with type I injury improve with a combination of medical therapy and traction.39,43,45 Once reduction of the injury is achieved, immobilization for 4 to 6 weeks in a collar is recommended. Studies have shown that the duration of symptoms prior to treatment is a critical factor in determining the response to more conservative treatment.39 Recurrences of type I injuries may indicate transverse ligament incompetence and may require C1–C2 fusion. Type II and III injuries should be considered inherently unstable because of injury to the transverse ligament and require C1–C2 fusion.
Translational Atlantoaxial Subluxation
Injury Description Translational atlantoaxial subluxation without fracture occurs when there is ligamentous instability. Loss of the transverse ligament allows the spinal cord to become compressed between the odontoid and the posterior arch of the atlas. Traumatic translational atlantoaxial subluxation is an extremely rare injury in children that occurs as the result of violent trauma, with few survivors.46,47 Most cases of traumatic translational atlantoaxial subluxation result from flexion injuries48; however, there are rare injuries with posterior C1–C2 subluxation in the presence of a normal odontoid and C1 ring caused by hyperextension or C1–C2 distraction.49 Nontraumatic translational instability of C1–C2 is associated with laxity of the transverse ligament or hypoplasia of the odontoid. This occurs in several developmental disorders, including Down syndrome, Klippel-Feil syndrome, and many of the skeletal dysplasias.
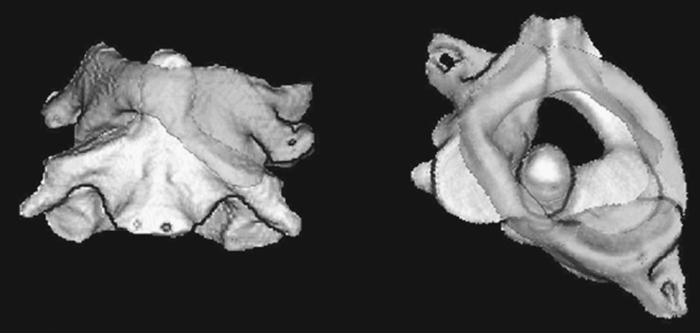
Figure 4–3 Three-dimensional reconstruction of a computed tomographic scan of a patient with type I atlantoaxial rotatory fixation. (Courtesy of Dr. Ronald Cohen at the Children’s Hospital at Oakland.)
Clinical Presentation In most patients who present with translational atlantoaxial subluxation, the injuries result from high-speed pedestrian– vehicular accidents.37
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





