Tongue Mucosal and Musculomucosal Flap for Lip Reconstruction
J. GUERREROSANTOS
EDITORIAL COMMENT
The use of tissue from the undersurface of the tongue is preferable for lip reconstruction because the dorsum of the tongue has a papillary appearance that does not change significantly with time. In addition, tongue flaps used for lip reconstruction need constant moisture because of their tendency to dry and scale.
INDICATIONS
The tongue musculomucosal flap can be used in reconstruction of both the upper and lower lips. For carrying out surgical repairs, one can use one or two tongue flaps that can be combined, when necessary, with skin flaps. Most frequent indications for this procedure are defects subsequent to removal of benign or malignant tumors, defects after trauma, and secondary deformities because of clefting.
ANATOMY
The principles of tongue mucosal and musculomucosal flaps are based on the fact that the blood supply to the mucous
membranes is derived from the perforating vessels of underlying muscle (5, 6). The tongue is a mobile mass of striated muscle covered by mucous membrane. It may be divided into a fixed part, which is the root, and a mobile part, which is formed by the body and apex. The body is divided into two halves by a median raphe that is seen externally as the median sulcus (Fig. 177.1).
membranes is derived from the perforating vessels of underlying muscle (5, 6). The tongue is a mobile mass of striated muscle covered by mucous membrane. It may be divided into a fixed part, which is the root, and a mobile part, which is formed by the body and apex. The body is divided into two halves by a median raphe that is seen externally as the median sulcus (Fig. 177.1).
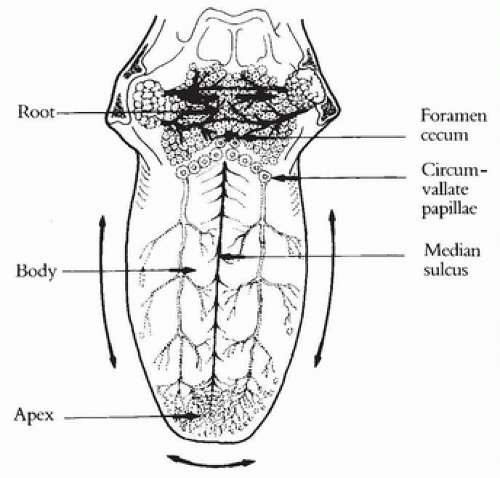 FIGURE 177.1 Anatomy and blood supply of the tongue. Abundant communicating arterial branches and arcades in lingual apex. |
The areas of the tongue covered by the mucous membrane are the apex or tip, the dorsum, the right and left margins, and the inferior surface. The root of the tongue is irrigated by the lingual artery and vein, which have transverse branches; from this part, transverse flaps can be taken. The mobile part of the tongue is irrigated by the ranine arteries and veins. The ranine arteries course next to the deep muscular mass and, forward of this point, have 10 to 12 collaterals.
The terminal branches anastomose in the lingual apex, forming the ranine arch. The median raphe separates both sides perfectly in the lingual body without any vascular anastomosis; this was recently confirmed in arteriographic studies. Longitudinal flaps can be obtained on the lingual body; it is not advisable to design flaps that cross the median raphe. Longitudinal as well as transverse and bipedicle flaps can be created on the apex because of the rich vascularity (see Fig. 177.1).
FLAP DESIGN AND DIMENSIONS
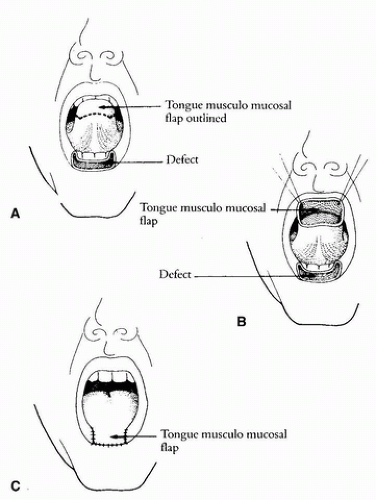
Three basic factors must be considered in designing a successful tongue flap. First, the exact location, width, and length of the flap depend on the location and size of the defect at the recipient site in the lip. Second, the outlines of the flap should be made following the direction of the blood supply in the root, body, and apex. Third, tension and distortion are the main enemies of successful tongue flap repair; good arterial and venous blood supply and gentle handling of the tissue are the only allies. A flap site that avoids tension from the mobility of the tongue should be selected (Fig. 177.2).
Although tongue musculomucosal flaps can be obtained equally well from the dorsum, lateral margins, or inferior surface, it is recommended that flaps for labial reconstruction be taken from the margins or the undersurface because the mucosa of these areas is smooth and resembles vermilion. It is not wrinkled and does not have papillae like the mucous membrane of the lingual dorsum.
OPERATIVE TECHNIQUE
Reconstruction of the Lower Lip
Direct Tongue Musculomucosal Flap
When total vermilion reconstruction is planned, a single flap is taken from the tip and margin and applied to the lower lip as a single unit. This flap can be used when a lip shave is done in cases of leukoplakia or multiple small epitheliomas. The flap is designed with a single pedicle, including the right amount of muscle for aesthetic reconstruction (Figs. 177.2 and 177.3). After careful hemostasis, the flap is sutured in a single layer, with a small raw area left in the pedicle. After 3 weeks, the flap is ready to be divided along a line 1.5 cm behind the posterior margin of the defect. In some cases, a surgical revision is made some months later to correct a residual bulge. Occasionally, the flap has a dark red color because of vascular congestion, and this coloration may last for some months; it later fades.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree