Topical Wound Agents.
Following admission to the burn center, the patient’s wounds are cleansed with soap and water. Loose tissue and blisters are debrided. Body and facial hair are shaved if involved in the area of a burn. Daily wound care is performed on a shower table with soap and tap water or, if the burn wound is small, at the patient’s bedside following a shower. The use of tanks for wound care has fallen out of favor because of the risks of cross-contamination.
Burn injury destroys the body’s protective layer from the environment and dressings are needed to protect the body from infection and minimize evaporative heat loss from the body. The ideal dressing if it existed would be inexpensive, easy to use, require infrequent changes, and be comfortable. While a number of topical agents are available for burn wound care, it is best to have a simple, well-reasoned wound care plan.
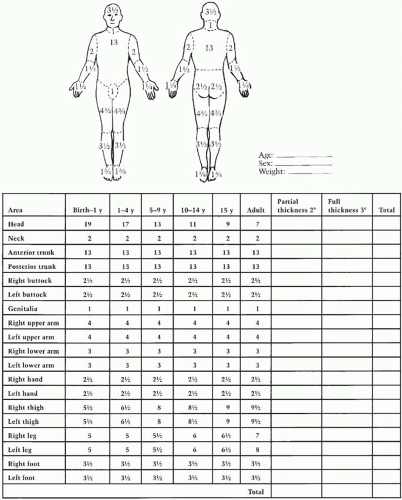
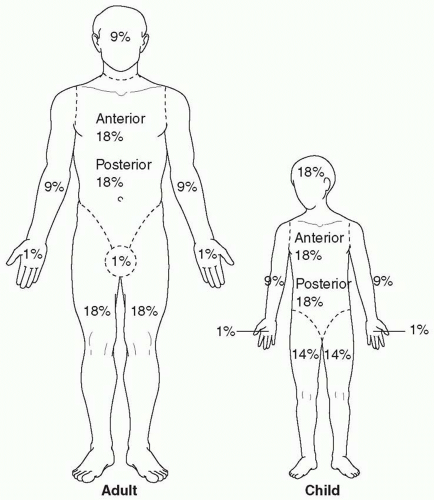
The choice of topical burn wound treatment is contingent on the depth of burn injury and the goals of management. Superficial burn wounds (such as sunburns) require soothing lotions that will expedite epithelial repair such as aloe vera. Partial thickness burn wounds need coverage with agents that will keep the wound moist and provide antimicrobial protection. Deeper partial thickness burn wounds should be covered with agents that will protect the eschar from microbial colonization. Once the eschar has lifted and the wound has begun to epithelialize, a dressing that optimizes epithelialization (i.e., greasy gauze and antibiotic ointment) is utilized. Full thickness burns are also covered with a topical agent that protects the burn wound from getting infected until the time of burn excision.
Prophylactic systemic antibiotics have no role in the management of burn wounds. In fact, the use of prophylactic
antibiotics has been shown to increase the risk of opportunistic infection.
1 Since burn eschar has no microcirculation, there is no mechanism for the delivery of systemically administered antibiotics. Therefore, topical agents need to provide broad-spectrum antimicrobial coverage at the site of colonization–the eschar.
In the early postburn period, the dominant colonizing organisms are staphylococci and streptococci–typical skin flora. Over time, however, the burn wound becomes colonized with gram-negative organisms. Thus, topical antimicrobial agents used in early burn care should have broad-spectrum coverage to minimize colonization of the wound, but they need not penetrate the burn eschar deeply.
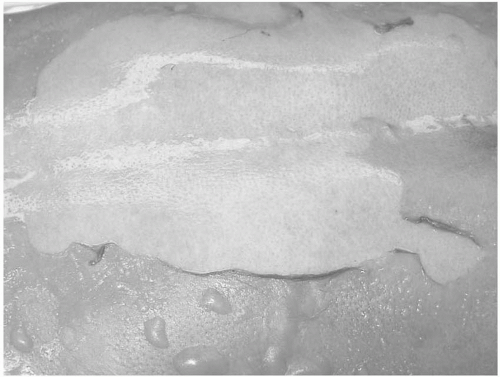
Silver sulfadiazine is the most commonly used topical antimicrobial agent. Silver sulfadiazine has broad-spectrum antimicrobial coverage, with excellent Staphylococcus and Streptococcus coverage. However, silver sulfadiazine is incapable of eschar penetration, so it is less useful in the management of the infected burn wound. Wounds treated with silver sulfadiazine will develop a yellowish-gray pseudoeschar that requires removal by cleansing during daily wound care. Traditionally, the principal drawback of silver sulfadiazine was thought to be leukopenia. However, it is not clear whether the leukopenia that occurs results from silver sulfadiazine toxicity or from the margination of leukocytes as part of the body’s systemic inflammatory response to the burn injury. Regardless, the leukopenia is typically self-limited, and therefore, the silver sulfadiazine should not be discontinued. Patients with a documented sulfa allergy may or may not have a reaction to the silver sulfadiazine. If there is concern about an allergy, a small test patch of silver sulfadiazine can be applied. Typically, if there is an allergy, the silver sulfadiazine will be irritating rather than soothing. In addition, a rash could signal a silver sulfadiazine allergy.
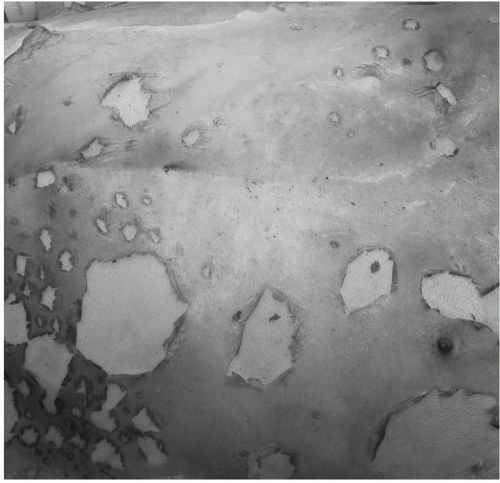
Mafenide (Sulfamylon) is another commonly used antimicrobial agent. Mafenide is available as a cream and, more recently, as a 5% solution. Mafenide, like silver sulfadiazine, has a broad antimicrobial spectrum, including gram-positive and gram-negative organisms. In addition, mafenide readily penetrates burn eschar, making it an excellent agent for treating burn wound infections. Mafenide is commonly used on the ears and the nose because of its ability to protect against suppurative chondritis; however, silver sulfadiazine appears to be equally effective in this setting. Since mafenide penetrates eschar well, twice-daily administration is typically necessary. Mafenide-soaked gauze can also be used as a dressing for skin grafts that have been placed over an infected or heavily colonized wound bed. There are two well-recognized drawbacks of mafenide. Mafenide is a potent carbonic anhydrase inhibitor and, therefore, can cause a metabolic acidosis. This problem can confound ventilator management. In addition, the application of mafenide can be painful and therefore its use may be limited in partial thickness burn wounds.
Silver nitrate is another commonly used topical antimicrobial agent. Silver nitrate provides broad-spectrum coverage against gram-positive and gram-negative organisms. It is relatively painless on administration and needs to be applied every 4 hours to keep the dressings moist. Silver nitrate has two principal drawbacks. First, it stains everything it touches black, including linen, floors, walls, and staff’s clothing. Second, since silver nitrate is prepared in water at a relatively hypotonic solution (0.5%), osmolar dilution can occur resulting in hyponatremia and hypochloremia. Therefore, frequent electrolyte monitoring is needed. Rarely, silver nitrate can cause methemoglobinemia. If this occurs silver nitrate should be discontinued.
Bacitracin, neomycin, and polymyxin B ointments are all commonly used for coverage of superficial wounds either alone or with petrolatum gauze to accelerate epithelialization. These ointments are also used routinely in the care of superficial face burns. Mupirocin (Bactroban) is another topical agent that is effective in treating methicillin-resistant Staphylococcus aureus (MRSA). Mupirocin should be used only when there is a culture-proven MRSA infection to avoid the development of resistant infections.