The Superior and Inferior Thyroid Artery Perforator (Stap) Flap
WARREN M. ROZEN
JEREMY L. WILSON
EDITORIAL COMMENT
A reliable pedicled flap in the head and neck region. Similar to the submental flap. The use of these flaps should be severely limited in patients with previous radiotherapy.
INDICATIONS
The superior and inferior thyroid artery perforator (STAP and ITAP) flaps can be used for a range of defects of the head and neck—we have used them for preauricular, postauricular, cheek, and perioral defects (1). They are suitable for harvest as free flaps.
ANATOMY
Published cadaveric injection studies have identified the external carotid and subclavian arteries as the main sources of blood supply to the anterior neck with a proposed watershed area between these territories running horizontally in the lower neck (2). The same studies have also suggested that there is little or no vascular communication across the midline. As a result of these findings, it has been suggested that anterior neck skin flaps should not be raised across the midline and should not incorporate the watershed area between the two parent vascular territories. This approach has limited the usefulness, size, and reach of anterior neck flaps. However, a recent description by Behan et al. (2010) of the cervicosubmental island flap brought into question the validity of these previous studies (3), with the skin of the anterior neck used with reliability.
In our anatomical studies, we have found a dominant thyroid artery perforator greater than 0.5 mm in diameter in every case (90/90 cases) on computed tomographic angiography (CTA) with a diameter range of 0.5 to 1.3 mm with a mean of 0.9 mm (Fig. 217.1). At least one such perforator was consistently shown to arise from its source vessel deep to the investing layer of deep cervical fascia, and to emerge from this layer at the anterior border of the sternocleidomastoid (SCM) muscle, at its caudocranial midpoint (within 2 cm of this point in all 90 cases). Other smaller thyroid artery perforators were shown to perforate the SCM. The dominant perforators arose from the superior thyroid artery (STA) in 89 of 90 cases and from the inferior thyroid artery (ITA) in 1 case. The dominant perforator consistently emerged between the investing layers of fascia forming the epimysium of the SCM, and traversed a variable subplatysmal course, before consistently perforating the platysma within the ipsilateral neck. After perforating the platysma, the STA perforator traversed an axial (transverse) subcutaneous course up to the midline, adjoining the axial
course of the STA perforator of the contralateral side of the neck. A long flap between the medial borders of each SCM could thus be planned as an axial pattern flap. These imaging findings have been confirmed operatively (Fig. 217.2).
course of the STA perforator of the contralateral side of the neck. A long flap between the medial borders of each SCM could thus be planned as an axial pattern flap. These imaging findings have been confirmed operatively (Fig. 217.2).
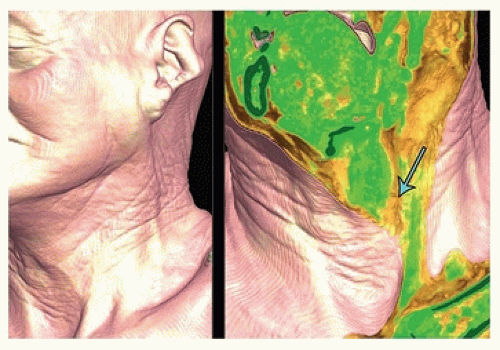 FIGURE 217.1 Preoperative computed tomographic angiogram of a patient undergoing periauricular reconstruction with a superior thyroid artery perforator (STAP) flap. Skin surface rendered view on the left, and cropped view demonstrating the STAP (arrow) on the right, with the perforator seen to emerge between the layers of the investing layer of fascia forming the epimysium of the SCM, and traverse a short subplatysmal course, before perforating the platysma within the ipsilateral neck and traversing an axial (transverse) subcutaneous course up to the midline, adjoining the axial course of the STAP of the contralateral side of the neck. (Reproduced with permission from Wilson JL, Rozen WM, Ross R, et al. The superior thyroid artery perforator flap: anatomical study and clinical series. Plast Reconstr Surg 2012;129(3):641-646.) |
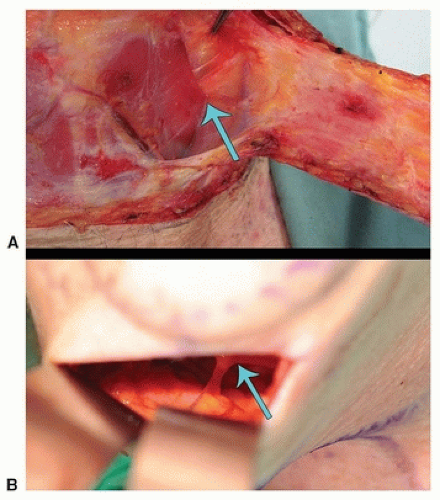 FIGURE 217.2 A: Intraoperative identification of the same superior thyroid artery perforator (STAP) as shown in Figure 217.2, confirming the position, course, and use of the axial course of this perforator as the vascular basis of the STAP flap. B: Another patient, undergoing a neck lift, with endoscopic identification of a STAP. Arrow depicts location of STAP. (Reproduced with permission from Wilson JL, Rozen WM, Ross R, et al. The superior thyroid artery perforator flap: anatomical study and clinical series. Plast Reconstr Surg 2012;129(3):641-646.)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





