Adolescents
Children
Gunshot wounds homicidal
Accidental gunshot injuries
Gunshot wounds suicidal
Gunshot wounds homicidal
Stab injuries usually with knives or similar
Penetrating stab injuries
Arrows and other missiles
Non-powder gun injuries
Blast injuries
Impalements
Younger children are typically the victims of accidental injury. Accidental weapon discharges can occur if children get unauthorized access to weapons, and hunting accidents are relatively common in rural areas with well-established firearm cultures. The inventiveness and curiosity of children (usually boys!) sometimes result in injury by a bizarre array of different missiles, explosives, and devices, sometimes of their own making. An accurate history of the injuring agent is essential to understand and treat the patient when they present.
In the United States, the evolution of the so-called school shootings has been a disturbing trend in recent times. In such cases, a shooter enters a school and inflicts multiple casualties on innocent and unprotected learners. Although well publicized, these scenarios are unusual but pose a formidable mass casualty challenge.
73.1 Resuscitation
Resuscitation should be performed in a swift and goal-oriented manner. One of the worst errors you can make is spending too much time with a bleeding patient in the emergency room and delaying operative hemostasis. In unstable patients, an airway should be secured, good venous access (Table 73.2) obtained by the quickest and simplest technique applicable, and resuscitation commenced. It is usually clear to an experienced surgeon that the patient is not responding to resuscitation, and the trip to the operating room should be undertaken without further delay. The patient must be kept warm, and packed red blood cells and other hematological products should be prepared for. The use of a balanced resuscitation approach with a 1:1 ratio of packed red cells and plasma is gaining momentum but still not proven to improve pediatric outcomes. The decision as to which body cavity or limb needs to be explored is usually clear after examination and initial resuscitation. Chest tubes can be placed with local anesthetic even in uncooperative children and should be used as resuscitative measures to avoid tension pneumothorax or hemothorax. Because of the thin anterior abdominal wall of most children, a large hemoperitoneum is usually clinically obvious. Trips to the computed tomography (CT) scanner are hazardous in this situation, and you will almost always regret them – rarely will you regret the absence of imaging information!
Table 73.2
Stepwise approach to venous access in a severely injured child
Stepwise approach to venous access in a severely injured child |
|---|
Peripheral IV with the largest size needle possible |
Long saphenous vein |
Cephalic or basilic veins |
External jugular vein |
Percutaneous central line by Seldinger stick |
Subclavian vein |
Internal jugular vein |
Femoral vein |
Intraosseous access |
Direct venous cutdown as a last resort |
73.2 Resuscitative Thoracotomy
The place of emergency department thoracotomy is an ongoing controversy in the management of the injured patient. I prefer to think of it as a resuscitative thoracotomy (RT), indicating its role as an adjunct to resuscitation when the patient does not respond to conventional resuscitation. Previously, children were assumed to have greater physiological reserve, and hence RT was applied liberally in an attempt to salvage desperate situations, but this usually failed or, even worse, produced survivors with neurologic compromise. Cumulative experience to date indicates that RT should be reserved for the following categories of pediatric patients after penetrating trauma:
- 1.
Penetrating thoracic injury with deterioration or poor response despite vigorous resuscitation
- 2.
Patients with penetrating thoracic injury who present with no signs of life to the emergency room but with a recently witnessed cardiac arrest
Under these circumstances, salvage rates of between 4 and 26 % can be expected, depending on the mechanism of injury and local circumstances. Children with penetrating abdominal injuries who do not respond to resuscitation should be transferred immediately to the operating room for laparotomy. It is my experience that children who receive a thoracotomy followed by laparotomy under these circumstances have a dismal prognosis and are best treated by laparotomy alone.
73.2.1 Technique
The technique is essentially the same as in the adult. The patient is positioned in the supine position with the selected side (usually left to facilitate direct cardiac massage) elevated on a bolster and the arm on that side elevated. After skin preparation, an incision is made with a cold knife as an anterolateral thoracotomy below the line of the nipple. The incision is carried through all layers, and the pleura is opened with a pair of scissors to avoid injury to the lung. A Finochietto retractor or rib spreader is placed. The pericardium is picked up between hemostats, taking care to avoid injury to the phrenic nerve and opened with a scissor if necessary to release tamponade or to allow internal cardiac massage. Aortic clamping is best achieved with a gently curved aortic clamp. Bleeding from hilar vessels can be controlled temporarily by the firm application of an angled vascular clamp. If it is necessary to cross the sternum and perform a clamshell incision to improve access to the heart or to enter the other side, this can be done quite easily in a child by using a pair of strong curved scissors or bone-cutting shears due to the incompletely calcified bone.
73.3 The Abdomen
Whereas one may sometimes deliberate over the decision of the best incision for abdominal access for other conditions, in penetrating trauma the answer is easy (even in small children) – the midline laparotomy (Fig. 73.1). This will give you the best access to the entire abdominal cavity including the aortic hiatus and pelvis; can be easily extended when you inevitably encounter the unexpected (into a sternotomy or thoracoabdominal incision); and heals in a durable and acceptable fashion. If necessary, you can leave the incision open in the context of abdominal compartment syndrome, leaving you the easiest closure later. Remember to prepare and drape the patient from the knees to the chin to allow access to the femoral vessels, neck, and chest if required. Make sure that the operating room is heated to at least 26–28 °C, and keep the patient warm with active warming devices. Mechanical retractors can make the difference between success and failure and should be available from the start. In cases of vigorous bleeding, autotransfusion appears to be a helpful adjunct to these patients’ care.


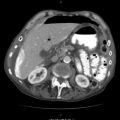
Fig. 73.1
Midline laparotomy gives you the best access to the child’s abdomen
In most cases, definitive surgery can be performed in children with penetrating abdominal injuries as they are less likely to develop a systemic inflammatory response syndrome (SIRS) or organ dysfunction than their similarly injured adult counterparts and will generally have the physiological reserves to tolerate the additional time on the operating table. In cases with an established coagulopathy and hypothermia, damage control techniques can be lifesaving.
73.3.1 Practical Advice and Pitfalls with the Abdomen
- 1.
Ensure you use an adequate-sized Foley catheter to allow for good drainage – not the smallest size available!
- 2.
When stomas are necessary, always ensure meticulous parastomal closure between the fascia and the bowel – the small bowel of a young child is like a puppy and can escape through the smallest defects!
- 3.
Drain as little as possible – only for anticipated bile, urine or pancreatic leak, and ongoing bleeding from parenchymal organs, not for bowel anastomoses.
- 4.
In most peoples’ hands and in most circumstances, bleeding from liver wounds is most safely treated by packing or by simple suture techniques (Fig. 73.2). Major liver resections in the context of hypovolemia are dangerous and usually unnecessary.

Fig. 73.2
In most peoples’ hands and in most circumstances, bleeding from liver wounds is most safely treated by packing or by simple suture techniques
- 5.
Splenic injury can be treated by salvage in many cases, but do not compromise the safety of your operation, particularly in an older child (>12) who will tolerate having their spleen out with a low risk of overwhelming infection.
- 6.
Non-expanding renal hematomas can be left alone. If you enter them, you will probably end up removing the kidney!
- 7.
Do the simplest operation to achieve your goal.
- 8.
Do not make two bowel anastomoses to preserve a short segment of bowel in a patient with normal length – resect it and do a single anastomosis.
- 9.
Close with continuous monofilament suture of adequate size (1 for adolescents, 0 for 7–12 years, 2/0 for 3–7 years, 3/0 for 0.5–3 years, and 4/0 for small infants and neonates).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree