THE MOUTH AND ORAL CARE
PART 3.6.1
THE MOUTH AND ORAL CARE
Authors
Roger Ellwood
Colgate-Palmolive Company
Director of Clinical Research for Europe
and
Scott Harper
(Author of Harry’s 8th Edition: Mouth and Oral Care)
ABSTRACT
While much of cosmetic chemistry and formulation is directed at maintaining or enhancing the appearance of the external surface of the body, the formulator of products for use in the human mouth must consider a more complex set of issues. Many oral care products address multiple consumer concerns at once, and it is common for an individual product to deliver both drug and cosmetic benefits. Understanding critical elements of oral biochemistry and microbiology will greatly help the formulator design products to deliver these benefits.
In addition to presenting some fundamentals of oral anatomy, physiology, and microbiology, this chapter will focus on the biology behind a variety of oral care consumer needs, the health and cosmetic problems behind these needs, and some approaches to solving these problems that can be introduced into oral care cosmetic or over-the-counter (OTC) drug products. Some of these concerns are summarized in Table 1.
3.6.1 The Teeth And Their Surroundings
a. Tooth Anatomy and Structure
b. Gingival Crevicular Fluid (GCF)
3.6.7 Major Oral Problems And Their Remedies Overview
c. Dental Caries (Tooth Decay)
e. Periodontal Diseases (Gingivitis And Periodontitis)
j. Aphthous Ulcers (Canker Sores)
3.6.1 THE TEETH AND THEIR SURROUNDINGS
The oral cavity contains the teeth, tongue, cheeks, palates, and gums (gingival tissues), and is bathed in saliva. The teeth and gums are major sources of consumer concerns, many of them related to dental plaque and other tooth deposits. However, oral care needs arise in other parts of the mouth as well. The following provides an overview of the biology of the oral cavity.
The normal human dentition consists of 20 primary (“baby”) teeth, which erupt from six months to four years of age, starting with the incisors, and are replaced by 32 secondary (adult) teeth, starting with incisors at about six years of age and culminating with the third molars (“wisdom teeth”), which erupt (in people who have them) around 20–21 years of age. Tooth makeup and form are influenced by genetics, the preeruptive environment (notably nutrition), and the posteruptive environment. Dental anatomy and alignment as well as individual oral care habits and salivary chemistry can have a profound effect upon the quantity, quality, and pathogenicity of the dental deposits that form on the teeth. Different parts of the tooth exhibit markedly different structure and characteristics, which make them prone to different types of problems.
Consumer needs | Underlying problems | Functional solutions |
| “Cosmetic” Indications |
|
• Attractive teeth/’’ bright smile” | • Dental stain/discoloration • Potentially unsightly dental deposits | • Tooth stain removal/prevention • Plaque/calculus reduction |
• Fresh breath | • Intrinsic/ extrinsic oral malodor | • Antimicrobial malodor prevention • Malodor masking/neutralization |
• Fresh/clean mouth feeling | • Food/microbial residues (?) | • Flavorants, astringents, remove dental deposits (?) |
• Clean mouth • Uncomfortable dental visits | • Dental plaque, calculus, stain • Uncomfortable dental cleaning to remove | • Plaque/calculus reduction • Stain reduction/prevention |
• Dry mouth | • Insufficient saliva flow or altered saliva composition | • Lubricating/moisturizing rinses or gels • Artificial salivas |
| “Drug” Indications |
|
• Healthy teeth/strong teeth | • Dental decay | • Decay prevention • Fluorides • Aid salivary function • Remineralization • Saliva stimulation • Plaque acid reduction |
• Healthy gums | • Gingivitis • Periodontitis (not an OTC indication) | • Plaque/gingivitis reduction and prevention |
• Sensitive teeth | • Exposed, hypersensitive dentin | • Tooth desensitization |
• Oral comfort | • Ulcers of the oral mucosa (e.g., canker sores) | • Topical anesthetics • Antimicrobial agents |
a. Tooth Anatomy and Structure
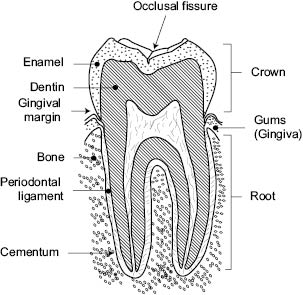
Figure 1. Simplified sketch of tooth anatomy
The tooth is divided into two areas: the crown (the enamel-covered part of the tooth that extends into the mouth) and the root, which is normally held firmly in place by the bone of the upper and lower jaws (Figure 1). Tooth crowns are covered by dense, hard dental enamel, the hardest tissue in the body. Enamel is thickest at the tip of the tooth and tapers to its thinnest point at the cemento-enamel junction (CEJ), where the crown gives way to the tooth root, which is covered by a thin mineralized layer called cementum. Underlying the enamel and cementum is a less dense mineralized tissue (dentin) that surrounds the dental pulp, which is rich in nerves and blood vessels.
In most individuals, the teeth are closely spaced and often touch side-to-side; the spaces between the teeth are referred to as interproximal spaces. The tooth roots are held firmly in place in the jaws through periodontal ligaments. In normal healthy teeth, the gums surround the teeth and come to an apex just above the CEJ, so that the roots are not exposed to the oral cavity. The physical shape of teeth varies with tooth type, from the chisel-shaped incisors to the blocky molars, which often have pits and fissures on their biting surfaces. As discussed later, tooth shape can have a profound effect on processes that can lead to various dental problems.
Dental enamel is composed mainly of a partially carbonated form of the calcium phosphate mineral hydroxyapatite [3Ca3(P04)2.Ca(OH)2], which accounts for about 98% of its composition. Minor amounts of collagen-like protein, remnants of the organic matrix mineralized during tooth development, also remain in the enamel structure. Hydroxyapatite is capable of ion exchange, and anions such as F– and CO32- may replace the OH– – group, while cations such as Zn2+, Sr2+, and Mg2+ may replace Ca2+. Caries susceptibility may be influenced by this ion exchange; for example, the extent to which OH has been replaced by F– has a protective effect on the vulnerability of the enamel to acid demineralization. The hydroxyapatite, of which enamel is largely composed, is present in the form of crystallites that make up rods oriented at right angles to the surface. Water and selected ions can penetrate a small distance into the dental enamel surface along the plane of the crystallites, which can facilitate ion exchange.
As with all calcium phosphate minerals, dental enamel is soluble in acid. A substantial body of data indicates that tooth mineral is highly stable above a pH level of approximately 5.5, referred to as the “critical pH,” and that tooth demineralization occurs when the pH falls below this critical level. The extent of enamel solubility is determined largely by the amount of acid present (measured as pH), the duration of exposure to acid, the amount of soluble calcium and phosphate ions in the fluid bathing the enamel, and the presence of other ions that influence the balance between mineral dissolution and crystallization. Thus the concept of “critical pH,” while useful, should not be considered to be an absolute value.
The layer of material beneath tooth enamel and cementum is the dentin. It contains approximately 70% hydroxyapatite, with the balance of its composition being collagen. Unlike the structure of enamel, which is characterized by densely packed crystals, the dentinal matrix is perforated by a number of tiny, fluid-filled canals (dentinal tubules) that radiate from the pulp cavity to the surface. Dentin can be exposed to the oral cavity through damage to the enamel or gingival recession and wearing of the cementum (the mineral layer covering the dentin of the tooth root). The presence of open dentinal tubules can lead to hypersensitivity, in which the exposed dentin may be painfully sensitive to various stimuli, including heat, cold, pressure, sugar, acid, and so forth. This is discussed in more detail later in this chapter.
Dentin, like enamel, is also acid-soluble. Because it has less mineral content, and possibly because its structure more readily permits penetration of bacteria and acid, exposed dentin is generally believed to be more susceptible to decay than enamel. This explains the rapid advancement of dental decay after it penetrates the enamel layer and the vulnerability of exposed tooth roots to decay.
The gums (gingival tissue) surround the teeth and overlie the bony structure in which the teeth are anchored. In health, the gum tissues directly adjacent to the teeth (the gingival margin) are firm and pink, extend just above the CEJ, and form a crevice that is not more than 3 mm deep. If dental plaque is permitted to accumulate adjacent to the gingival margin and within the gingival crevice, the gum tissue can become irritated, inflamed, and liable to bleeding. In some cases this inflammatory state stabilizes as chronic gingivitis, while in other cases the inflammation can advance to the destructive disease periodontitis.
Saliva is a major factor in the maintenance of a healthy mouth. Saliva is continuously being produced, bathing teeth and oral tissues in a dynamic environment that serves to lubricate the mouth, remove harmful materials from the oral environment, and maintain the mineral balance of the teeth.
Saliva is produced by three pairs of major glands and the smaller glands of the oral mucosa (labial, lingual, buccal, and palatal). The secretions differ from one another in composition and may also differ according to the rate of flow, time of day, and so forth. For instance, it is well known that salivary flow is reduced at night; this makes it extremely important to cleanse the teeth between that previous midnight snack and going to bed, as the protective effects of saliva are substantially reduced during sleep.
Saliva contains mucopolysaccharides, proteins, enzymes, and inorganic materials such as calcium, sodium, potassium, chloride, bicarbonate, and phosphate ions, and bacteria shed from the oral surfaces and a variety of their constituents. The organic constituents of saliva are thought to be responsible for the development of the acquired dental pellicle (as described later). The presence of calcium and phosphate ions and the bicarbonate buffer system are believed to be significant both in the control of dental caries and in calculus formation. The pH of resting saliva ranges from about 6.5–7.2, while that of stimulated saliva can range up to about 8.0; the pH increase reflects a higher bicarbonate content in simulated supply.
The importance of saliva in preventing tooth decay following eating was demonstrated in the 1940s by R.M. Stephan. He devised a miniature pH electrode from antimony and used it to determine the pH of dental plaque at various sites on the teeth. His experiments showed that the pH of dental plaque decreased rapidly from about pH 6.82 to about pH 5 within a few minutes after consuming a sugar challenge and slowly returned toward neutrality over the next 20 to 60 minutes. If saliva flow to the teeth was restricted, the pH would remain depressed below the critical pH for enamel demineralization for much longer periods. The importance of saliva in maintaining oral pH may partially explain why an inadequate flow of saliva resulting from head and neck irradiation, drug-induced hyposalivation, or pathology can result in increased caries susceptibility and other oral problems.
b. Gingival Crevicular Fluid (GCF)
GCF exudes from the epithelium within the gingival sulcus or pocket. It is more similar to blood plasma than to saliva and can serve as a source of nutrients to the bacteria growing within the sulcus and along the gingival margin; it can also carry a variety of specific and nonspecific host defense factors.
The oral soft tissues consist of the tongue, gums, cheeks, hard and soft palate, and sublingual region. The oral soft tissues are covered by a variety of nonkeratinized and keratinized epithelia. The surface of the soft tissues, most notably the tongue, can harbor large populations of oral bacteria that can serve as a reservoir to recolonize the teeth after cleaning. The microbial flora of the tongue can also play a prominent role in the generation of oral malodor (bad breath). Additionally, certain oral soft tissues are prone in some individuals to develop painful sores or ulcers, for example, aphthous ulcers (canker sores), which are addressed at greater depth later in this chapter.
As soon as a tooth erupts into the mouth, and subsequently after every cleaning, it is prone to coverage with a variety of dental deposits that can cause diverse conditions that concern consumers. The enamel of a freshly cleaned tooth is rapidly covered by a pellicle of proteins adsorbed from saliva, followed by salivary bacteria that form dental plaque. Dental plaque bacteria can, under certain conditions, release by-products that can be harmful to the teeth or gums. Dental pellicle and plaque are also liable to accumulation of stain and neutralized deposits (dental calculus or tartar).
Immediately after cleaning, the enamel surface is covered very rapidly by a 1–3 µm thick film of proline-rich phosphoproteins, peptides, and glycoproteins adsorbed from the saliva; thus the presence of a truly “clean” enamel surface in the oral environment is a fleeting phenomenon. The adsorption of salivary peptides and proteins appears to be relatively specific, starting within minutes of a tooth cleaning and continuing for several hours. While the acquired enamel pellicle is free from bacteria, it has been shown to contain a variety of bacterial constituents including enzymes such as glucosyltransferase, soluble polysaccharides, and various bacterial cell wall constituents.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








