CHAPTER 14 The male facelift
History
Facial rejuvenation in the male patient can be particularly challenging for a variety of plainly apparent reasons: men don’t wear makeup, they eschew any possibility of an over-operated appearance, and the hairline and beard cause many differences in terms of operative strategies (see Table 14.1). In a world that equates youthful appearance with fresh, new ideas, the patient population now encompasses men who want to stay busy in a very competitive environment rather than for vanity. They may be in business, acting, television, even politics. Growing social acceptability of aesthetic techniques has added to this demand.
Table 14.1 Special challenges of male facial rejuvenation
The technical and aesthetic goals of the male facelift (Tables 14.2A and 14.2B) share similar principles as for the female: dissection in skin and sub-SMAS layers, repositioning of the SMAS and supra-SMAS fat to restore volume in a vertical vector, avoiding a lateral pull, and redraping of the skin in a natural way. It is, however, absolutely essential that the surgeon understands important differences between the male and female patient and also has a commanding knowledge of the male anatomy and techniques to achieve these goals in a naturally appearing way.
Table 14.2A General aesthetic goals for male facial rejuvenation
Table 14.2B Immediate surgical goals for male facial rejuvenation
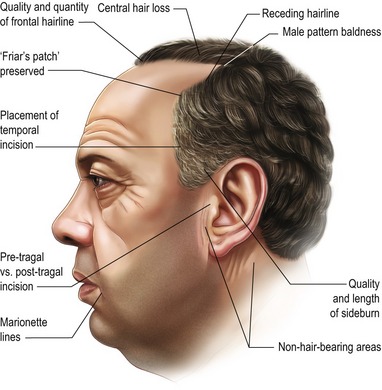
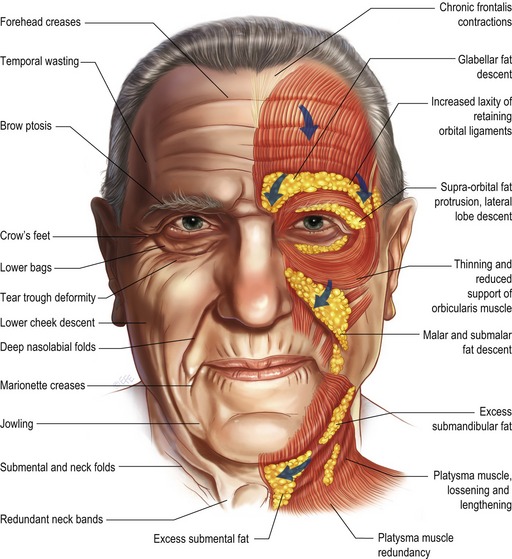
The process of facial aging represents a combination of gravitational effects, atrophy, and sun damage yielding the characteristic changes shown in Figs 14.1 and 14.2. This chapter will review the process of facial aging, the relevant surgical anatomy, and the common male facelift techniques.
Physical evaluation
Preoperative counseling
The classic “SIMON” patient described in the plastic surgery literature (see Table 14.3) should be avoided as well as patients with body dysmorphic disorder. These patients can be easily recognized, screened and referred for psychiatric evaluation.
Technical steps
Preoperative management
0.1–0.2 mg of clonidine is administered to the hypertensive patient at least 45 minutes prior to the procedure. Ten minutes before, the patient is also infused with local tumescent fluid (0.5% lidocaine, 1 : 200,000 epinephrine) bilaterally. These two steps will help blood pressure control intra- and postoperatively. It is especially important to maintain a dry intra-operative field as the hypervascularity of the male follicular skin contributes to the increased incidence of hematoma formation.
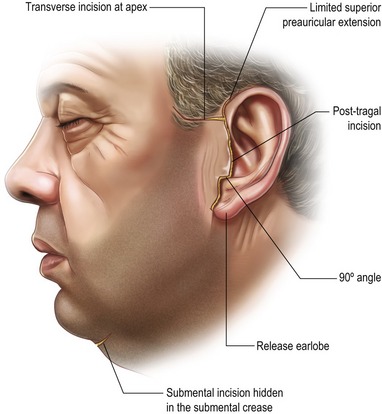
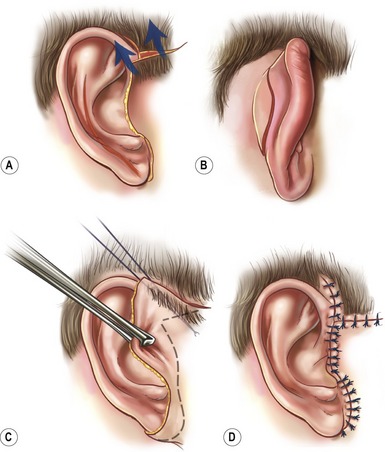
The incision options for the male facelift are illustrated in Fig. 14.3. The preauricular hairline incision chosen depends on the amount of skin laxity, skin quality, and previous incisions. The incision is initiated a short distance anterior and superior to the root of the helix in the temporal scalp, may extend transversely into the sideburn, and if necessary, sparingly follows the anterior temporal hairline (see Fig. 14.4). As discussed previously, the preauricular incision then proceeds caudally in the pre-tragal region if there is a natural skin crease and very little sun damage. The scalpel should bevel in line with the hair shaft. Alternatively, a post-tragal incision with defatting and follicular cauterization is performed. For the short-scar facelift, the incision passes beneath the earlobe and extends into the retroauricular sulcus staying 2 mm on the concha, so any scar migration that may occur will pull the scar no farther than into the sulcus. If there is severe laxity of the neck skin, the incision then traverses the hairless skin in the retroauricular region for 3–5 mm at a point which is superior enough in this region to be hidden if the patient opts for short hair. The final result should not be compromised simply to rigidly commit to a shorter retroauricular incision. If there is too much cervical laxity, the surgeon must extend the incision into the hair. Going into the retroauricular scalp with a sigmoid curve, instead of the occipital hairline incision, is preferred as men tend to retain their hair growth in this region and it allows the patient to have closely cropped hair without a visible incision.