In this article, we explore the nuances of dorsal preservation (DP) rhinoplasty, a technique that has seen resurgence in popularity in recent years. We discuss the importance of careful patient selection, as DP is not suitable for all nasal types. Our preferred technique, the high septal strip approach, allows for precise lowering of the nasal dorsum while maintaining the natural contour, minimizing tissue damage, and enhancing long-term outcomes. We emphasize the critical role of meticulous surgical execution and postoperative care in achieving optimal results.
Key points
- •
Renewed interest in dorsal preservation (DP): DP techniques in rhinoplasty have gained increased attention, with renewed focus on training programs incorporating this method. Most current practitioners have self-taught the techniques due to limited formal training.
- •
Patient selection crucial: Proper patient selection is essential to prevent complications in DP rhinoplasty. The less resection and dissection performed, the better the long-term outcomes due to reduced soft tissue damage.
- •
High septal strip technique: This technique involves resecting the most dorsal part of the septum to lower the dorsum while preserving its shape. It allows for fine adjustments in height and contour of the nasal structure.
- •
Surgical execution and postoperative care: Successful outcomes in DP depend on careful execution of the surgery, managing patient expectations, and diligent postoperative care. Techniques such as fixation of the neodorsum help ensure stability and reduce the risk of complications like recurrence or saddling.
- •
Long-term benefits and satisfaction: DP has shown fewer adverse outcomes, higher patient satisfaction, and easier revision surgeries compared to traditional rhinoplasty, making it a preferred approach for suitable cases.
Overview
Although DP ( Dorsal preservation ) in rhinoplasty is not a new concept, there has been renewed interest in this approach and technique since Saban’s 2018 article, Dorsal Preservation: The Push Down Technique Reassessed. There is a growing trend in training programs to incorporate official didactics in preservation rhinoplasty (PR). However, presently that the majority of rhinoplasty surgeons performing DP have acquired their skills through self-teaching, or limited mini-fellowships while the majority of formal residency and fellowship training programs still primarily focus on structural rhinoplasty.
The exponential increase in both the level of interest and rapid advancements in DP techniques, along with the limited availability of standardized training programs, has inevitably resulted in a certain state of ambiguity about terminology, indications, patient selection criteria, technique selection, and the decision-making process for clinical and surgical interventions among rhinoplasty surgeons.
DP is not suitable for all types of noses. Patient selection is crucial for preventing complications. However, when discussing long-term outcomes, it is logically deducible that the less resection and dissection performed, the less damage to soft tissues and subsequent fibrosis and distortion, positively contributing to improved long-term outcomes.
Important indicators of success in DP include: (1) in-depth understanding and candid management of patient expectations; (2) accurate dorsal and nasal analysis; (3) appropriate choice of surgical technique; (4) meticulous surgical execution; and (5) careful postoperative management.
The objective of DP is to reduce the height and convexity of the dorsum while preserving the Keystone Area, which holds significant anatomic and functional importance. While acknowledging the potential for oversimplification, it is conceptually feasible to draw comparisons between this notion and established techniques employed in architectural engineering for the purpose of building demolition. The concept of DP can be compared to the architectural technique known as the Kajima Cut and Takedown Method, which is employed to demolish tall buildings from the bottom up, minimizing noise and dust pollution.
The superior strip technique (also knowns as the “high septal strip” and “sub-dorsal septal strip”) refers to resection of the most dorsal segment of the cartilaginous septum and allows for incremental adjustment to its height. This can be accomplished by resecting a predetermined segment of sub-dorsal septum just beneath the dorsum, thereby creating space for the dorsum to descend into. The intact septum left in place (the median pillar structure) will determine the dorsal shape and height. It is important to note that our goal is often to lower and flatten the dorsum. Since the K-area functions as a semi-mobile joint, flattening or even curving of the bony cartilaginous dorsum is possible.
Complete osteotomies are employed to fully separate the nose from the face and the cranium, allowing for full mobilization of the bony-cartilaginous pyramid and control dorsal height reduction. This article will discuss nasal hump reduction with DP using sub-dorsal septal strip resection and push/let-down techniques (PDO/LDO).
We have previously published our data on the long-term results of DP rhinoplasty, which objectively demonstrated fewer adverse outcomes in DP rhinoplasty compared to structural rhinoplasty. Our data further show as high long-term patient and surgeon satisfaction with a lower revision rate compared to classical rhinoplasty. In addition, the abundance of septal cartilage available in DP and the natural anatomy maintained during the primary surgery, make revisional surgery easier and safer than in structural rhinoplasty.
In this article, we discuss the authors’ preferred DP technique, the high septal strip impaction. It is our aim to additionally discuss the indications, advantages, and disadvantages of this technique in order to provide a strong foundation for technique selection depending on various nasal pathologies and deformities.
Preoperative Assessment
In addition to the ever-important psychologic evaluation of the patient and their reasons for desiring rhinoplasty, the surgeon must categorize the “nose type” in order to select the appropriate surgical technique.
In DP cases, it is crucial to preoperatively assess the nasal dorsum by examining its size, shape, and orientation externally and palpating its cartilaginous and bony elements. The rhinoplasty surgeon needs to determine, ‘Is it possible to maintain the dorsum intact?’ Often, the conclusion is that the dorsum has a natural appearance and is preserveable.
Furthermore, a more cartilaginous dorsum makes a stronger case for preservation methods. Diagnosing deviations and asymmetries preoperatively is crucial for choosing the appropriate septoplasty and osteotomy methods. An in-depth examination of the nostrils focuses on their size, orientation, and aesthetic markers. In tension noses, the nostrils are slim with excessive height, while the nasal lobule seems shorter. After employing impaction methods for dorsal lowering, the nostrils might widen and the internal nasal valves expand. At times, these outcomes are anticipated and preferred, but if overdone, a concluding alar base reduction is necessary.
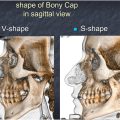
DP works better in V-shaped nasal bones than in S-shaped bones.
Without additional contouring maneuvers, S-shaped noses are more likely to develop an osseous residual hump.
Previously, we published the guidelines for dorsum preservation in primary rhinoplasties, where we classified approaches based on the nose type summarized as follows:
Type 1 (straight noses) PR: complete preservation of the dorsum without any dissection of the soft tissue envelope;
Type 2 (tension noses) PR: DP with bony cartilaginous resurfacing;
Type 3 (kyphotic humpy noses) PR: Cartilaginous-only preservation with bony-cartilaginous disarticulation and push-down of the cartilaginous vault.
In the event of a severely deviated and unstable septum, the Cottle procedure or its modifications or structural techniques must be considered.
Briefly, Type 1 PR is mainly applied to straight noses. The procedure is less traumatic and allows dorsum lowering. Type 2 PR is indicated when bony cap resurfacing or resection is needed, that is, for patients with minor bony bumps, S-shaped nasal bones, patient with tension nose deformity and aesthetically pleasing dorsal lines. Either the sub-superficial musculoaponeurotic system (SMAS) or subperichondrial/subperiosteal plane is utilized for skin and soft tissue elevation. The nasal bones are then reshaped (using a rasp or osteotome), and the superior bony margins are smoothed.
Type 3 PR is indicated for individuals with humpy and kyphotic nasal deformities that necessitate the use of disarticulation procedures. The surgical procedure includes the removal of a bony hump in conjunction with the K-A cartilaginous push-down technique.
Technique
For the sake of clarity, we have divided our approach into 10 steps, which we will outline as follows in sequential order.
Step 1: Approach to the Dorsum and High Septum
Reduction rhinoplasty and DP often necessitate the exposure of the caudal and dorsal septum, unless the nose is straight (Type 1), in which case dorsal undermining can be avoided. The procedure is commonly carried out via an endonasal inter-septum-columella route, a standard technique in septoplasty, without any lateral intercartilaginous extension.
The septal incision involves the mucoperichondrium along the caudal septum up to the anterior septal angle. Next, bilateral septal superior tunnels, very similar to the L-strut shape septoplasty procedure, in a limited submucoperichondrial dissection, along the dorsal cartilaginous septum toward the radix is performed and the W-point is identified and preserved. There is no need to elevate the mucoperichondrium off the entire cartilaginous septal framework. If the perpendicular plate of the ethmoid (PPE) is long, requiring excision in the area corresponding to the dorsal convexity, submucoperiosteal dissection over the anterosuperior angle of the perpendicular plate of the ethmoid bone is needed.
Step 2: Septal Incision
The septum is incised just below the dorsum, so as not to leave any remnant of the upper cartilaginous septum under the K-area, which could result in a “coat-hanger effect.” This section must begin where the cartilaginous septum and upper lateral cartilages (ULCs) diverge, at the W-point. The dorsal septal area supporting the supratip region, extending from the anterior septal angle cephalically for about 10 mm, termed the W-ASA segment, must be left intact at this point in the procedure.
The division of the cartilaginous septum below the dorsum will continue until the bony junction of the PPE, easily felt through the bony contact at the tip of the instrument. Then, if needed, using a 2 mm bone rongeur, the ethmoid perpendicular plate anterior bony angle will be resected incrementally up to the radix region. This maneuver is only necessary if the PPE blocks the descent. It is crucial to always verify the position of the instrument’s tip when approaching the radix or base of the cranium to prevent cribriform plate mobilization.
To verify that the division has been completed, an elevator is positioned in the left superior septal tunnel beneath the K-area and moved horizontally along the dorsal vault to the contralateral superior tunnel. This movement must be unimpeded. If not, the residual bridge must be excised. At this point, the septum and dorsum are no longer interconnected.
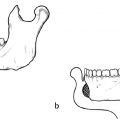
Step 3: Excision of the Septal Strip
Using fine scissors, a second cartilaginous incision will be made, almost parallel to the first, starting at the W-point, and ending at the bony contact in depth, from anterior to posterior. This cartilaginous strip incision will stop at the junction of the perpendicular plate of the ethmoid. At this point, the cartilaginous strip will be disarticulated from the PPE. The cartilaginous portion is then extracted, with relative ease. This first strip will typically be 3 mm in height and almost 30 mm length following a grossly triangular shape. This cartilaginous segment is preserved in saline for future use as a graft, if necessary.
Using a delicate bone rongeur or Caplan scissors, the superior anterior angle of the perpendicular plate of the ethmoid (called the E-point, E for ethmoid) can be removed, with high precision and soft hands, just under the nasal bones.
Step 4: Complete Mobilization of the Nasal Pyramid
Lateral, transverse, and radix osteotomies are necessary to render the bony pyramid wholly mobile and detached from the craniofacial skeleton. Typically, the choice of technique is determined by the surgeon preference . The following is a brief overview of these osteotomy techniques:
Lateral osteotomy
A vestibular incision is made by using a monopolar cautery or a Colorado to avoid any bleeding, in front of the head of the inferior turbinate at the skin/mucosa junction. Endonasal osteotomies may be performed using sharp, straight guarded osteotomes. Alternatively, ultrasonic or power instruments may be utilized. The choice of how high or low the osteotomy must be will depend on the patient’s lateral bony anatomy, skin thickness, and hump size. The osteotomy is generally carried up to the level of the medial canthus with care not to cause injury to the ligaments. Our preferred site for lateral osteotomy is the naso-facial groove, to avoid visible or palpable bony steps or extra width remaining at the base of the lateral wall. The osteotomy will be carried out till touching the frontal bone, sounding harder.
When the nasal pyramid needs to be lowered by more than 4 mm, the LDO is preferred. This involves removing a triangular bone wedge from the frontal processes of the maxilla. This removal should be executed low and laterally in the nasofacial groove to prevent detectable or tactile irregularities. An endonasal method is employed. Periosteal undermining is performed on the internal and external bony sides, to ease the bony wedge resection.
For the lateral osteotomy, the osteotome’s tip should be perpendicular to the lateral bony wall. Ensuring a genuine vertical cut may be crucial as it enhances the sliding of bony surfaces and aids the push-down procedure, decreasing the likelihood of over-narrowing the base.
Radix osteotomy
The triangular bony extension of the frontal bone that slides under the nasal bones has been referred to by a number of names, including the nasal spine of the frontal bone, the nasal process of the frontal bone, and the internal nasal spine (spina nasalis interna). Radix osteotomy entails bone cuts in the nasal bones and this bony process, which is particularly resistant and provides the most resilient point of the nasal framework.
Radix and transverse osteotomies have a tendency to bleed. As such as we recommend reinjection with 1% lidocaine with 1:80,000 epinephrine, placing the patient in reverse Trendelenburg position and icing before and after the osteotomies. For better control, we also recommend the assistant to hold the patient’s head immobile and for the surgeon to handle the mallet to perform the osteotomy for more precise control.
The osteotomy of the radix may be approached either internally or externally; a direct approach may also be used if the soft tissue has been elevated off the dorsum. This can be accomplished by the use of 2 mm osteotomes, piezoelectric system, or a radix saw. The preponderance of our cases is performed via an external approach with a 2 mm stab incision by a #11 blade and the use of 2 mm osteotome. Prior to performing the osteotomy, the #11 blade is moved from side to side, using skin elasticity to avoid a bigger scar, through the incision to score the periosteum over the radix, and the planned transverse osteotomy.
The orientation of the osteotome at the radix bears discussion. Although many author caution of the proximity of the skull base in this maneuver, Saman and colleagues (unpublished data as of yet) in a radiographic analysis of 100 heads have demonstrated that even at the most cephalic portion of the radix with a perpendicular osteotomy, the mean distance from the most anterior portion of the skull base is nearly 12 mm, which a minimum of 9 mm distance. Nonetheless, an oblique osteotomy slightly more caudally (at the area just before the start of the dorsal convexity) has important advantages. Firstly, this is theoretically safer as it is directed away from the skull base. Secondly, the oblique orientation of the bone cut prevents excessive radix lowering by creating a hinge that allows the radix to slide down but not drop excessively. Finally, it is advantageous in minimizing the bony step off at the location of the osteotomy.
Transverse osteotomy
Transverse osteotomies connect the radix osteotomy to the lateral osteotomies, thereby freeing the nasal skeleton from craniofacial attachments. Transverse osteotomies can be achieved using delicate osteotomes via the radix percutaneous incision or via external stab incisions at mid-distance between sellion and inner canthus after marking the angular vein to prevent from bleeding. If done percutaneously, it is worth to perform a few bony sections from low to high and vice-versa to ensure complete osteotomy. At the completion of this maneuver, the nasal bones are ready for mobilization.
Bony mobilization
The initial motion is horizontal mobilization. Care must be taken not to fracture inward the sidewalls and to separate the bony subunits, following excessive inward pressure on bony sidewalls. The skeletal pyramid is moved horizontally to the right and left sides with no pinching or vertical forcing of the bones. If mobilization is not completed, surgeons will sense a bony bridge obstructing this free lateralization. Then, the osteotomies must be redone until the complete liberation of the bony pyramid is attained. This mobilization must not be forced, as this could result in undesirable fractures and make it impossible to accurately manipulate the nasal pyramid. If lateral osteotomies were previously performed percutaneously, it may be advantageous to conduct them again via an endonasal approach.
The second motion is squeezing and lowering as to make the nasal bones fit into the pyriform. This pinching and lowering maneuver is performed with both hands; one hand pinches while the other gingerly pushes downward.
At this juncture, the dorsum is examined in terms of height and convexity. In case of a residual hump, a spring effect must be eliminated by means of the Ballerina maneuver at the lateral keystone blockage to allow for opening of the joint; one must also ensure adequate resurfacing of the bony cap in S-shaped nasal bones has been performed.
In cases of resistance to lowering of the dorsum, the coat hanger effect must be considered, which refers to the excess subdorsal cartilage at the flexion area. One must also ensure that the mucosa under the nasal bones does not provide resistance to lowering. If the dorsum still needs to be lowered after these areas have been examined, incremental superior septal excisions can be performed under direct vision to create more space under the keystone area so that the dorsum can descend into that space. To facilitate this step, the cartilaginous vault can be lifted by introducing an elevator under the vaults, allowing for visualization of the entire superior septum, and direct and precise strip excision. The removed cartilaginous segments can be saved for use for any necessary further grafting as needed.
Considering the anterior septal pillar supporting the supratip area, this free dorsal portion (W-ASA segment) of the septum should have been left undisturbed until the very end of the preceding stages, as strip removal should begin at the W-point. This W-ASA anterior septum pillar can function as an autoseptal extension graft as it is fixed to the anterior septum and can be used for additional fixation in tip procedures for cephalic rotation, or it can be removed flush with the descended septum and neodorsum and used for grafting if needed.
Neodorsum fixation
To prevent any postoperative issues, such as lateralization, deviation, or hump recurrence, it is advantageous to fixate the neodorsum to the stable untouched septum. In some cases, a direct fixation of the neodorsum to the intact septum and W-ASA is recommended; a transosseous suture can be performed as well, especially easier in the open approach. In endonasal cases, to perform such a cerclage suture, we perform a 2 or 3 levels cerclage sutures linking the cartilaginous vault to the remaining septum. The upper one is done on the rhinion; the lowest one is done endonasally at the W-point. Another suture can be done in between the Rhinion cerclage and the W-cerclage sutures. To perform the upper cerclage sutures, we utilize the percutaneous suture technique as described by Dogan. In this technique, a 5-0 PDS suture is passed endonasally through the intact septum and retrieved on the contralateral side. A 22-gauge hypodermic needle is then introduced percutaneously over the septum, passed through the junction of the dorsal septum and the ULC on the same side as the septal suture introduction. The end of the suture is then threaded through the needle and captured as it comes out of the end of the hypodermic needle. The needle is retracted carefully without being brought out of the nasal skin, nor catching the dermis. The needle tip is mobilized subdermally to the contralateral septal-upper lateral junction and brought out into the opposite nasal airway. The suture is then pulled from the needle, and the hypodermic needle is removed. This, in essence, creates a loop around the neodorsum, which is next tied down to the intact septum, thereby securing it in place. We prefer placing a minimum of 3 percutaneous sutures to ensure sturdy fixation.
Sutures, dressing, and immediate postoperative period
Infusion of tranexamic acid in the osteotomy sites has been shown in our experience (article to be published) to significantly reduce the immediate postoperative swelling and bruising (from 3/5–1/5). Generally, these infusions of pure tranexamic acid (5 cc) are done immediately after the lateral osteotomies are completed and before the final closures.
Sutures
The aim of the sutures is not only to close the skin but also to close the dead spaces created by the subperichondrial undermining. A few Vicryl Rapid 5-0 sutures are placed on the vestibular approach. One is done under the plica nasi to close the upper dead space below the ULC. It is important to avoid catching the cartilage or the external dermis to avoid granulomas or distortions. In open approach, the columellar incision is closed with a series of interrupted 6-0 fast absorbing gut sutures.
Dressing
- •
Internal dressing: In cases of minimal septal manipulation, transseptal sutures to close dead space are sufficient. If signficant elevation of the mucoperichondreal flaps has occurred, or additional functional (IT reduction, sinus surgery, etc) maneuvers have been performed, silicone internal nasal splints are placed and kept in place for 1 w.
- •
External dressing: With the use of external dressings, we aim to stabilize the bony cartilaginous pyramid in the proper position, to control the tip position, and to reduce the deadspace and swelling. Further, the idea dressing must be stable yet easy to remove without pulling up on the nose. To achieve these goals, a non-adhesive dressing is placed over the dorsum; then steri-strips are applied firmly over the non-adhesive dressing as to push the nose inward, that is, perpendicular to the face. A rigid cast is fixated over the nose in a stable fashion that is removed 8 to 10 d postoperative.
Post-Operation Recommendations
In post-rhinoplasty care, patients should be informed to avoid actions that increase intranasal pressure, such as Valsalva maneuvers and forceful nose blowing. They should also follow standard instructions, including avoiding strenuous activity, not sneezing through the nose, keeping the head elevated while sleeping, and practicing caution when sneezing to minimize the risk of bleeding, swelling, and ecchymosis.
Local cleaning involves the use of hydrogen peroxide and ointment gently applied with a cotton tip applicator to incisions only. Patients should refrain from inserting any objects into the nose or attempting to remove the nasal cast for cleaning or shape assessment. To alleviate swelling, a regimen of oral Prednisolone at a dosage of 40 mg or higher for a duration of 5 d or more is prescribed, along with phenylephrine to aid with nasal decongestion.
Post-Operation Visit
Whenever possible, it is better to see the patient on postoperative days 4 and 8. Early postoperation is useful for cleaning the nose, checking the patient status, and reviewing postoperative instruction. On day 8, patient returns for cast removal (and splint if placed) and to answer any questions patient may have.
Complications in dorsal preservation
Functional Concerns
Not every undesirable rhinoplasty outcome necessitates revisional surgery. The majority of these concerns can be managed with time and prudent management. Therefore, it is beneficial to evaluate these concerns over time and not rush to aggressive intervention. Here, we will briefly discuss some of the transient and long-term possible complications of dorsal preservation.
Nasal obstruction is the most common early functional finding following nasal surgery. Early nasal obstruction is typically caused by nasal and turbinate mucosal edema and typically resolves on its own within 3 mo; however, in certain cases, intranasal corticosteroids or vasoconstrictors may expedite the recovery. Although nasal obstruction caused by turbinate hypertrophy in the early postoperative phase may be edematous and temporary, persistent turbinate hypertrophy due to bony or mucosal redundancy may necessitate surgical inferior turbinoplasty.
Early postoperative internal edema may also contribute to the transient olfactory disturbances following rhinoplasty; however, we hypothetise that persistent anosmia or hyposmia may be caused by septal or osseous maneuvers that directly or indirectly harm the cribriform area. We have previously presented cases in which patients complained of chronic anosmia without any clinical or radiographic evidence of cranial base or cribriform injury.
Stenorhinia, or an abnormally narrow pyriform aperture, has been identified in less than 3% of our preoperative patients. We urge that patients suspected of stenorhinia (clinically or by computed tomography) be evaluated and counseled about the finding, even in the absence of preoperative nasal obstruction, as modified preoperative planning and surgical maneuvers may be necessary to prevent postoperative obstructive symptoms. It is imperative to note that the push-down procedure, if done properly, does not cause pyriform narrowing any more than traditional nasal bone fractures.
Aesthetic complications
The most important indicators of success in DP are: (1) a thorough understanding and candid management of patient expectations, (2) accurate dorsal and nasal analysis, (3) appropriate surgical technique selection according to published guidelines, (4) meticulous surgical execution, and (5) careful postoperative management. It is crucial to inform the patient of the importance of postoperative appointments to allow for managing unpredictable deformity in a timely fashion.
As with any aesthetic intervention, it is essential that we have an open dialogue with our patients regarding their expectations and desired aesthetic outcomes. It is essential that the patient be requested to articulate, in order of importance, their aesthetic concerns and expectations. During the visit, the patient is always asked to provide the top 3 priorities and expectations to customize the surgical steps. As surgeons, we must be forthright when discussing realistic expectations, the healing trajectory and timeline, the significance of following postoperative instructions, and the possibility of postoperative complications that may or may not require intervention.
While the ideal outcome of rhinoplasty is to successfully address both aesthetic and functional objectives in a single surgical procedure, it is crucial to inform patients about the potential need for additional surgery in cases of complications or unsatisfactory results. Even with the most skilled surgeons, unforeseen healing processes and fibrosis can lead to undesirable outcomes, ranging from minor concerns to more significant complications.
To give objective information, and to involve the patient in the success of the rhinoplasty procedure, we generally inform the patient that approximately 80% of the issue is related to the surgery but 20% are directly related to the patient’s specific healing, which encompasses their genetic, environment, nutritional, and postoperative care factors. Therefore, it is vital that patients understand that they are a team with the surgeon with the common objective of improving their aesthetic (and function.) In this era of social media and unattainable “perfection” standards, it is imperative that our patients set a realistic objective of substantial “improvement” rather than unattainable “perfection.” Naturally, a psychologic evaluation of the patient is necessary prior to surgical intervention in order to determine motivations and expectations and to rule out concerns such as Body Dysmorphic Disorder.
Aesthetic concerns, like functional concerns, are best evaluated over the time continuum, given the healing changes that occur with time. Targeted dilute triamcinolone injections followed by short-term taping may be used to treat the resulting inflammatory reaction. For example, periosteal and/or perichondrial fibrotic reactions or callus-like healing processes may cause a pseudohump in the early phases, especially if the dorsum is exposed for resurfacing. Diluted triamcinolone (10 mg/mL) injections can be used to treat these convexities. Likewise, fullness in the tip/supratip may be addressed in the early postoperative period in the same manner.
Another transitory postoperative concern may be small patches of dermal depression, which can occur along the sidewalls or the radix but can also occur along the dorsum. These small depressions can be treated with careful self-massage and, later, if necessary, in-office injections of dissolvable dermal fillers, which will act as spreader material. Other minor deformities, which are frequently caused by bone or cartilaginous spicules, can be treated with percutaneous needle access or gentle rasping under local anesthesia.
Recurrence or Persistent of the Dorsal Convexity
In cases when a genuine dorsal convexity reoccurs (as opposed to transient inflammatory or callus-type convexities) or is observed as a residual effect due to the incomplete intraoperative hump resolution, a revisionary surgery may become necessary. Conducting a meticulous physical examination is essential in order to accurately determine whether the observed abnormality is indeed a genuine dorsal hump, as opposed to a low radix or supratip saddling that may be disguising itself as a hump.
Axis Deviation
The optimal nasal dorsum has a linear and perpendicular trajectory, effectively bisecting the face into 2 imperfectly symmetric vertical halves. A lateral deviation of the axis is defined as the divergence of the nasal dorsum toward either side of the midline. The occurrence of lateral deviations of the dorsum subsequent to DP surgery may be attributed to the asymmetrical healing of the PDO.
Additionally, residual septal deviation, particularly caudally and dorsally, may cause axis deviation of the dorsum. This undesirable complication can be avoided with performing symmetric push down, adequate fixation, and proper septoplasty. If the deviation is a result of the asymmetry of nasal bone heights, asymmetric PDO, or unilateral wedge resection (as in LDO) in conjunction with PDO may be indicated in the initial surgery. Gubisch emphasized the Cottle axiom “as the septum goes, so goes the nose,” arguing that nasal deviations are always related to or associated with septal deformities. Facing this deviation, the surgeon can perform in-office lateral manipulation very similar to nasal fracture reductions, but done very gently with incremental increasing pressure during about 3mn on a lying patient who is asked to express if any pain occurs. Then a taping is left for a few days. This maneuver can be done painless till 1 y postoperation.
Middle Third Widening and Thickening
PDO and LDO naturally produce a biomechanical widening of the middle vault. This can be prevented intraoperatively by performing a ballerina maneuver or a ULC partial disarticulation from the septum. Early postoperative middle third widening may be attributable to edema and can be treated conservatively with digital massages, taping, possible triamcinolone injections, and time. However, in cases of persistent middle vault fullness, surgical revision may be considered. This widening is frequently observed in the frontal view, resulting in a flared nasal morphology following PDO. Contrary to what may be observed in patients with polly beak deformity, (that has never been observed in our experience after PR) the profile contours of these patients are satisfactory.
A possible cause of middle third widening may be excess or overlap of fibrocartilaginous tissue in the scroll area after PDO, in which scar tissue formation in the proximal scroll area, corresponding to the W-point, or excessive overlap of the caudal ULC scroll at the junction of ULC with lower lateral cartilages (LLC) results in tissue excess in the middle third. Surgical resection of the surplus tissue is the definitive treatment for this untoward finding if medical therapy fails.
Alternatively, the widening of the middle third may be due to the bowing of the ULCs in response to PDO, thereby widening the arch of the cartilaginous vault. If widening of the middle third is not desired, the surgeon must consider preventative maneuvers during the primary DP procedure to account for this bowing. The widening of the middle third correlates directly with the amount of push down, that is, reduction in dorsal height, and this effect is logically magnified in patients with cartilaginous noses and short nasal bones. Notably, the widening is not always undesirable, as it can enhance the aesthetics of a narrow vault and enlarge the internal valve; this is an advantage of DP over structural techniques in such situations.
Supratip Saddling
The W-ASA segment provides structural support for the supratip region. If the superior strip incision begins at the ASA, the descent of the dorsum will always cause the W-ASA height to decrease, resulting in a loss of support and a saddling in the supratip region. For this reason, we advocate always beginning at the W point to maintain the W-ASA height. Once the dorsum has been brought to the appropriate height, the W-ASA height can be adjusted through incremental direct cartilage excisions, allowing for the management of supratip height. Again, prevention is preferable to treatment. Should intraoperative supratip saddling be detected, it can be corrected with solid or fragmented cartilage grafting. In the postoperative period, filler injections should be discussed.
Bony Step Offs
Bony steps can be observed in areas of osteotomy, most frequently in the region of the radix osteotomy, but also in the regions of lateral osteotomy and less frequently in the territory of transverse osteotomy. It is imperative that the surgeon examines these areas of palpable/visible step-offs intraoperatively. In case of visible step-offs either at the radix, or on the lateral walls, we recommend to simply perform what we name “rescue percutaneous osteotomies” to cut the excess of residual bone at a higher level, to drop it inside the fracture line and to forget it there (article unpublished procedure). Sometimes, a simple rasping can frequently enhance the contours and prevent the need for revisional surgery.
Postoperatively, rasping or meticulous infrascturing of proud segments may be performed in a clinic or in the operating room under local anesthesia. The location of a radix osteotomy is crucial in terms of the risk of step deformity. To circumvent this problem, the osteotomy must be conducted cephalically to the intercanthal line. The orientation of the osteotome is also crucial. If the radix is perpendicular to the sellion, it may collapse; if it is angled downward, a hinge is formed that substantially reduces the risk of collapsing. Nonetheless, if an unintended step occurs, the simplest way to correct the problem is to execute another osteotomy via the same percutaneous approach, cutting the bone at a higher level tangential to the glabella, and dropping the bone fragment in the fracture. The same procedure can be readily done percutaneously after too high lateral osteotomies; a technique we refer to as “rescue osteotomies.”
Dorsal contouring with DP is an effective method with exceptional long-term functional and aesthetic results. In this article, we have provided a concise summary of the superior strip technique in dorsal preservation. We have additionally reviewed pertinent indications, advantages, and possible pitfalls in this technique. It goes without saying that the rhinoplasty surgeon must have an in-depth understanding of nasal anatomy, the biodynamics of dorsal preservation, and the technical nuances and philosophy of DP. When the proper DP technique is applied to the proper nose type, the results are astoundingly satisfying and long-lasting.
Clinics care points
- •
Preservation of the keystone area is crucial for both structural and aesthetic outcomes. Proper handling prevents complications like inverted V deformity and ensures long-term stability.
- •
Appropriate patient selection is vital for successful dorsal preservation. Not all nasal types are suitable for DP, and improper selection can lead to suboptimal results and increased complication rates.
- •
Fixating the neodorsum to the stable septum via open or percutaneous sutures significantly reduces the risk of lateralization, deviation, and postoperative hump recurrence.
- •
Incomplete lateral or transverse osteotomies can lead to difficulties with mobilization and manipulation of the nasal pyramid. Ensuring full mobilization is a key to preventing undesirable fractures and achieving the desired contour.
- •
Performing incremental septal strip excisions allows for better control of dorsum height and minimizes the risk of over-resection, especially when fine-tuning the final outcome.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree