Introduction170
INTRODUCTION
SARCOIDAL GRANULOMAS
SARCOIDOSIS
Histopathology
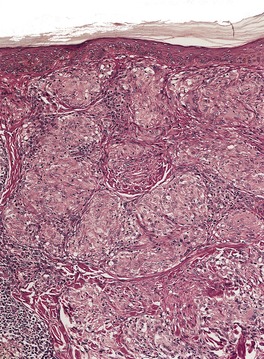
Fig. 7.1
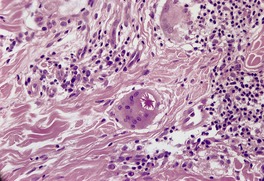
Fig. 7.2
REACTIONS TO FOREIGN MATERIALS
TUBERCULOID GRANULOMAS
TUBERCULOSIS
Histopathology
Histological differential diagnosis
TUBERCULIDS
LEPROSY
Histopathology206
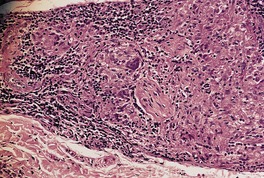
Fig. 7.3
FATAL BACTERIAL GRANULOMA
Histopathology
LATE SYPHILIS
LEISHMANIASIS
ROSACEA
Histopathology225
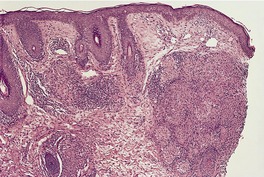
Fig. 7.4
IDIOPATHIC FACIAL ASEPTIC GRANULOMA
Histopathology
PERIORAL DERMATITIS
Histopathology
LUPUS MILIARIS DISSEMINATUS FACIEI
Histopathology
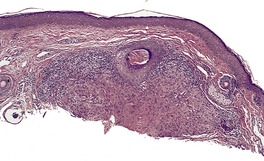
Fig. 7.5
CROHN’S DISEASE
NECROBIOTIC (COLLAGENOLYTIC) GRANULOMAS
GRANULOMA ANNULARE
Treatment of granuloma annulare
Histopathology
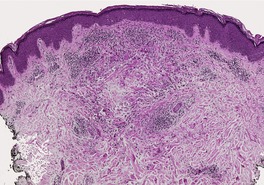
Fig. 7.6
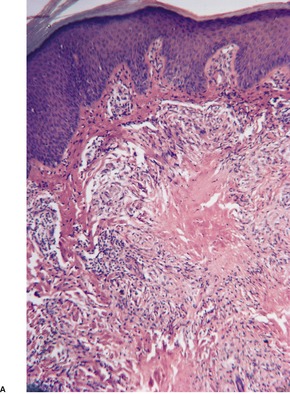
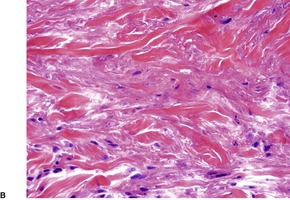
Fig. 7.7
Note: additional rare causes of necrobiotic granulomas include injected bovine collagen, Trichophyton rubrum infection, suture material, berylliosis, injection sites of drugs of abuse, hepatitis B vaccine, disodium clodronate, ataxia telangiectasia, parvovirus B19 infection, metastatic Crohn’s disease.
‘Blue’ granulomas
‘Red’ granulomas
Granuloma annulare
Necrobiosis lipoidica
Wegener’s granulomatosis
Necrobiotic xanthogranuloma
Rheumatoid vasculitis
Rheumatoid nodule
Pseudorheumatoid nodules of adults
Churg–Strauss syndrome
Eosinophilic cellulitis (Wells’ syndrome)
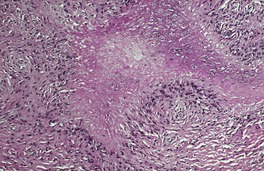
Fig. 7.8
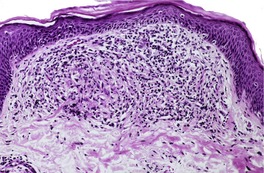
Fig. 7.9
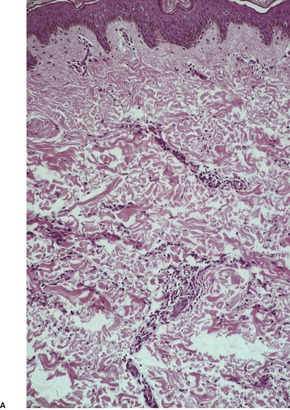
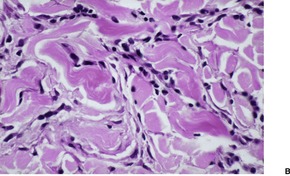
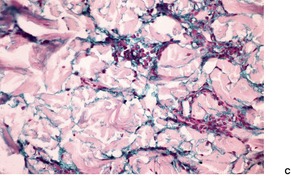
Fig. 7.10
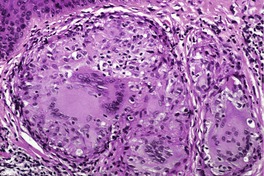
Fig. 7.11
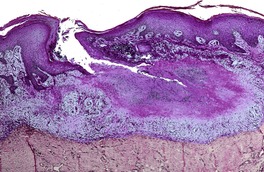
Fig. 7.12
Electron microscopy
NECROBIOSIS LIPOIDICA
Treatment of necrobiosis lipoidica
Histopathology
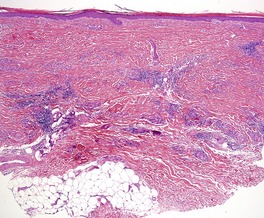
Fig. 7.13
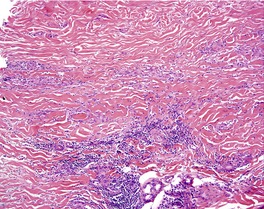
Fig. 7.14

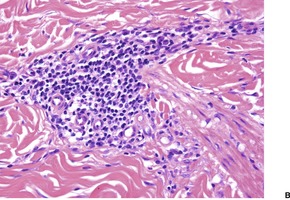
Fig. 7.15
NECROBIOTIC XANTHOGRANULOMA
Histopathology
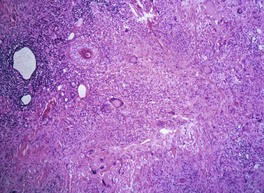
Fig. 7.16
RHEUMATOID NODULES
Histopathology
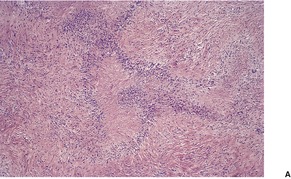
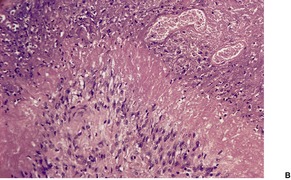
Fig. 7.17
RHEUMATIC FEVER NODULES
Histopathology
REACTIONS TO FOREIGN MATERIALS AND VACCINES
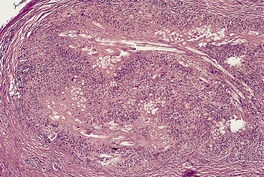
Fig. 7.18
MISCELLANEOUS DISEASES
SUPPURATIVE GRANULOMAS
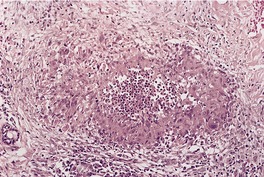
Fig. 7.19
Histopathology
CHROMOMYCOSIS AND PHAEOHYPHOMYCOSIS
SPOROTRICHOSIS
NON-TUBERCULOUS MYCOBACTERIAL INFECTIONS
BLASTOMYCOSIS
PARACOCCIDIOIDOMYCOSIS
COCCIDIOIDOMYCOSIS
BLASTOMYCOSIS-LIKE PYODERMA
MYCETOMAS, NOCARDIOSIS, AND ACTINOMYCOSIS
CAT-SCRATCH DISEASE
LYMPHOGRANULOMA VENEREUM
PYODERMA GANGRENOSUM
RUPTURED CYSTS AND FOLLICLES
FOREIGN BODY GRANULOMAS
EXOGENOUS MATERIAL
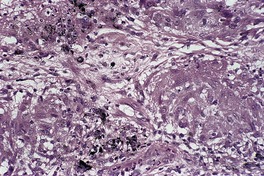
Fig. 7.20
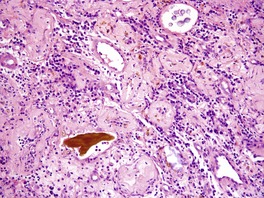
Fig. 7.21
ENDOGENOUS MATERIAL
XANTHOGRANULOMAS
MISCELLANEOUS GRANULOMAS
CHALAZION
Histopathology
MELKERSSON–ROSENTHAL SYNDROME
Histopathology
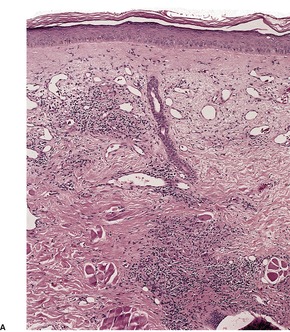
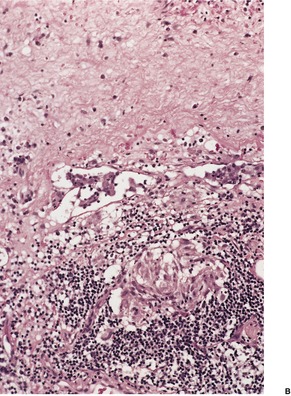
Fig. 7.22
ELASTOLYTIC GRANULOMAS
Actinic granuloma
Histopathology
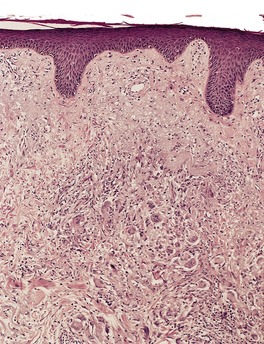
Fig. 7.23
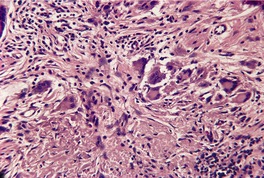
Fig. 7.24
Annular elastolytic giant cell granuloma
Histopathology
Atypical necrobiosis lipoidica
Histopathology
Granuloma multiforme
Histopathology
ANNULAR GRANULOMATOUS LESIONS IN OCHRONOSIS
Histopathology
GRANULOMAS IN IMMUNODEFICIENCY DISORDERS
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


The granulomatous reaction pattern
Suppurative granulomas184
Chromomycosis and phaeohyphomycosis185
Sporotrichosis185
Non-tuberculous mycobacterial infections185
Blastomycosis185
Paracoccidioidomycosis185
Coccidioidomycosis185
Blastomycosis-like pyoderma185
Mycetomas, nocardiosis, and actinomycosis186
Cat-scratch disease186
Lymphogranuloma venereum186
Pyoderma gangrenosum186
Ruptured cysts and follicles186
Xanthogranulomas187
Miscellaneous granulomas187
Combined granulomatous and lichenoid pattern194
The granulomatous reaction pattern is defined as a distinctive inflammatory pattern characterized by the presence of granulomas. Granulomas are relatively discrete collections of histiocytes or epithelioid histiocytes with variable numbers of admixed multinucleate giant cells of varying types and other inflammatory cells. 1 Conditions in which there is a diffuse infiltrate of histiocytes within the dermis, such as lepromatous leprosy, are not included in this reaction pattern. The group is subdivided by way of:
• the arrangement of granulomas;
• the presence of accessory features such as central necrosis, suppuration, or necrobiosis; and
• the presence of foreign material or organisms.
It is difficult to present a completely satisfactory classification of the granulomatous reactions. 2 As Hirsh and Johnson remark in their review of the subject, ‘Sometimes a perfect fit can be achieved only with the help of an enlightened shove’. 3 Many conditions described within this group may show only non-specific changes in the early evolution of the inflammatory process and in a late or resolving stage show fibrosis and non-specific changes without granulomas. Occasionally a variety of granuloma types may be seen in one area, e.g. in reactions to foreign bodies or around ruptured hair follicles.
It is necessary in any granulomatous dermatitis to exclude an infectious cause. In some countries, up to 90% of granulomas have an infectious etiology. 4 Culture of fresh tissue as well as histological search increases the chances of identifying a specific infectious agent. The time-consuming examination of multiple sections may be necessary to exclude such a cause. Special stains for organisms may be indicated. Occasionally fungi are shown only by silver stains, such as Grocott methenamine silver, and not by PAS staining. All granulomas should be examined under polarized light to detect or exclude birefringent foreign material.
Considerable advances have been made in the understanding of the formation and maintenance of granulomas in tissue reactions and the roles played by B and T lymphocytes and cytokines.5.6.7. and 8. It is also clear that there are several types of macrophages in granulomas, particularly at an ultrastructural level. 9 The different forms of multinucleate giant cells seen in granulomas may simply reflect the types of cytokines being produced by the component cells. 10 This new information has not so far been shown to be useful in routine diagnostic problems. The glioma-associated oncogene homologue gli-1 is expressed in lesional skin in patients with cutaneous sarcoidosis, granuloma annulare, and necrobiosis lipoidica. 11 These findings provide a rationale for clinical trials of inhibitors of gli-1 signaling, including tacrolimus and sizolimus, for the treatment of these conditions. 11 Polymerase chain reaction techniques (PCR) have proved useful in detecting infectious agents in tissue sections, particularly mycobacterial species.12.13.14.15. and 16.
The following types of granulomas form the basis of the subclassification of diseases in this reaction pattern.
• Sarcoidal – granulomas composed of epithelioid histiocytes and giant cells with a paucity of surrounding lymphocytes and plasma cells (‘naked’ granulomas).
• Tuberculoid – granulomas composed of epithelioid histiocytes, giant cells of Langhans and foreign body type with a more substantial rim of lymphocytes and plasma cells and sometimes showing central ‘caseation’ necrosis. Granulomas have a tendency to confluence.
• Necrobiotic (collagenolytic) – granulomas are usually poorly formed and there are collections, and a more diffuse array, of histiocytes, lymphocytes, and giant cells with associated ‘necrobiosis’ (collagenolysis). The inflammatory component may be admixed with the ‘necrobiosis’ or form a palisade around it.
• Suppurative – granulomas composed of epithelioid histiocytes and multinucleate giant cells with central collections of neutrophils. Chronic inflammatory cells are usually present at the periphery of the granulomas.
• Foreign body – granulomas composed of epithelioid histiocytes, multinucleate (foreign body-type) giant cells, and variable numbers of other inflammatory cells. There is identifiable foreign material, either exogenous or endogenous in origin.
• Xanthogranulomas – granulomas composed of numerous histiocytes with foamy/pale cytoplasm with a variable admixture of other inflammatory cells and some Touton giant cells
• Miscellaneous – a category in which the granulomas may be variable in appearance or do not always fit neatly into one of the above categories.
Many of the conditions exhibiting a granulomatous tissue reaction have been discussed in other chapters; they will be mentioned only briefly.
The various granulomatous diseases will be discussed, in order, according to the classification listed above.
Sarcoidal granulomas are found in sarcoidosis and in certain types of reaction to foreign materials and squames.
The prototypic condition in this group is sarcoidosis. Sarcoidal granulomas are discrete, round to oval, and composed of epithelioid histiocytes and multinucleate giant cells which may be of either Langhans or foreign body type. Generally, the type of multinucleate histiocyte present in a granuloma is not helpful in arriving at a specific histological diagnosis. Giant cells may contain asteroid bodies, conchoidal bodies (Schaumann bodies), or crystalline particles. Typical granulomas are surrounded by a sparse rim of lymphocytes and plasma cells, and only occasional lymphocytes are present within them. Consequently, they have been described as having a ‘naked’ appearance. Although the granulomas may be in close proximity to one another, their confluence is not commonly found. With reticulin stains, a network of reticulin fibers is seen surrounding and permeating the histiocytic cluster.
Sarcoidal granulomas can be found in the following circumstances:
• sarcoidosis
• Blau’s syndrome
• foreign body reactions (see Table 7.1)
Silica (including windshield glass)
Silicone
Tattoo pigments
Zirconium
Beryllium
Zinc
Acrylic or nylon fibers
Keratin from ruptured cysts (uncommon)
Exogenous ochronosis
Sea-urchin spines
Cactus
Wheat stubble
Desensitizing injections
Ophthalmic drops (sodium bisulfite)
Sulfonamides
Interferon injection sites
• Sézary syndrome17
• metastatic Crohn’s disease
• orofacial granulomatosis
• granuloma annulare (sarcoidal type)
• herpes-zoster scars18
• breast cancer21
• common variable immunodeficiency (see p. 191)
• X-linked hyper-IgM syndrome. 22
Sarcoidal granulomas are exceedingly rare in secondary syphilis (see p. 575), Sézary syndrome, herpes-zoster scars (see p. 617), systemic lymphomas, and breast cancer. The granulomas in metastatic Crohn’s disease and orofacial granulomatosis are often of mixed sarcoidal and tuberculoid types. These diseases are considered with the miscellaneous granulomatous diseases (see p. 188). The sarcoidal variant of granuloma annulare is discussed with other types of this condition (see p. 180). They will not be considered further in this section.
Sarcoidosis is a multisystem disease which may involve any organ of the body but most commonly affects the lungs, lymph nodes (mediastinal and peripheral), skin, liver, spleen, and eyes.23.24.25. and 26. Central nervous system involvement is uncommon. 27 There is an increased incidence of sarcoidosis in people of Irish and Afro-Caribbean origin. 28 Cutaneous sarcoidosis is rare in Asia. 29
Between 10% and 35% of patients with systemic sarcoidosis have cutaneous lesions.30.31. and 32. Although sarcoidosis is usually a multiorgan disease, chronic cutaneous lesions may be the only manifestation. 33 The skin lesions may be specific, showing a granulomatous histology, or non-specific. The most common non-specific skin lesion is erythema nodosum, which is said to occur in 3–25% of cases. 30 Sarcoidosis of the knees is frequently associated with erythema nodosum. 34 An erythema nodosum-like eruption with the histological changes of sarcoidosis has also been described. 35 Sarcoidosis predominantly affects adults; skin lesions are rarely seen in children.36.37.38. and 39. There are reports of its occurrence in monozygotic twins. 40 Children presenting before the age of 4 years, usually have the triad of rash, uveitis, and arthritis,41. and 42. without apparent pulmonary involvement. 42 This early-onset sarcoidosis (OMIM 609464) is caused by mutations in the NOD2/CARD15 gene on chromosome 16q12, similar to Blau’s syndrome (see below). Vasculitis may also occur in this group. 42
A diversity of clinical forms of cutaneous sarcoidosis occurs. These forms include:
• A maculopapular eruption associated with acute lymphadenopathy, uveitis, or pulmonary involvement.
• Plaques with marked telangiectasia (angiolupoid sarcoidosis).
• Nodular subcutaneous sarcoidosis.47.48.49.50.51.52. and 53. This form was diagnosed in 10 of 85 patients (11.8%) in one series. 54 Lesions were most frequently located on the extremities, particularly the forearms where indurated linear bands were sometimes found. It may occur on the breast, mimicking breast carcinoma. 55 Subcutaneous sarcoidosis is the only specific subset of cutaneous sarcoidosis frequently associated with systemic disease. 56
• A miscellaneous group which includes cicatricial alopecia,57. and 58. an acral form, 59 ichthyosiform sarcoidosis,60.61. and 62. ulcerative,63. and 64. necrotizing, morpheaform and mutilating forms,65.66.67.68. and 69. verrucous lesions,70. and 71. discoid lupus erythematosus-like lesions, 72 and erythroderma. 73 Cutaneous sarcoidal granulomas have also been reported at the site of cosmetic filler injections in patients with or without systemic sarcoidosis.74. and 75.
This miscellaneous group represents rare cutaneous manifestations of sarcoidosis. Lupus pernio may resolve with fibrosis and scarring and is often associated with involvement of the upper respiratory tract and lungs. 76 Oral, eyelid, and scrotal lesions have been reported.77.78. and 79. The majority of skin lesions resolve without scarring. Hypopigmented macules without underlying granulomas have been described, particularly in patients of African descent. 80 Other rare presentations have included leonine facies, 81 faint erythema, 82 palmar erythema, 83 vasculitis, 42 alopecia,84. and 85. and lesions confined to the vulva. 86 Sarcoidosis may follow the use of interferon therapy (IFN-α) for melanoma87 or hepatitis C.88.89.90.91.92.93. and 94. Sometimes the lesions are limited to injection site scars in these patients. 95 It may also occur in patients with hepatitis C unrelated to treatment. 96 It has also followed BCG vaccination. 97
It is generally considered that the presence of cutaneous lesions in association with systemic involvement is an indicator of more severe disease. Skin lesions may occur in scars98.99.100. and 101. following trauma (including surgery, desensitizing injection sites, and venepuncture),102.103. and 104. cosmetic tattoos,105. and 106. radiation, and chronic infection. In some cases these lesions may be the first manifestation of sarcoidosis.107. and 108. Other cases do not appear to be related to systemic sarcoidosis and may be a sarcoidal reaction to a foreign body. 109
Various systemic diseases have been reported in association with cutaneous sarcoidosis. The association in many of these conditions is probably fortuitous. They include B-cell chronic lymphocytic leukemia, 110 cutaneous lymphoma,111. and 112. pyoderma gangrenosum, 113 hypoparathyroidism, 114 cryptococcal infection, 115 dermatomyositis, 116 primary biliary cirrhosis, 117 autoimmune thyroiditis and/or vitiligo,118.119. and 120. polycythemia vera, 121 Wegener’s granulomatosis, 122 and HIV infection. 123 In cases of HIV infection, sarcoidosis may develop after the commencement of highly active antiretroviral therapy (HAART) and the restoration of some immune function.123. and 124. The term ‘immune restoration disease’ has been used for this circumstance. Subcutaneous granulomas and granulomatous tenosynovitis have been reported in an organ transplant recipient. 125
The etiology of sarcoidosis remains controversial although an infectious origin has long been suspected.126. and 127. The main candidate is a cell-wall-deficient form of an acid-fast bacillus, similar, if not identical to, Mycobacterium tuberculosis. 128 In one study, DNA sequences coding for the mycobacterial 65 kDa antigen were found in 11 of 35 cases of sarcoidosis, 129 while in a more recent study, using only cutaneous specimens, mycobacterial DNA was demonstrated by PCR in 16 of 20 cases. 130 Non-tuberculous (atypical) mycobacteria constitute the largest group of the species identified in this study. 130 Other findings supportive of a mycobacterial etiology are the beneficial effects of long-term tetracyclines131 and the activation of a case following concurrent M. marinum infection of the skin. 132 In a study of 35 patients with sarcoidosis in 2005, M. tuberculosis rRNA was not detected in any case. 133 Based on these results the authors concluded that this organism cannot be considered as the etiological agent of the disease. 133 Another study concluded that there was no role for human herpesvirus type 8 (HHV-8) in the etiology, despite earlier reports suggesting a role. 134
Several studies have reported increased T-helper (Th)-1 cytokines with increased levels of tumor necrosis factor (TNF)-α in patients with sarcoidosis. 135
The exact relationship of Blau’s syndrome (OMIM 186580) to sarcoidosis is becoming clearer. It is characterized by the familial presentation of a sarcoid-like granulomatous disease involving the skin, uveal tract and joints, but not the lung. 136 Camptodactyly is another defining sign. 137 Ichthyosis has been reported in one case. 138 Onset is in childhood and the mode of inheritance is autosomal dominant. It shares with early-onset sarcoidosis mutations in the NOD2/CARD15 gene which maps to chromosome 16q12.139.140. and 141. Some patients with Crohn’s disease also have mutations in this gene.
For limited cutaneous sarcoidosis, parenteral therapies have been the mainstay of therapy but systemic therapy has been used for severe cutaneous disease, particularly if there is an aesthetic impact. 142 Therapies that have been used include corticosteroids, hydroxychloroquine, chloroquine, allopurinol, methotrexate, isotretinoin, mepacrine, 143 tacrolimus, 144 thalidomide, 142 and various inhibitors of TNF-α such as adalimumab145. and 146. and infliximab.135. and 147. The various therapies used to treat cutaneous sarcoidosis have recently been reviewed. 148
There is a dermal infiltrate of naked sarcoidal granulomas (Fig. 7.1). 149 Granulomas may be present only in the superficial dermis or they may extend through the whole thickness of the dermis or subcutis, depending on the type of cutaneous lesion. 150 Interstitial and tuberculoid granulomas are uncommon. 149 Both perineural and periadnexal localization of the granulomas has been reported.149.151. and 152. A granulomatous vasculitis is exceedingly rare. 153 Necrosis is not usually seen in granulomas but has been reported. 154 Small amounts of fibrinous or granular material may be seen in some granulomas. 23 Increased mucin is present in about 20% of cases. 149 Fibrinoid necrosis is said to be quite common in the cutaneous lesions of black South Africans. 28 Slight perigranulomatous fibrosis may be present but marked dermal scarring is unusual except in lupus pernio or necrotizing and ulcerating lesions. Fibrosis is often present in subcutaneous sarcoidosis. Touton-like giant cells may rarely be present. 155
Sarcoidosis. The granulomas in the dermis are composed of epithelioid histiocytes and multinucleate giant cells with only a sparse infiltrate of lymphocytes at the periphery (‘naked’ granulomas). (H & E)
In subcutaneous sarcoidosis the granulomas are usually limited to the subcutis without any dermal extension. The infiltrate is predominantly lobular with little or no septal involvement. 54 Discrete foci of necrosis may be present in the center of some granulomas in a few cases. 54 Perigranulomatous fibrosis, sometimes encroaching on the septa, is also present. 156
Overlying epidermal hyperplasia occurs in verrucous lesions70 and hyperkeratosis occurs in the rare ichthyosiform variant. 60 A lichenoid variant has been reported. There was a thick band-like infiltrate of sarcoidal granulomas with basal apoptotic keratinocytes. 157 Otherwise, in most cases, the overlying epidermis is normal or atrophic.
Transepidermal elimination has been reported in sarcoidosis and the histology shows characteristic elimination channels. 158 In some cases the round cell infiltrate surrounding the granulomas is more intense and the granulomas less discrete. The diagnosis of sarcoidosis may then become one of exclusion.
Asteroid bodies and conchoidal bodies (Schaumann bodies) may be seen in multinucleate giant cells but are not specific for sarcoidosis and may occur in other granulomatous reactions including tuberculosis (Fig. 7.2). Schaumann bodies, which are shell-like calcium-impregnated protein complexes, are much more common in the granulomas of sarcoidosis than in those of tuberculosis. 159 Birefringent material has been found in the granulomas from 22–50% of cases.149.150.160. and 161. Foreign bodies are more common in sarcoidal granulomas from sites subject to minor trauma, such as the knee.34. and 161. Furthermore, patients with sarcoidosis can get granulomas at the sites of implantation of foreign material.162. and 163. Electron probe microanalysis has identified calcium, phosphorus, silicon, and aluminum in the birefringent material referred to above. It is thought that the calcium salts are probably the precursors of Schaumann bodies. Another explanation for the material is that it represents foreign material inoculated during a previous episode of inapparent trauma leading to granuloma formation subsequently in a patient with sarcoidosis.164. and 165. Asteroid bodies are said by some to be formed from trapped collagen bundles166 or from components of the cytoskeleton, predominantly vimentin intermediate filaments. 167
Sarcoidosis. An asteroid body is present in the cytoplasm of a multinucleate giant cell. (H & E)
Biopsies taken from Kveim–Siltzbach skin test sites, sometimes used in the past for the diagnosis of sarcoidosis, show a variety of changes ranging from poorly formed granulomas with a heavy mononuclear cell infiltrate to small granulomas with few mononuclear cells. Measurement of the serum angiotensin-converting enzyme (ACE) level has now replaced this skin test.
Immunohistochemical marker studies have shown that the T lymphocytes expressing the suppressor/cytotoxic phenotype (CD8+) are found predominantly in the perigranulomatous mantle whereas those expressing the helper/inducer phenotype (CD4+) are present throughout the granuloma. 168 B lymphocytes are also present in the mantle zone.
Immunofluorescence studies in some cases have shown IgM at the dermoepidermal junction, IgM within blood vessel walls, and IgG within and around the granuloma. A fibrin network is present within granulomas. 169
A number of foreign substances and materials when introduced into the skin may induce a granulomatous dermatitis which histologically resembles sarcoidosis. They are listed in Table 7.1.
Following some kind of trauma, silica may contaminate a wound in the form of dirt, sand, rock, or glass (including windshield glass from motor vehicles). 170 Papules and nodules arise in the area of trauma. The granulomas seen in the dermal reaction contain varying numbers of Langhans or foreign body giant cells, some of which may contain clear colorless particles. These may be difficult to see with routine microscopy but are birefringent in polarized light. The differentiation from true sarcoidosis may be difficult, since granulomas sometimes develop in scars in sarcoidosis and the granulomas can contain birefringent calcite crystals. A sarcoidal reaction to identifiable foreign material does not exclude sarcoidosis. It has been suggested that particulate foreign material may serve as a nidus for granuloma formation in sarcoidosis. 171 Silica-rich birefringent particles have also been described in lesions without a history of injury or silica exposure. 172 Energy-dispersive X-ray analysis techniques using scanning electron microscopy can be used to identify elements present in the crystalline material. 173 The granulomas are thought to develop as a response to colloidal silica particles and not as a result of a hypersensitivity reaction. 174
A granulomatous dermatitis may occur in response to pigments used in tattooing (see p. 389).175. and 176. The skin lesions are sometimes limited to certain areas of a tattoo where a particular pigment has been used. 176 Two patterns are seen, a foreign body type and a sarcoid type. 177 In the latter form there are aggregates of epithelioid histiocytes and giant cells with a sparse perigranulomatous round cell infiltrate. The histiocytes and giant cells contain pigment particles. True sarcoidosis has also been reported in tattoos, in some cases associated with pulmonary hilar lymphadenopathy. Some of these cases may represent a generalized sarcoid-like reaction to tattoo pigments rather than true sarcoidosis.178. and 179. Other granulomatous complications of tattoos include tuberculosis cutis and leprosy. 180
Sarcoidal granulomas may occur as a rare complication of ear piercing. It is not always a consequence of the trauma/scarring but may represent a contact allergy to nickel and other metals. 181
Zirconium compounds used in under-arm deodorants and other skin preparations have been associated with a granulomatous skin reaction in sensitized individuals.182. and 183. Histologically, the lesions are identical to sarcoidosis. Usually no birefringent material is seen in polarized light. In one case of a reaction to an aluminum–zirconium complex, foreign body granulomas and birefringent particles were seen as well as tuberculoid type granulomas. 184 Ophthalmic drops containing sodium bisulfite have been implicated in the formation of pigmented papules on the face. The papules were caused by sarcoidal granulomas with brown-black pigment in foreign body giant cells. 185
Sarcoidal granulomas have been reported at the injection sites of interferon, both interferon β-1b used in the treatment of multiple sclerosis, 186 and interferon α-2a used in the treatment of hepatitis C. 187
In the past, cutaneous granulomatous lesions with histology similar to sarcoidosis have been reported in persons exposed to beryllium compounds in industry.188. and 189. Other foreign bodies capable of inducing sarcoidal granulomas include acrylic and nylon fibers, wheat stubble, and sea urchin spines.190.191. and 192. Sea urchin spines can produce all types of granuloma, not only sarcoidal ones. The nature of the granulomatous reaction that followed the use of hydroxyurea is uncertain. It may have been sarcoidosis itself. 193
Occasionally, keratin from ruptured cysts or hair follicles can induce sarcoidal granulomas rather than the more usual foreign body type of reaction.
While the granulomas in the tuberculoid group consist of collections of epithelioid histiocytes, including multinucleate forms, they tend to be less circumscribed than those in the sarcoidal group, have a greater tendency to confluence, and are surrounded by a substantial rim of lymphocytes and plasma cells. Langhans giant cells tend to be more characteristic of this group but foreign body type giant cells are also seen. There may be areas of caseation in the lesions of tuberculosis.
Tuberculoid granulomas are seen in the following conditions:
• tuberculosis
• tuberculids
• leprosy
• fatal bacterial granuloma
• late syphilis
• leishmaniasis
• rosacea
• idiopathic facial aseptic granuloma
• perioral dermatitis
• lupus miliaris disseminatus faciei
• Crohn’s disease.
In addition to these diseases, tuberculoid granulomas, some with central necrosis, have been described at injection sites of protamine-insulin, as a hypersensitivity reaction to protamine. One case, consisting of both tuberculoid and sarcoidal granulomas followed Q fever vaccination. 194 The granulomas occurring in the homolateral limb after previous mastectomy, although described as sarcoidal, were more of a tuberculoid nature. 21
Typical tuberculoid granulomas can be seen in the dermal inflammatory reaction of late primary inoculation tuberculosis, late miliary tuberculosis, tuberculosis cutis orificialis, tuberculosis verrucosa cutis (‘prosector’s wart’), scrofuloderma, and lupus vulgaris. 195 Cutaneous tuberculosis is discussed in detail with the bacterial infections (see p. 556). A similar pattern of inflammation can be seen after BCG vaccination and immunotherapy.196. and 197.
Santa Cruz and Strayer have stressed the variety of histological changes seen in cutaneous tuberculosis. 198 In many forms, particularly in early lesions, there is a mixture of inflammatory cells within the dermis which includes histiocytes and multinucleate cells without well-formed epithelioid granulomas. The changes seen in the overlying epidermis are variable. In some forms inflammatory changes extend into the subcutis. Areas of caseation may or may not be present within granulomas. In some cases this may be difficult to distinguish from the necrobiosis seen in rheumatoid nodules (see p. 183). The number of acid-fast organisms varies in different lesions. In lesions with caseation, organisms are most frequently found in the centers of necrotic foci. 199 Generally, where there are well-formed granulomas without caseation necrosis, organisms are absent or difficult to find. Neutrophils may be a component of the inflammatory infiltrate, and abscesses form in some clinical subtypes. Both Schaumann bodies and asteroid bodies can occasionally be present in multinucleate giant cells.
In lesions with caseation and demonstrable acid-fast organisms, the histological diagnosis may be straightforward. In lupus vulgaris, however, caseation necrosis, if present, is minimal and organisms are rarely found. Evidence of mycobacterial infection may be determined by polymerase chain reaction techniques. 200
There is usually a heavier round cell infiltrate about tuberculous granulomas than is seen in sarcoidosis. It is to be remembered that the small foci of fibrinous material that sometimes are seen in the granulomas of sarcoidosis may mimic and be mistaken for caseation. Epidermal changes and dermal fibrosis are not commonly part of the histopathology of sarcoidosis.
Lesions of other non-tuberculous mycobacterial infections of the skin, such as those due to Mycobacterium marinum, may be histologically indistinguishable from cutaneous tuberculosis. Organisms are usually difficult to find in M. marinum infections; they are described as being longer and broader than typical M. tuberculosis. Culture or PCR is required for species identification.
The combination of marked irregular epidermal hyperplasia, epidermal and dermal abscesses, and dermal tuberculoid granulomas may be seen in tuberculosis verrucosa cutis, caused by M. tuberculosis, and in swimming pool granuloma due to M. marinum infection. This reaction pattern is also seen in cutaneous fungal infections such as sporotrichosis, chromomycosis, and blastomycosis. Diagnosis depends on identification of the appropriate organism.
The lesions of tuberculosis cutis orificialis must be distinguished from those of oral or anal Crohn’s disease and from the Melkersson–Rosenthal syndrome (see p. 188). This is not always possible on histological grounds and may depend on clinical history and associated lesions. Foci of caseation and acid-fast organisms may be seen in tuberculous lesions. Marked edema and granulomas related to or in the lumen of dilated lymphatic channels are present in the Melkersson–Rosenthal syndrome.
The tuberculids are a heterogeneous group of cutaneous disorders associated with tuberculous infections elsewhere in the body or in other parts of the skin (see p. 559). They include lichen scrofulosorum, papulonecrotic tuberculid, and erythema induratum-nodular vasculitis. Although it has previously been thought that organisms are not found in tuberculids, recent PCR studies have demonstrated mycobacterial DNA in some cases (see p. 559). 200
In lichen scrofulosorum there is a superficial inflammatory reaction about hair follicles and sweat ducts which may include tuberculoid granulomas. Acid-fast organisms are not usually seen or cultured from the lesions. 201 Caseation is rare. 202
Histopathological studies of papulonecrotic tuberculid have shown a subacute or granulomatous vasculitis and dermal coagulative necrosis with, in some cases, a surrounding palisading histiocytic reaction resembling granuloma annulare. 203 Acid-fast bacilli are not found in the lesions. Tuberculoid granulomas were not described in one study204 but have been recorded in others. 195
In erythema induratum-nodular vasculitis there is a lobular panniculitis, although tuberculoid granulomas usually extend into the deep dermis (see p. 463).
Tuberculoid granulomas are seen in the tuberculoid (TT), borderline tuberculoid (BT), and borderline (BB) groups of the classification of leprosy introduced by Ridley and Jopling. 205 Leprosy is considered further on page 562.
In tuberculoid leprosy (TT), single or grouped epithelioid granulomas with a peripheral rim of lymphocytes are distributed throughout the dermis and subcutis. Unlike lepromatous leprosy this infiltrate does not spare the upper papillary dermis (grenz zone) and it may extend into and destroy the basal layer and part of the stratum malpighii. The granulomas are characteristically arranged in and around neurovascular bundles and arrectores pilorum muscles. Granulomas, particularly in the deeper parts of the infiltrate, tend to be oval and elongated along the course of the nerves and vessels (Fig. 7.3). Small cutaneous nerve bundles are infiltrated and enlarged by the inflammatory cells. There may be destruction of nerves, sometimes with caseation necrosis which may mimic cutaneous tuberculosis. In contrast, the infiltrate in tuberculosis is not particularly related to nerves. The granulomas in tuberculoid leprosy may contain well-formed Langhans-type giant cells and less well-formed multinucleate foreign body giant cells. The causative organism, Mycobacterium leprae, which is best demonstrated by modifications of the Ziehl–Neelsen stain such as the Wade–Fite method, is usually not found in the lesions of tuberculoid leprosy. Rare organisms may be present in nerve fibers. PCR has been used to demonstrate DNA of M. leprae in lesions. 16
Leprosy. The tuberculoid granuloma is elongated along the course of a nerve in the deep dermis. (H & E)
Granulomas in the borderline tuberculoid form (BT) are surrounded by fewer lymphocytes, contain more foreign body giant cells than Langhans cells, and may or may not extend up to the epidermis. Organisms may be found in small numbers or not at all. Nerve bundle enlargement is not so prominent and there is no caseation necrosis or destruction of the epidermis.
In the borderline form (BB) the granulomas are poorly formed and the epithelioid cells separated by edema. Scant lymphocytes are present about the granulomas and there are no giant cells. Nerve involvement is slight. Organisms are found, usually only in small numbers.
This condition was first reported in the English literature in 2002 under the title ‘fatal bacteria granuloma after trauma: a new entity’. 207The cases were reported from rural China. They were characterized by spreading, dark-red plaques that followed slight trauma to the face. The patients had severe headache and clouding of consciousness during the later stages of the disease. All patients died within 1.5– 4 years.
Electron microscopy demonstrated two types of bacteria: one was an anaerobic actinomycete, which was sensitive to lincomycin (a forerunner of clindamycin); the other organism seen was a Staphylococcus. The unknown actinomycete was regarded as the probable causative agent. 207 A recent paper has reported finding Propionibacterium acnes, which seems unusual. 208
The epidermis was normal and there was a heavy, diffuse dermal infiltrate of cells, mainly histiocytes. In addition there were lymphocytes, plasma cells, neutrophils, and many multinucleated giant cells in some areas. There was vascular occlusion with focal hemorrhage and necrosis in the deep dermis. 207
Some lesions of late secondary syphilis and nodular lesions of tertiary syphilis show a superficial and deep dermal inflammatory reaction in which there are tuberculoid granulomas (see p. 575). 209 Plasma cells are generally but not always prominent in the inflammatory infiltrate and there may be swelling of endothelial cells.210. and 211. One recent study has found that a plasma cell infiltrate and endothelial swelling, traditionally associated with syphilis of the skin, are in fact infrequently seen in biopsies. 212 Organisms are rarely demonstrable in these lesions.
In chronic cutaneous leishmaniasis (see p. 635) and leishmaniasis recidivans, tuberculoid granulomas are present in the upper and lower dermis. 213 The overlying epidermal changes are variable. Occasionally the granulomas extend to the basal layer of the epidermis as in tuberculoid leprosy. 214 Necrosis is not usually seen in the granulomas. 215 Leishmaniae are usually scarce but may be found in histiocytes or, rarely, free in the dermis. The organisms have sometimes been mistaken for Histoplasma capsulatum but differ from the latter in having a kinetoplast.
Rosacea is characterized by persistent erythema and telangiectasia, predominantly of the cheeks but also affecting the chin, nose, and forehead (see p. 434). The lacrimal and salivary glands were affected in one case. 216 In the papular form, papules and papulopustules are superimposed on this background. Tuberculoid granulomas are seen in the granulomatous form. Granulomatous rosacea has been reported in children as well as adults, and in association with infection with the human immunodeficiency virus (HIV).217.218. and 219. Granulomatous rosacea can be found in most clinical variants of rosacea. 220 A rosacea-like granulomatous eruption developed in an adult patient using tacrolimus ointment in the treatment of atopic dermatitis. 221 Granulomas may be a response to Demodex organisms or lipids.222. and 223. Granulomas have also been described in the lesions of pyoderma faciale, thought to be an extreme form of rosacea. 224
The changes seen in biopsies of the papules are variable and relate to the age of the lesion. Early lesions may show only a mild perivascular lymphocytic infiltrate in the dermis. In older lesions there is a mixed inflammatory infiltrate related to the vessels or to vessels and pilosebaceous units. The infiltrate consists of lymphocytes and histiocytes with variable numbers of plasma cells and multinucleate giant cells of Langhans or foreign body type. In some lesions epithelioid histiocytes and giant cells are organized into tuberculoid granulomas (granulomatous rosacea) (Fig. 7.4). 226 An acute folliculitis with follicular and perifollicular pustules and destruction of the hair follicle is sometimes seen. This corresponds to the perifollicular variant of granulomatous rosacea described by Sánchez et al. 220 Granulomatous inflammation may be centered on identifiable ruptured hair follicles. At other times the granulomas are distributed diffusely through the dermis. 220 There is dermal edema and vascular dilatation. Epidermal changes, if present, are mild and non-specific.
Granulomatous rosacea. Tuberculoid granulomas are present in the dermis. There is some telangiectasia of vessels in the superficial dermis. (H & E)
In granulomatous rosacea, the granulomas are usually of tuberculoid type and not the ‘naked’ granulomas of sarcoidosis (see p. 172). Changes resembling caseous necrosis may be present, associated with a histiocytic reaction. In one series, necrosis was present in 11% of cases. 217 Differentiation from lupus vulgaris may be difficult. In some cases of rosacea the inflammatory changes may be related to damaged hair follicles. The presence of marked vascular dilatation is suggestive of rosacea.
Thirty cases of this unusual granulomatous condition of the face have been reported from a single center in France.227. and 228. All cases occurred in children, with a mean age of 3.8 years. The children presented with one or several acquired painless nodules on the face, lasting for at least one month. There was no response to antibiotics and no infectious agent was demonstrated. It was suggested that the disease might belong to the spectrum of childhood rosacea. 228 A granulomatous response to an embryological residue was also considered. 228
The lesions were composed of granulomas consisting of lymphocytes, histiocytes, epithelioid cells, some neutrophils, and numerous foreign body giant cells. In one case, the granulomas developed around a non-ruptured epidermoid cyst. 228 Foreign body giant cells would be unusual as the predominant feature in rosacea; accordingly, this etiological theory (see above) seems unlikely.
Perioral dermatitis is regarded by some as a distinct entity229 and by others as a variant of rosacea. 230 The histological changes seen in perioral dermatitis and acne rosacea overlap, and clinical features are often more important in separating these two conditions. 231
Red papules, papulovesicles, or papulopustules on a background of erythema are arranged symmetrically on the chin and nasolabial folds with a characteristic clear zone around the lips. 232 Lesions may occur less commonly on the lower aspect of the cheeks and on the forehead. 233 A periocular variant has also been described.234. and 235. Perioral dermatitis chiefly affects young women, but it has also been reported in children.236.237.238. and 239. In a recent review of patients with lip and perioral area dermatitis, Nedorost has presented a useful table with the distinguishing features between a rosacea-type of perioral dermatitis, a steroid-induced type, and disease due to irritants, allergic/photoallergic contact reactions, and atopic cheilitis. 240 She suggests that an extended patch test series may be useful in making a diagnosis. 240 Inhaled corticosteroids may also induce the disease. 241
Granulomatous perioral dermatitis of childhood is particularly seen in children of Afro-Caribbean descent. This form has been given the acronym FACE – facial Afro-Caribbean childhood eruption.242.243. and 244. This term is no longer used because of its rare occurrence in non-black children. The term childhood granulomatous periorificial dermatitis is now preferred.245. and 246. Subtle clinical differences exist between this condition and perioral dermatitis and granulomatous rosacea, although it may still be a variant of one of these conditions. It has also been proposed as a childhood variant of lupus miliaris disseminatus faciei (see below). 247 It is benign, self-limited, and typically resolves within a year of onset without scarring. 245 Extrafacial lesions may occur.245. and 248. Its resolution seems to be hastened with the use of systemic antibiotics248 or with tacrolimus. 249
In many cases perioral dermatitis appears to be related to the application of one or more cosmetic preparations which may act by occlusion. 250 The use of strong topical corticosteroids, particularly fluorinated ones, may also have an etiological role.251.252. and 253. Various types of toothpaste have been implicated.254. and 255. Perioral dermatitis has been reported in renal transplant recipients maintained on oral corticosteroids and azathioprine. 256 It has also been associated with the wearing of the veil by Arab women. 257
Its relative rarity in patients with seborrheic dermatitis treated with corticosteroids has led to the postulate that perioral dermatitis may develop under fusiform-bacteria-rich conditions, rather than Malassezia-rich conditions as in the case of seborrheic dermatitis. 258
Topical metronidazole, erythromycin, and oral tetracyclines have been used as conventional treatments. Liquid nitrogen, benzoyl peroxide, and oral isotretinoin are other therapies. Recently, topical pimecrolimus has been used successfully. 259 Its efficacy has been confirmed by a randomized, vehicle-controlled study of 1% pimecrolimus cream. It was found to rapidly improve clinical symptoms, being most effective in corticosteroid-induced perioral dermatitis. 260
The histological changes in perioral dermatitis have been described as identical to those seen in rosacea.230. and 236. Others have found the epidermal changes to be more prominent than in rosacea, consisting of parakeratosis, often related to hair follicle ostia, spongiosis, which sometimes involves the hair follicle, and slight acanthosis. 261 The changes in the dermis are similar to those in papular rosacea and consist of perivascular or perifollicular infiltrates of lymphocytes and histiocytes and vascular ectasia. Uncommonly, an acute folliculitis is present. Tuberculoid granulomas have been described in the dermis in some series, but not in others. 261
In childhood granulomatous periorificial dermatitis, epithelioid granulomas are often perifollicular in distribution. This is not a feature of sarcoidosis. 245 Furthermore, the granulomas are more tuberculoid than sarcoidal in type.
Although the cause of lupus miliaris disseminatus faciei is unknown, it may be related to rosacea.262. and 263. It has also been called acne agminata and acnitis. 264 It is characterized by yellowish brown papules distributed over the central part of the face, including the eyebrows and eyelids. When widespread facial lesions are present, the appearances may mimic sarcoidosis. 265 Occasionally lesions occur elsewhere, including the axillae.266. and 267. The lesions last for months and heal with scarring. 268 This condition occurs in both sexes, predominantly in adolescents and young adults and rarely in the elderly.269. and 270. It has been suggested that as the currently used name is confusing, a new title should be substituted – FIGURE (facial idiopathic granulomas with regressive evolution). 271
Studies using PCR techniques have failed to demonstrate the DNA of M. tuberculosis in lesional skin. 272
Successful treatment with the 1450 nm diode laser has been reported recently. 273
There are few histopathological studies of this condition. 274 Biopsy appearances overlap those of both rosacea and perioral dermatitis. The characteristic lesion is an area of dermal necrosis, sometimes described as caseation necrosis, surrounded by epithelioid histiocytes, multinucleate giant cells and lymphocytes (Fig. 7.5). In many cases granulomas appear related to ruptured pilosebaceous units. 275 Nuclear fragments may be seen in the necrotic foci. Early lesions show superficial perivascular infiltrates of lymphocytes, histiocytes, and occasional neutrophils. Late lesions have these changes together with dermal fibrosis, particularly about follicles. Established lesions may show tuberculoid or suppurative granulomas. Demodex folliculorum were not seen in one study. 274 Small vessel changes with necrosis of blood vessel walls, thrombi, and extravasated red blood cells have also been described. 266 Acid-fast bacilli are not found in the areas of necrosis and there is no evidence that this condition is related to tuberculosis (see above).
Lupus miliaris disseminatus faciei. A shave biopsy of one of several papules near the lower eyelid. (H & E)
One study of lysozyme in these lesions suggests that there is an immunological mechanism involved in the pathogenesis of this condition rather than a foreign body reaction to an unidentified dermal agent. 276 Conversely, it has been suggested that the lesions represent a granulomatous reaction to damaged pilosebaceous units. 277
Non-caseating granulomas of tuberculoid type may be found, rarely, in the dermis and subcutis in Crohn’s disease (see p. 493). The term metastatic Crohn’s disease is often used for the presence of multiple cutaneous lesions. 278 Granulomas are not uncommon in the wall of perianal sinuses and fistulas. A granulomatous cheilitis has also been reported (see p. 188). 279 It is important to exclude Crohn’s disease in cases of apparent Melkersson–Rosenthal syndrome. 280
There is even a report of cutaneous granulomas developing in a patient with histologically proven ulcerative colitis. 281
The term ‘necrobiosis’ has been retained here because of common usage and refers to areas of altered dermal connective tissue in which, by light microscopy, there is blurring and loss of definition of collagen bundles, sometimes separation of fibers, a decrease in connective tissue nuclei, and an alteration in staining by routine histological stains, often with increased basophilia or eosinophilia. The term ‘collagenolytic’ granuloma is favored by others. 282 Granular stringy mucin is sometimes seen in such areas in granuloma annulare, and fibrin may be seen in rheumatoid nodules. Necrobiotic areas are partially or completely surrounded by a histiocytic rim which may include multinucleate giant cells. In some cases histiocytes become more spindle-shaped and form a ‘palisade’.
Necrobiotic (collagenolytic) granulomas283 are found in the following conditions:
• granuloma annulare and its variants
• necrobiosis lipoidica
• necrobiotic xanthogranuloma
• rheumatoid nodules
• rheumatic fever nodules
• reactions to foreign materials and vaccines
• miscellaneous diseases.
Granuloma annulare is a dermatosis, usually self-limited, of unknown etiology and characterized by necrobiotic (collagenolytic) dermal papules that often assume an annular configuration. 284 Either the skin or the subcutis, or both, may be involved. The clinical variants of granuloma annulare include localized, generalized, perforating, 285 and subcutaneous or deep forms.286. and 287. Rare types include a follicular pustulous variant, 288 an acute-onset, painful acral form, 289 and a patch form, 290 although the latter cases are probably examples of the interstitial granulomatous form of drug reaction (see p. 192). The linear variant reported some years ago would now be regarded as a variant of interstitial granulomatous dermatitis (see p. 191). 291 Classic granuloma annulare was preceded in one case by the development of a severe linear form along Blaschko’s lines. 292
In the localized form, one or more erythematous or skin-colored papules are found. Grouped papules tend to form annular or arciform plaques. The hands, feet, arms, and legs are the sites of predilection in some 80% of cases. 293 A papular umbilicated form has been described in children in which grouped umbilicated flesh-colored papules are limited to the dorsum of the hands and fingers. 294 The generalized form accounts for approximately 15% of cases.284. and 295. Multiple macules, papules, or nodules are distributed over the trunk and limbs. 296 Rarely, there may be confluent erythematous patches or plaques.297. and 298. The appearances may even simulate mycosis fungoides. 299 It has been reported as a side effect of allopurinol300 and of amlodipine. 301 Lesions in perforating granuloma annulare are grouped papules, some of which have a central umbilication with scale. 302 The extremities are the most common site. The generalized form may also have perforating lesions. 303 A high incidence of perforating granuloma annulare has been reported in Hawaii. 304 It is rare in infants and young children. 305 In subcutaneous (or deep) granuloma annulare, deep dermal or subcutaneous nodules are found on the lower legs, hands, head, and buttocks.306. and 307. These lesions are associated with superficial papules in 25% of cases. 308 This group also includes those lesions described as pseudorheumatoid nodules, palisading subcutaneous granuloma, and benign rheumatoid nodules.309.310. and 311. Although arthritis does not usually occur in children with these nodular lesions, IgM rheumatoid factor has been found in serum in some cases.312. and 313. There is a report of one case occurring in association with juvenile rheumatoid arthritis. 311 Computed tomography (CT) scan changes of this variant have been described. 314 Rarely, the changes may involve deeper soft tissues and produce a destructive arthritis and limb deformity. 315 Pseudorheumatoid nodules have also been reported in adults. A recent series of 14 cases all involved females and most involved the small joints of the hand. 316 Granuloma annulare was present at the periphery of the nodules in eight cases. 316 The authors suggested the term juxta-articular nodular granuloma annulare for these cases. 316
Granuloma annulare has been reported as a seasonal eruption on the elbows or hands317. and 318. and from unusual sites such as the penis,319.320.321. and 322. palms, 323 about the eyes,324.325.326. and 327. and ear.328. and 329. There has been one case of cutaneous granuloma annulare associated with histologically similar intra-abdominal visceral lesions in a male with insulin-dependent diabetes. 330
Females are affected more than twice as commonly as males. The localized and deep forms are more common in children and young adults.307. and 331. The deep (subcutaneous) form has been reported as a congenital lesion. 332 Generalized granuloma annulare occurs most frequently in middle-aged to elderly adults. Most cases of granuloma annulare are sporadic but familial cases have occasionally been reported. 333 Patients with the generalized form of the disease show a significantly higher frequency of HLA-BW35 compared with controls and with those who have the localized form of the disease. 334
Lesions of granuloma annulare have a tendency to regress spontaneously; however, about 40% of cases recur. 293 Resolution of lesions subject to biopsy, but not other lesions has been reported. 335 Spontaneous regression of localized lesions in children occurred, in one series, from 6 months to 7 years, with a mean of 2.5 years. 336 In the generalized form, the clinical course is chronic with infrequent spontaneous resolution and poor response to therapy. 296 Non-perforating lesions are usually asymptomatic. 337
Although the etiology and pathogenesis of the skin lesions in granuloma annulare remain uncertain, possible triggering events include insect bites, trauma, the presence of viral warts, drugs, erythema multiforme, and exposure to sunlight.301.338.339. and 340. Lesions have occurred in the scars of herpes zoster, localized or generalized,341.342.343.344.345. and 346. in a saphenectomy scar, 347 in a Becker’s nevus, 348 and at the sites of tuberculin skin tests. 349 The possible link between both the localized and generalized forms and diabetes mellitus remains controversial. There is more convincing evidence of this association with the generalized form than with the localized form although there may be a weak association with nodular as opposed to the annular type of localized lesion.350.351. and 352. Significantly lower serum insulin levels have been found in children with multiple lesions of granuloma annulare. 353 A case-control study failed to find any association between granuloma annulare and type 2 diabetes mellitus. 354 Reported cases of the concurrence of these two diseases may represent the chance association of two not uncommon conditions. 355 It has been reported in association with sarcoidosis, 356 Alagille syndrome, 357 toxic adenoma of the thyroid, 358 autoimmune thyroiditis,359. and 360. uveitis, 361 hepatitis B362 and C infection, 363 parvovirus B19 infection, 364 BCG, 365 hepatitis B, 366 and antitetanus vaccination,367. and 368. waxing-induced pseudofolliculitis, 369 tuberculosis,370. and 371. tattoos, 372 granulomatous mycosis fungoides, 373 a monoclonal gammopathy, 374 hypercalcemia, 375 myelodysplastic syndrome, 376 chronic myelomonocytic leukemia, 377 Hodgkin’s lymphoma, non-Hodgkin’s lymphoma, gastrointestinal stromal tumor, 378 and metastatic adenocarcinoma.379.380.381.382.383.384.385.386.387. and 388. In these conditions, the clinical presentation may be atypical. 389 Localized, generalized, and perforating forms of granuloma annulare have been reported in patients with AIDS; the generalized form is the most common clinical pattern.390.391.392.393.394.395.396.397.398. and 399. It may, rarely, be the presenting complaint in AIDS. 400Bartonella infection has not been detected in lesions of granuloma annulare. 401 Interstitial granuloma annulare has been reported in borreliosis, 402 but it may represent a pattern related to the Borrelia infection itself.
It has been suggested that the underlying cause of the necrobiotic granulomas is an immunoglobulin-mediated vasculitis. 403 In a recent study, neutrophils and neutrophil fragments were commonly present in early lesions but a true vasculitis was rare. Direct immunofluorescence studies did not demonstrate immune deposits in vessel walls. 404 Other studies have stressed the importance of cell-mediated immune mechanisms with a delayed hypersensitivity reaction of T helper (Th) 1 type against as yet undefined antigens.405. and 406. This is supported by the finding of increased levels of interleukin (IL)-18, interferon gamma, and IL-2 in lesional skin. 407 Collagen synthesis is increased in the lesions of granuloma annulare, probably representing a reparative phenomenon. 408
There is no therapy of choice for granuloma annulare, and the most widely used drugs are topical and systemic corticosteroids, but they are not always effective, and relapses may occur when they are discontinued. 406 Other therapies have included cryosurgery, laser, 409 retinoids, 410 vitamin E and a 5-lipoxygenase inhibitor, 411 dapsone, chloroquine, ultraviolet A1 phototherapy,406. and 412. and narrowband ultraviolet B therapy. 413 A combination of systemic isotretinoin and topical pimecrolimus 1% cream has been used successfully in the generalized form. 414 Imiquimod cream has been used but it produced considerable localized inflammation. 415 T-cell directed therapies such as infliximab, efalizumab, and etanercept have been used in recalcitrant cases.407. and 416. Hydroxyurea may be a viable option for the treatment of recalcitrant cases of disseminated disease. 417
Three histological patterns may be seen in granuloma annulare – necrobiotic (collagenolytic) granulomas, an interstitial or ‘incomplete’ form, and granulomas of sarcoidal or tuberculoid type. The third of these patterns is uncommon. 418 In most histopathological studies, the interstitial form is most common. 419
In the form with necrobiotic (collagenolytic) granulomas, one or more areas of necrobiosis, surrounded by histiocytes and lymphocytes, are present in the superficial and mid dermis (Fig. 7.6). The peripheral rim of histiocytes may form a palisaded pattern (Fig. 7.7). Variable numbers of multinucleate giant cells are found in this zone. Some histiocytes have an epithelioid appearance. An increased mitotic rate is found in the histiocytes in some cases. 420 The histiocytes are CD68+. 299 Surprisingly, in one series, the histiocytic component of the infiltrate stained only for vimentin and lysozyme and not the other common histiocyte markers (HAM56, CD68 (KP1), Mac-387, and factor XIIIa). 421 PGM1, the most specific histiocytic marker, is strongly expressed in all cases.422. and 423. The intervening areas of the dermis between the necrobiotic granulomas are relatively normal compared with necrobiosis lipoidica, and there is no fibrosis. A perivascular infiltrate of lymphocytes and histiocytes is also present; eosinophils are found in 40–66% of cases but plasma cells are rare.424. and 425. In contrast, plasma cells are not uncommon in necrobiosis lipoidica. The central necrobiotic areas contain increased amounts of connective tissue mucins which may appear as basophilic stringy material between collagen bundles. Neutrophils and nuclear dust contribute to the basophilic appearance. Based on these changes, Lynch and Barrett have classified granuloma annulare as a ‘blue’ granuloma, in contrast to the ‘red’ necrobiotic (collagenolytic) granulomas in which fibrin, eosinophils, or flame figures contribute to an eosinophilic appearance.282. and 426. Although this is an oversimplification of a sometimes difficult assessment, the various ‘blue’ and ‘red’ granulomas are listed in Table 7.2. Special stains such as colloidal iron and Alcian blue aid in the demonstration of mucin. Heparan sulfate is present in addition to hyaluronic acid.427. and 428. Elastic fibers may be reduced, absent, or unchanged in the involved skin.429. and 430. The colocalization of granuloma annulare and mid-dermal elastolysis has been reported. 431
Granuloma annulare. The inflammatory cell infiltrate surrounds the area of ‘necrobiosis’ (collagenolysis) on all sides. It is not ‘open ended’ as in necrobiosis lipoidica. (H & E)
Granuloma annulare. (A) A palisade of inflammatory cells surrounds the central zone of ‘necrobiosis’ (collagenolysis). (B) There is some nuclear dust within this central zone. (H & E)
Occasionally, neutrophils or nuclear fragments are present in necrobiotic areas. 404 In the rare follicular-pustulous form there are neutrophils in the upper portion of the follicles leading to pustule formation. 288 Palisading necrobiotic granulomas surround hair follicles. 432 An acute or subacute vasculitis has been described in or near foci of necrobiosis, associated with varying degrees of endothelial swelling, necrosis of vessel walls, fibrin exudation, and nuclear dust. 403
The lesions of subcutaneous or deep granuloma annulare have areas of necrobiosis which are often larger than in the superficial type (Fig. 7.8). These foci are distributed in the deep dermis, subcutis and, rarely, deep soft tissues.315. and 433. There may be overlying superficial dermal lesions. Eosinophils are said to be more common in this variant than in the superficial lesions.
Subcutaneous granuloma annulare. There are large areas of ‘necrobiosis’ surrounded by a palisade of lymphocytes and histiocytes. (H & E)
In the juxta-articular nodular form of granuloma annulare (pseudorheumatoid nodules) there are deep dermal nodules with subcutaneous extension composed of epithelioid granulomas separated by thickened collagen bundles. Eosinophilic material, composed predominantly of collagen, is surrounded by histiocytes in a palisaded array. This contrasts with rheumatoid nodules where the central material is fibrin, and the usual form of granuloma annulare, in which it is mucin. Scanty mucin is often present in this juxta-articular form. The interstitial form of granuloma annulare is present next to the nodules in about half of the cases, further support for the notion that the nodular lesions are a form of granuloma annulare. 316
In the disseminated form of granuloma annulare, the granulomatous foci are often situated in the papillary dermis (Fig. 7.9). Necrobiosis may be inconspicuous. There is some superficial resemblance to lichen nitidus (see p. 45), although in disseminated granuloma annulare there are no acanthotic downgrowths of the epidermis at the periphery of the lesions.
Disseminated granuloma annulare with involvement of the papillary dermis. There are no acanthotic downgrowths of rete pegs at the margins of the inflammatory focus, as seen in lichen nitidus. ‘Necrobiosis’ may be subtle in this form of granuloma annulare. (H & E)
In the interstitial or ‘incomplete’ form of granuloma annulare, the histological changes are subtle and best assessed at lower power. The dermis has a ‘busy’ look due to increased numbers of inflammatory cells, mainly histiocytes and lymphocytes (Fig. 7.10). They are arranged about vessels and between collagen bundles which are separated by increased connective tissue mucin. There are no formed areas of necrobiosis. In some cases the interstitial component is minimal. A similar appearance can be seen in the interstitial granulomatous drug reaction (see p. 192) although in the latter condition true necrobiosis is uncommon, and, if present, localized. Furthermore, eosinophils are often present and there may be lichenoid changes at the dermal–epidermal interface. In interstitial granulomatous dermatitis there are both neutrophils and eosinophils in the infiltrate, although both cell types may be sparse. Another characteristic feature is the presence of a palisade of histiocytes around one or many collagen fibers, which often have a basophilic hue. Rarely, Mycobacterium marinum infection of the skin may mimic interstitial granuloma annulare. 434 It is uncertain whether the cases of this type of granuloma annulare associated with borreliosis are mimics or true examples of granuloma annulare. 402 Other mimics include granulomatous mycosis fungoides and B-cell lymphoma. 435 Negative staining for both hemosiderin and human herpesvirus 8 can be used to distinguish interstitial granuloma annulare from early Kaposi’s sarcoma in which both are usually positive. 436
(A) Granuloma annulare of ‘incomplete’ type. (B) The dermis is hypercellular (a so-called ‘busy dermis’). (H & E) (C) There is an increased amount of interstitial mucin. (Alcian blue)
Cases of the non-necrobiotic sarcoidal or tuberculoid type of granuloma annulare are uncommon and pose a diagnostic problem. The presence of increased dermal mucin or eosinophils may be helpful distinguishing features (Fig. 7.11). Eosinophils and obvious mucin are not seen in sarcoidosis. 424 However, granuloma annulare and sarcoidosis have been reported in the same patient. 437
Sarcoidal granuloma annulare. A single field can closely resemble sarcoidosis, although the granuloma is not completely ‘naked’. (H & E)
In most cases of granuloma annulare, the epidermal changes are minimal. Perforating lesions have a central epidermal perforation which communicates with an underlying necrobiotic granuloma (Fig. 7.12). At the edges of the perforation there are varying degrees of downward epidermal hyperplasia to form a channel. The channel contains necrobiotic material and cellular debris. There is surface hyperkeratosis. 285 The lesions sometimes perforate by way of a hair follicle. 438 Pustules are a very rare finding in the perforating variant. 288
Perforating granuloma annulare. (H & E)
Immunofluorescence studies have shown fibrin in areas of necrobiosis. 437 IgM and C3 were present in blood vessel walls in one series. 403 Immunoperoxidase techniques have demonstrated activated T lymphocytes with an excess of helper/inducer phenotype (CD4+) and CD1-positive dendritic cells related to Langerhans cells in the perivascular and granulomatous infiltrates. 405 In contrast, lymphocytes were predominantly of CD8 type in a patient with HIV infection. 439 A study of the staining pattern of lysozyme in the inflammatory cell infiltrate suggests that this may be useful in distinguishing granuloma annulare from other necrobiotic granulomas. 440 The distribution of the inhibitor of metalloproteinase-1 is different in granuloma annulare and necrobiosis lipoidica. 441
Ultrastructural studies have confirmed the presence of histiocytes in the dermal infiltrate together with cellular debris and fibroblasts. Degenerative changes in collagen in areas of necrobiosis include swelling, loss of periodic banding, and fragmentation of fibers. Elastic fibers also show degenerative changes. Fibrin and other amorphous material is present in interstitial areas. 442
Necrobiosis lipoidica was originally called ‘necrobiosis lipoidica diabeticorum’ but, although some cases are associated with diabetes mellitus,443. and 444. it is not peculiar to diabetes. 445 In one series only 11% of patients with necrobiosis lipoidica had diabetes mellitus at presentation, while a further 11% developed impaired glucose tolerance/diabetes in the succeeding 15 years. 446 The incidence in diabetics is low – approximately 3 cases per 1000. 443 It is even lower in childhood diabetes. 447
The legs, particularly the shins, are overwhelmingly the commonest site of involvement, but lesions may also occur on the forearms, hands, and trunk. Unusual sites include the nipple, penis, surgical scars, and a lymphedematous arm.448.449.450.451.452. and 453. Three-quarters of cases are bilateral at presentation and many more become bilateral later. Lesions may be single but are more often multiple. Diffuse disease is rare. 454 Females are affected more than males in a ratio of 3 to 1. The average age of onset in one series was 34 years, but the condition may be seen in children.455. and 456. It has occurred in monozygotic twins, but not until adult life. 457
The earliest lesions are red papules which enlarge radially to become patches or plaques with an atrophic, slightly depressed, shiny yellow-brown center and a well-defined raised red to purplish edge. Nodules are uncommon. 458 Some lesions resolve spontaneously but many are persistent and chronic and may ulcerate;459.460. and 461. this occurred in 13% of cases in one series. 462 Rarely, squamous cell carcinoma may arise in long-standing lesions.463.464.465.466.467. and 468. The simultaneous occurrence of necrobiosis lipoidica with granuloma annulare469. and 470. and with sarcoidosis has been reported.471. and 472. It has also been associated with autoimmune thyroid disease, scleroderma, rheumatoid arthritis, and jejunoileal bypass surgery. 473 The case reported in association with light-chain-restricted plasma cellular infiltrates473. and 474. has been questioned by others as not representing necrobiosis lipoidica. 475
The association of these lesions with diabetes has already been referred to but the role of this metabolic disorder in the development of the cutaneous lesions is not understood. Diabetic vascular changes may be important: in some early lesions a necrotizing vasculitis has been described. 476 Lesions show increased blood flow, refuting the hypothesis that the disease is a manifestation of ischemic disease. 477 The finding in areas of sclerotic collagen of Glut-1, a protein responsible for glucose transport across epithelial and endothelial barrier tissue, raises the possibility that a disturbance in glucose transport by fibroblasts may contribute to the histological findings. 478 Adults and children with insulin-dependent diabetes mellitus and necrobiosis lipoidica are at high risk for diabetic nephropathy and retinopathy. 479 The recent detection of spirochetal organisms in patients with this disease from central Europe, by focus floating microscopy, points to an involvement of B. burgdorferi or other strains in the development of this disease. 480
The treatment of necrobiosis lipoidica is suboptimal. It has included topical and intralesional steroids, antiplatelet drugs such as aspirin and ticlopidine, and drugs that decrease blood viscosity such as pentoxifylline. 481 Thalidomide, 481 topical PUVA therapy, 482 UVA1 phototherapy, 483 photodynamic therapy, 484 methotrexate, 485 topical granulocyte-macrophage colony-stimulating factor (GM-CSF), 486 and pioglitazone487 have all been used with some improvement of the disease. Antimalarial agents such as chloroquine and hydroxychloroquine have resulted in the clearance of lesions, particularly if used in the early stages of their evolution. 488
The histopathological changes in necrobiosis lipoidica involve the full thickness of the dermis and often the subcutis (Fig. 7.13). Early lesions are not often biopsied. They are said to show a superficial and deep perivascular and interstitial mixed inflammatory cell infiltrate in the dermis. Similar changes are present in septa of adipose tissue. A necrotizing vasculitis with adjacent areas of necrobiosis and necrosis of adnexal structures has also been seen. 476
Necrobiosis lipoidica. There is involvement of the full thickness of the dermis with extension into the subcutis. (H & E)
In active chronic lesions there is some variability between cases. The characteristic changes are seen at the edge of the lesions. These changes involve most of the dermis but particularly its lower two-thirds. Areas of necrobiosis may be extensive or slight: they are often more extensive and less well defined than in granuloma annulare (Fig. 7.14). The intervening areas of the dermis are also abnormal. Histiocytes, including variable numbers of multinucleate Langhans or foreign body giant cells, outline the areas of necrobiosis. The necrobiosis tends to be irregular and less complete than in granuloma annulare. There is a variable amount of dermal fibrosis and a superficial and deep perivascular inflammatory reaction which, in contrast to the usual picture in granuloma annulare, includes plasma cells (Fig. 7.15). Occasional eosinophils may be present. 424 In some cases necrobiotic areas are less frequent and there are collections of epithelioid histiocytes and multinucleate cells, particularly about dermal vessels. The dermal changes extend into the underlying septa of the subcutis and into the periphery of fat lobules. This septal panniculitis may resemble erythema nodosum but in that condition there are no significant dermal changes. Lymphoid cell aggregates, containing germinal centers, are present in the deep dermis or subcutis in approximately 10% of cases of necrobiosis lipoidica. 489
Necrobiosis lipoidica. There are several layers of ‘necrobiosis’ within the dermis. (H & E)
(A) Necrobiosis lipoidica. (B) A perivascular inflammatory cell infiltrate is present in the dermis. There is ‘necrobiosis’ of the adjacent collagen. (H & E)
In old atrophic lesions and in the center of plaques there is little necrobiosis and much dermal fibrosis. The underlying subcutis is also fibrotic. Elastic tissue stains demonstrate considerable loss of elastic tissue. Scattered histiocytes may be present.
The presence of lipid in necrobiotic areas (demonstrated by Sudan stains) has been used in the past to distinguish necrobiosis lipoidica from granuloma annulare, but subsequent studies have also shown lipid droplets in granuloma annulare. 430 Cholesterol clefts may be present, uncommonly, in areas of necrobiosis.448. and 490. Rarely they are a conspicuous feature.458. and 491. Fibrin can also be demonstrated in necrobiotic areas. 444 There may be small amounts of mucin in the affected dermis but the presence of large amounts in areas of necrobiosis favors a diagnosis of granuloma annulare.
Vascular changes are more prominent in necrobiosis lipoidica, particularly in the deeper vessels. 283 These range from endothelial swelling to a lymphocytic vasculitis and perivasculitis. Epithelioid granulomas may be present in the vessel wall or adjacent to it. In old lesions the wall may show fibrous thickening. The smaller, more superficial vessels are increased in number and telangiectatic. Apart from atrophy and ulceration, epidermal changes are unremarkable in necrobiosis lipoidica. Transepidermal elimination of degenerate collagen has been reported;491. and 492. it may be associated with focal acanthosis or pseudoepitheliomatous hyperplasia. Transfollicular elimination also occurs. 493
Although in most cases it is possible to distinguish necrobiosis lipoidica from granuloma annulare, there are cases in which this is difficult both clinically and histologically. 444 There may also be difficulties distinguishing between necrobiosis lipoidica and necrobiotic xanthogranuloma (see below). Cholesterol clefts and transepidermal elimination may occur in both these conditions. Clinical features are usually distinctive in necrobiotic xanthogranuloma but not all cases are associated with paraproteinemia or a periorbital distribution of lesions.490. and 494.
Immunofluorescence studies have demonstrated IgM and C3 in the walls of blood vessels in the involved skin. Fibrin is seen in necrobiotic areas. IgM, C3, and fibrinogen may be present at the dermoepidermal junction. 495
Necrobiotic xanthogranuloma is a rare condition characterized by the presence of violaceous to red, partly xanthomatous plaques and nodules; there is a predilection for the periorbital area. A paraproteinemia is often present. The clinical course is chronic. It is discussed further in Chapter 40, page 958.
There are broad zones of hyaline necrobiosis as well as granulomatous foci composed of histiocytes, foam cells, and multinucleate cells (Fig. 7.16). The amount of xanthomatization is variable. Distinction from necrobiosis lipoidica is sometimes difficult on a small biopsy, but the clinical features of these two conditions are quite different.
Necrobiotic xanthogranuloma. The ‘necrobiosis’ is only focal. Numerous giant cells are present. (H & E)
Skin manifestations, including rheumatoid nodules, are relatively common in rheumatoid arthritis.498. and 499. These nodules occur in approximately 20% of patients, usually in the vicinity of joints. Sited primarily in the subcutaneous tissue, they may involve the deep and even the superficial dermis. They vary from millimeters to centimeters in size and consist of fibrous white masses in which there are creamy yellow irregular areas of necrobiosis. Old lesions may have clefts and cystic spaces in these regions. It is most probable that rheumatoid nodules result from a vasculitic process; however, even in very early lesions such a change may be difficult to demonstrate. 500 Nodules usually persist for months to years. Rarely, similar lesions occur in systemic lupus erythematosus.501.502. and 503.
Multiple small nodules may develop on the hands, feet, and ears during methotrexate therapy. 504 This event is known as ‘accelerated rheumatoid nodulosis’. The term rheumatoid nodulosis has also been used for the presence of subcutaneous rheumatoid nodules with recurrent articular symptoms but no significant synovitis. The rheumatoid factor is often negative.505. and 506. The distinction of this entity from juxta-articular pseudorheumatoid nodules is problematic. 506
There are one or more irregular areas of necrobiosis in the subcutis and dermis (Fig. 7.17). These areas are surrounded by a well-developed palisade of elongated histiocytes, with occasional lymphocytes, neutrophils, mast cells, and foreign body giant cells. 507 The central necrobiotic focus is usually homogeneous and eosinophilic. 508 There is sometimes obvious fibrin. In contrast, the areas of necrobiosis in the subcutaneous or deep variant of granuloma annulare are often pale and mucinous with a tendency to basophilia. Old rheumatoid nodules may show areas of dense fibrosis, clefts, and ‘cystic’ degeneration of the necrobiotic foci. The dermis and subcutis surrounding the necrobiotic granulomas show a perivascular round cell infiltrate which includes plasma cells. Eosinophils may be present. Uncommonly, an acute vasculitis is seen in the surrounding vessels and sometimes a necrotic blood vessel associated with nuclear fragments or sparse neutrophils may be seen in the center of areas of necrobiosis. Occasionally, a superficial nodule may perforate the epidermis. 509
(A) Rheumatoid nodule. (B) A palisade of elongate histiocytes surrounds a zone of ‘necrobiosis’. (H & E)
Fibrin is present in the center of the necrobiotic areas. 510 Rarely, immunoglobulins and complement have been demonstrated in vessels exhibiting a vasculitis. It is unusual to find mucin in necrobiotic foci in rheumatoid nodules, and this is the single most useful feature in distinguishing these lesions from the deep variant of granuloma annulare. 508 In some cases of deep granuloma annulare the changes are very similar to those of rheumatoid nodules; clinical information is most helpful in these instances.
With the decline in the prevalence of rheumatic fever in developed countries, rheumatic nodules are now rarely seen or biopsied. Consequently, most histological studies are found in the older literature. 511 Nodules are more common in children than adults and are usually associated with acute rheumatic carditis. They are usually asymptomatic and are distributed symmetrically over bony prominences, particularly at the elbows. 512 Their size ranges from a few millimeters to 2–3 centimeters in diameter. The lesions, unlike rheumatoid nodules, last for only a short time and eventually involute. 511
Rheumatic nodules form in the subcutis or in the tissue deep to it. They include one or more foci of altered collagen (fibrinoid necrosis or fibrinoid change): this change is characterized by separation and swelling of the collagen bundles and increased eosinophilia. These foci may contain scattered inflammatory cells512 or cell debris511 and are surrounded by histiocytes, sometimes arranged in palisaded array. 511 Multinucleate histiocytes may be seen. A mixed inflammatory cell infiltrate is present at the periphery of these areas and around the vessels. Lipid may be seen in histiocytes about the altered collagen. 511 Apparent differences in the published histological description of these lesions may reflect differences in their age, early lesions being more exudative. A study of 40 rheumatic fever nodules, including ultrastructural features of two cases, has been published from India. 513
Purified bovine collagen is currently being used, in the form of intracutaneous injections, to treat certain forms of superficial scarring (see p. 394). In some persons this results in a granulomatous reaction resembling granuloma annulare. There are irregular foci of eosinophilic necrobiosis surrounded by a palisading rim of multinucleate and mononuclear histiocytes, with lymphocytes and plasma cells. 514
Areas of necrobiosis associated with a granulomatous reaction have also been described, rarely, in association with Trichophyton rubrum, and with the presence of splinters of wood and suture material (Fig. 7.18).515.516. and 517. Necrobiotic areas are also seen in cutaneous berylliosis. Changes which superficially resemble necrobiotic granulomas are also seen in injection sites of drugs of abuse. 518
Suture granuloma. There is a palisaded, centrally ‘necrobiotic’ granuloma to foreign material. (H & E)
Children with ataxia telangiectasia may present with erythematous plaques which on histopathological examination show necrobiotic granulomas. As with other immunodeficiency diseases, granulomas of other types are often present. Tuberculoid and sarcoidal granulomas have also been reported in ataxia telangiectasia. 521
Necrobiotic granulomas have also been reported in parvovirus B19 infection. 364 There is some resemblance to the lesions of granuloma annulare. At other times the pattern is more like interstitial granulomatous dermatitis.
The extravascular granulomas of Churg–Strauss (allergic) granulomatosis and of Wegener’s granulomatosis may have necrobiotic features. They are mentioned here for completeness, but they are considered further in Chapter 8, pages 239–241. Necrobiotic granulomas are a rare manifestation of systemic lymphoma. 20
Finally, Crohn’s disease of so-called metastatic type may have necrobiotic granulomas. 522
The suppurative granulomas consist of collections of epithelioid histiocytes, with or without multinucleate giant cells, in the centers of which are collections of neutrophils (Fig. 7.19). Most of the conditions included in this group are discussed in other chapters and only the major differential histological features will be noted here.
Sporotrichosis. A suppurative granuloma is present. (H & E)
Suppurative granulomas are seen in the following conditions:
• chromomycosis and phaeohyphomycosis
• sporotrichosis
• non-tuberculous mycobacterial infections
• blastomycosis
• paracoccidioidomycosis
• coccidioidomycosis
• blastomycosis-like pyoderma
• mycetoma, nocardiosis, and actinomycosis
• cat-scratch disease
• lymphogranuloma venereum
• pyoderma gangrenosum
• ruptured cysts and follicles.
The first seven conditions listed above show very similar histological changes. These include marked irregular epidermal hyperplasia (‘pseudoepitheliomatous’ hyperplasia), intraepidermal and dermal microabscesses, suppurative granulomas, and a mixed inflammatory cell infiltrate which includes scattered multinucleate giant cells. Specific diagnosis depends on identification of the causative agent in tissue sections or by culture. Similar changes are seen in halogenodermas but granulomas and giant cells are not seen, except in relation to ruptured hair follicles. It is necessary to cut multiple sections and carefully examine them for microorganisms when such a histopathological pattern is seen. Most organisms can be seen in routine histological sections if care is taken, but stains for fungi (for example, the PAS and Grocott methenamine silver methods) and mycobacteria may reveal organisms that escape detection in hematoxylin and eosin preparations.
In chromomycosis the characteristic organisms are round to oval thick-walled brown cells about 6–12 µm in diameter (sclerotic bodies, Medlar bodies). Intracellular septation may be seen. Single organisms or small groups are found within multinucleate giant cells, within microabscesses, suppurative granulomas, or surface crust. Tuberculoid granulomas are occasionally seen in the dermal infiltrate. 523 In phaeohyphomycosis, which is clinically distinct from chromomycosis, there are hyphal and yeast forms in suppurative granulomas. Species identification requires culture of the organism. Chromomycosis and phaeohyphomycosis are discussed further in Chapter 25, pages 596–598.
The causative organism, Sporothrix schenckii, is present in the lesions of primary cutaneous sporotrichosis (see p. 598) in the yeast form; it is only rarely found in its hyphal form. The formation of sporothrix asteroids by the encasement of individual yeast cells by a deposit of immune complexes and fibrin is an occasional finding. These asteroids are seen infrequently in sporotrichotic lesions in some parts of the world, but are comparatively common in those seen in Australia and South Africa. 524 The yeast cells are small, round to oval structures, some of which show budding. They may be found within giant cells or in suppurative granulomas. They are difficult to see and may require PAS stains for recognition. The asteroids are found only in microabscesses and the centers of suppurative granulomas. They can be recognized in these locations on careful study of hematoxylin and eosin preparations. Generally, organisms are few in sporotrichosis.
Tuberculoid or suppurative granulomas may be seen in infections caused by non-tuberculous mycobacteria, including M. marinum and M. chelonae (see p. 559). In M. marinum infections, caseation is not usually seen. Organisms are sparse; when found, they are usually within histiocytes. Organisms may be moderately plentiful in M. chelonae infections. They are frequently seen in and about round to oval clear spaces in the center of suppurative foci.
Rarely these infections may present with a lichenoid as well as a granulomatous dermatitis. 525
In the disseminated form of blastomycosis the organisms are scarce and are found either within giant cells or free in the dermis (see p. 594). The organism (Blastomyces dermatitidis) is a thick-walled round cell, 8–15 µm in diameter. Multiple nuclei may be seen in the cell. Single broad-based buds are occasionally present on the surface. PAS or Grocott methenamine silver stains facilitate demonstration of the organism.
Most cutaneous lesions in paracoccidioidomycosis (‘South American blastomycosis’) are secondary lesions seen in the course of the disseminated form of the disease (see p. 595). The causative agent, Paracoccidioides brasiliensis, is usually found in giant cells. The organisms vary more in size than Blastomyces dermatitidis and can be larger. Also, P. brasiliensis is thin walled, lacks multiple nuclei, and often has multiple buds arranged round the mother cell.
The cutaneous lesions of coccidioidomycosis are almost always secondary to pulmonary disease (see p. 594). Areas of necrosis are sometimes present in the dermis. Sporangia of Coccidioides immitis are rounded structures, 10–80 µm in diameter, which contain multiple sporangiospores, 1–5 µm in diameter. Sporangia are usually easily identified in sections stained with hematoxylin and eosin. Spherules and sporangiospores stain with silver stains. Sporangiospores are PAS positive whereas spherules may be negative or only weakly positive. 526
Marked epidermal hyperplasia and epidermal, follicular and dermal abscesses are seen in blastomycosis-like pyoderma (see p. 553). There is usually severe solar elastosis. In some cases a palisading rim of histiocytes is seen surrounding the suppurative foci in the dermis. Multinucleate giant cells are occasionally present in this zone but they are not as common as in the mycoses discussed above. Bacteria, particularly Gram-positive cocci, may be seen in suppurative foci. Staphylococcus aureus is often isolated from tissue samples but not from the skin surface.
In mycetomas, nocardiosis, and actinomycosis, foci of suppuration may become surrounded by a histiocytic rim to form suppurative granulomas. Organisms are present within the suppurative foci. These conditions are discussed in Chapter 25, pages 600–602.
Superficial granulomatous pyoderma is a variant of pyoderma gangrenosum (see p. 237) which has a more indolent course than classic pyoderma gangrenosum.528. and 529. One group has suggested that this condition would be better called ‘pathergic granulomatous cutaneous ulceration’. 530 Unlike the typical pyoderma gangrenosum, there are suppurative granulomas and scattered multinucleate giant cells in the dermis associated with irregular epidermal hyperplasia, sinus formation, fibrosis, and a heavy mixed inflammatory infiltrate which includes plasma cells and eosinophils.529. and 531. The histological changes mimic an infectious process but the lesions respond to corticosteroid therapy and not antibiotics.
Occasionally suppurative granulomas are seen adjacent to ruptured cysts (epidermal and dermoid cysts, in particular) and to inflamed hair follicles which rupture, liberating their contents into the dermis.
The essential feature of foreign body granulomas is the presence either of identifiable exogenous (foreign) material or of endogenous material which has become altered in some way so that it acts as a foreign body. Around this material are arranged histiocytes (including epithelioid histiocytes), multinucleate giant cells derived from histiocytes, and variable numbers of other inflammatory cells. Multinucleate giant cells are often of foreign body type, with nuclei scattered irregularly throughout the cytoplasm, but Langhans giant cells are also seen. In some cases the reaction consists almost entirely of multinucleate cells. Where there are moderate to large amounts of foreign material, histiocytes are sometimes arranged in an irregular palisade. Some foreign materials, e.g. tattoo pigment, induce granulomas of different types. The causative agent may or may not be birefringent when sections are examined in polarized light.
Foreign body granulomas are formed around such disparate substances as starch, 532 talc, 533 tattoo material (Fig. 7.20),177. and 534. cactus bristles, 535 wood splinters, suture material, retained epicardial pacing wires,536. and 537. Bioplastique, Dermalive and Artecoll microimplants,538.539.540. and 541. injected mineral oil, 542 injected hyaluronic acid,543.544.545. and 546. pencil lead, 547 bovine collagen, 548 artificial hair, 549 golf club graphite, 550 fragments of a chain saw blade, 551 and insect mouth parts. 552 Some foreign materials such as glass, zirconium, 553 beryllium, acrylic fibers, and tattoo pigments may induce local sarcoidal granulomas (see p. 173). Tuberculoid granulomas have been reported in one patient at the site of injection of zinc-containing insulin. 554 Granulomatous reactions have appeared suddenly to long-implanted material as a feature of the immune reconstitution syndrome associated with the use of highly active antiretroviral therapy (HAART) for HIV infection. 555 Multiple linear nodules, composed of granulomas of foreign body type, have developed along the superficial veins on both arms in an HIV-positive intravenous drug user treated with HAART. 556
Foreign body granuloma. There is tattoo pigment present. (H & E)
Talc particles are birefringent, as are starch granules; the latter exhibit a characteristic Maltese cross birefringence in polarized light. 557 Incidentally, it is not well known that cryptococci may also be birefringent in polarized light. Materials used to ‘cut’ heroin and other addictive drugs and the filler materials in crushed tablets may produce cutaneous foreign body granulomas in intravenous drug abusers. 558 The elemental nature of unknown inorganic material can be determined using energy-dispersive X-ray analysis techniques if necessary. A granulomatous reaction has been recorded at the base of the penis following the injection of acyclovir (aciclovir) tablets dissolved in hydrogen peroxide, in the self-treatment of recurrent genital herpes infection. 559
Plant material may be readily identified by its characteristic structure and may be PAS positive. 535 It is prudent to perform stains for bacteria and fungi to exclude contaminating organisms when foreign bodies such as wood splinters or bone fragments are found. Pulse granulomas (Fig. 7.21) are rare reactions to particles of food that are characterized by clusters of small to medium-sized hyaline rings.560. and 561. They may be seen around fistulae involving the gastrointestinal tract. Because the hyaline material usually involves vessel walls, cases have also been reported as (giant-cell) hyalin angiopathy (see p. 386).
Pulse granuloma. There is foreign material present and hyaline thickening of adjacent vessel walls, so-called ‘hyalin angiopathy’. (H & E)
A granulomatous reaction at the site of an arthropod bite may be a reaction to insect fragments or introduced epidermal elements. 552 A florid granulomatous reaction producing an exophytic tumor has been reported following multiple bee stings used as a folk remedy. 562
A granulomatous reaction is sometimes seen about certain types of suture material including nylon, silk, and dacron. 563 Each type of suture material has a characteristic appearance and birefringence pattern in tissue sections.
Immunization with aluminum-adsorbed vaccines such as tetanus toxoid may produce an unusual foreign body reaction.564. and 565. A central zone of granular debris containing aluminum and phosphate is surrounded by a rim of granular histiocytes (see p. 392). A marked lymphoid infiltrate with lymphoid follicles and eosinophils is present at the periphery. This may superficially resemble the changes of Kimura’s disease. The granulomatous reaction involving a Mantoux test site may have resulted from the implantation of epidermal keratin during the intradermal injection. 566 The foreign body granuloma that resulted from a BCG vaccination was probably due to the presence of monosodium glutamate in the vaccine. 567 Granulomatous inflammation of the penis has followed intravesical treatments with BCG. The nature of the reactions was never completely elucidated, but it was thought to be a BCG-related granulomatous reaction. 568 A granulomatous reaction of mixed foreign body and sarcoidal types has followed the use of depot formulations of leuprorelin acetate in the treatment of prostate cancer. 569
A granulomatous reaction has been reported on the eyelids following the use of aluminum salts in blepharopigmentation, a process which attempts to produce a permanent line along the eyelid margin, simulating a cosmetic eyeliner.570. and 571. A similar cosmetic tattoo has been reported on the lips. 572 Titanium alloys used in ear piercing are a rare cause of a granulomatous reaction. 573
Granulomas have been described in the skin at the point of entry of acupuncture, indwelling catheter, and venepuncture needles coated with silicone.574.575. and 576. Particles of silicon were detected in macrophages by X-ray microanalysis. Silica granulomas of the elbow have been reported in a tennis player as a consequence of falls on a tennis court which was covered with an artificial silica/polypropylon grass surface. 577 Silicone granulomas have followed its injection into various sites for cosmetic purposes.578.579. and 580. Their origin was not determined in another case. 581 They are discussed further in Chapter 14, pages 394–395.
Both metastatic and dystrophic calcification may be associated with a granulomatous foreign body reaction. This is also seen in idiopathic calcinosis of the scrotum and subepidermal calcified nodules.
A granulomatous reaction to keratin and hair shafts occurs adjacent to ruptured epidermal, pilar and dermoid cysts, pilomatrixomas, and any condition associated with rupture or destruction of a hair follicle. Granulomas have been reported as a reaction to autologous hairs incarcerated during hair transplantation. 584 A similar reaction is seen in the interdigital web spaces of barbers from implanted hair.585. and 586. It is not uncommon for enlargement of a banal nevocellular nevus to be due to a granulomatous reaction following damage to a hair follicle. Fragments of keratin may or may not be found in these reactions. Occasional fine wavy eosinophilic squames may be identifiable within spaces in the dermis or within giant cells. Hair shafts are oval or rounded structures when cut in section and sometimes exhibit cortical and medullary layers: they are variably birefringent in polarized light and acid fast when stained by the Ziehl–Neelsen technique. Foreign body granulomas to keratin are also seen near squamous cell carcinomas and in recurrences. Their presence is an indication for a careful search for residual tumor. 587
Cutaneous amyloid is usually inert but in nodular amyloidosis it may occasionally provoke a foreign body giant cell reaction.
Xanthogranulomas are granulomas composed of numerous histiocytes with foamy/pale cytoplasm and a variable admixture of other inflammatory cells and some Touton giant cells. The diseases in this category are considered in Chapter 40, pages 953–959.
The prototype disease for this category is juvenile xanthogranuloma, but the other non-Langerhans cell histiocytoses are also included. 1 In addition, the xanthomas can be considered in this category although there are usually only sparse or no inflammatory cells in some of these diseases. Reticulohistiocytoma is another example. 1
The miscellaneous category includes conditions which do not fit neatly into any of the more established categories of granulomatous disease.
The following conditions will be discussed in this section:
• Chalazion
• Melkersson–Rosenthal syndrome
• elastolytic granulomas
• annular granulomatous lesions in ochronosis
• granulomas in immunodeficiency disorders
• interstitial granulomatous dermatitis
• interstitial granulomatous drug reaction
• superantigen id reaction
• granulomatous T-cell lymphomas.
A chalazion is a solitary, usually painless lesion of the eyelid that results from a granulomatous reaction to lipid released from a blocked sebaceous gland. It is best visualized when the lid is everted. Recurrent lesions may occur in patients with seborrheic dermatitis and rosacea.
The granulomatous reaction in a chalazion has mixed tuberculoid and foreign body features. Sometimes there is associated suppuration as well, with small collections of neutrophils. In the center of the granuloma there is a characteristic clear space resulting from lipids that have been removed during processing. There is a heavy chronic inflammatory cell infiltrate surrounding the granuloma(s). The infiltrate is composed of lymphocytes, some plasma cells, and a few neutrophils.
The Melkersson–Rosenthal syndrome is a rare condition of unknown etiology characterized by the triad of chronic orofacial swelling predominantly involving the lips, recurrent facial nerve palsy, and a fissured tongue (lingua plicata).588.589.590.591.592. and 593. The complete triad occurs in about 25% of cases. A monosymptomatic form in which there is localized episodic swelling of the lip(s) has been called cheilitis granulomatosa of Miescher or granulomatous cheilitis.594.595.596. and 597. The term ‘orofacial granulomatosis’ was introduced by Wiesenfeld and colleagues in 1985 to cover both granulomatous cheilitis and Melkersson–Rosenthal syndrome. 588 Anogenital granulomatosis has been regarded as the counterpart of orofacial granulomatosis.598. and 599. Crohn’s disease and sarcoidosis need exclusion. Some of these cases were called vulvitis granulomatosa in the past.598. and 600. The concomitance of granulomatous cheilitis and vulvitis is extremely rare. 601
The presenting complaint is usually swelling of the lips, but adjacent areas of the cheek are frequently involved. 593 The initial facial swelling may last only a few days and be soft and fluctuant, but it becomes firmer and persistent with time. 602 Facial nerve palsy, usually unilateral, occurs in 13–50% of cases.588. and 603. Facial swelling has also been reported in association with syringomyelia. 604 The median age at onset was 20 years in one series, and there was an equal sex incidence. 588 Persistent unilateral orbital and eyelid edema is an extremely rare manifestation of the disease. 605
The etiology is unknown but the syndrome has been considered to be a manifestation of sarcoidosis, 606 a reaction to infection or to foreign material, such as silicates, gold, and mercury, 607 and a delayed hypersensitivity to cow’s milk protein or food additives. 608 In one case, it was worsened by the cocoa in drinking chocolate. 609Borrelia burgdorferi has been excluded as an etiological agent, 610 but the DNA of Mycobacterium tuberculosis has been identified by PCR in one case. 611 In a further case the granulomatous cheilitis was regarded as the consequence of a tuberculid. 612 Elimination of odontogenic infections has produced remission in some cases. 613
Occasional cases have been associated with other granulomatous skin lesions or granulomatous lymphadenopathy.588. and 614. A granulomatous cheilitis may be a manifestation of Crohn’s disease.279.615.616. and 617. The lip sign may predate gastrointestinal symptoms by years.618. and 619. There is one report of a patient with Crohn’s disease and the full triad of lesions associated with the Melkersson–Rosenthal syndrome. 620
Granulomatous cheilitis has been successfully treated with clofazimine, thalidomide, and infliximab.616.621. and 622. Triamcinolone injections have also been used, both alone,623. and 624. and combined with dapsone.625. and 626. Sometimes surgical treatment is necessary for the persistent macrocheilia that may occur with Melkersson–Rosenthal syndrome and cheilitis granulomatosa.627. and 628. Amalgam removal resulted in the resolution of another case. 629
There is marked edema in the dermis together with a perivascular inflammatory cell infiltrate consisting of lymphocytes, plasma cells, histiocytes, and occasional eosinophils; the infiltrate may extend into underlying muscle. Small ‘naked’ collections of epithelioid cells, loose tuberculoid granulomas with a peripheral round cell infiltrate or isolated multinucleate giant cells are usually present. The inflammatory infiltrate is more consistently related to vessels than that in sarcoidosis (Fig. 7.22). Schaumann bodies and birefringent fragments may occasionally be seen in histiocytes and giant cells. Lymphatics are usually widely dilated and may contain collections of inflammatory cells. Alternatively, inflammatory cell collections may bulge into the lumen of vessels. 630 Older lesions may show dermal fibrosis. Collagenous nodules which represent fibrosed granulomas may be found after treatment with steroids. 631 Overlying epithelial changes are non-specific. There are no reliable features to allow distinction of those cases which represent a manifestation of Crohn’s disease.
(A) Melkersson-Rosenthal syndrome. (B) A granulomatous reaction is present adjacent to a vessel containing inflammatory cells. (H & E)
Similar histological changes are seen in association with chronic edema and swelling of the vulva and penis in some cases of recurrent infections of this region.599. and 632. Squamous cell carcinoma of the vulva has been reported in long-standing vulvitis granulomatosa. 633
The violaceous lesions reported in patients with rheumatoid arthritis as cutaneous histiocytic lymphangitis and angioendotheliomatosis have some histological similarities to both Melkersson–Rosenthal syndrome and angioendotheliomatosis.634. and 635. Both reports would appear to be describing the same entity. There were dilated lymphatics in the dermis containing aggregates of inflammatory cells, mainly histiocytes, with adjacent lymphoid aggregates, but no granulomas as seen in Melkersson–Rosenthal syndrome. Granulomas were present in another case with intralymphatic histiocytosis associated with orthopedic metal implants. 636 The term intravascular histiocytosis is now the preferred title for this entity (see p. 961).
The elastolytic granulomas predominantly affect the exposed skin of the head, neck, and limbs. This group of granulomatous conditions includes actinic granuloma, 637 annular elastolytic giant cell granuloma, atypical necrobiosis lipoidica of the face and scalp, 638 and Miescher’s granuloma. 639 They are all characterized by annular lesions exhibiting a zonal histological pattern that includes a granulomatous response with giant cells at the annular rim and centrally a loss of elastic fibers or the presence of solar elastotic material. These conditions appear to form part of a spectrum. Some have used the term annular elastolytic giant cell granuloma as the group generic term,640. and 641. while others have used it for cases not associated with actinic damage, and have retained the term actinic granuloma for those that do. The two entities will be considered separately in the discussion that follows. The relationship, if any, of this group to the necrobiotic granulomas is controversial. Another lesion, granuloma multiforme, is also very similar clinically and histologically to these conditions and is discussed here.
In 1975, O’Brien described annular skin lesions which occurred in sun-damaged skin and were characterized histologically by disappearance of solar elastotic fibers and, at the edge of the lesion, by a histiocytic and giant cell inflammatory reaction.637. and 642. His concept of a granulomatous response to solar elastosis was challenged by some643 and supported by others.644. and 645. Some felt that this lesion was granuloma annulare in sun-damaged skin.643. and 646. In support of O’Brien, similar changes have been described in association with solar elastosis in pinguecula of the bulbar conjunctiva.647. and 648. Temporal arteritis may arise in association with actinic granuloma. Both conditions have been regarded as a response to actinically damaged elastic tissue. 649
As initially described, actinic granuloma begins as single or grouped pink papules which evolve to annular lesions in sun-exposed regions of the neck, face, chest, and arms. A reticular pattern has been described in one case. 650 Both sexes are affected equally and most of the patients are 40 years of age or older. Alopecia resulted in one case. 651 Solitary cases have been reported in association with relapsing polychondritis, 652 molluscum contagiosum, 653 and cutaneous amyloidosis. 654
Actinic granuloma has been reported following prolonged sunbed usage, 655 and in association with prolonged doxycycline phototoxicity. 656 Acitretin has been used to treat this condition. 657
In annular lesions, the changes seen at the rim of the lesion differ from those in the center (Fig. 7.23). The dermis in the region of the rim is infiltrated by histiocytes and there are many foreign body giant cells. The latter are applied to, and engulf, elastotic fibers (elastoclasis; Fig. 7.24). There is also a variable component of lymphocytes, plasma cells, and eosinophils. Within the central zone, there is complete or almost complete loss of both elastotic fibers and normal elastic fibers. The dermal collagen in this region is relatively normal or slightly increased. Unlike granuloma annulare and necrobiosis lipoidica, necrobiosis is not usually seen. The absence of increased dermal mucin also distinguishes most cases from granuloma annulare. Asteroid bodies are sometimes present in giant cells. In some cases mononuclear histiocytes may be more prominent than multinucleate giant cells, and occasionally tuberculoid granulomas form. 658
Actinic granuloma. There are many foreign body giant cells arranged around elastotic fibers. Some fibers have been phagocytosed. (H & E)
Actinic granuloma. Multinucleate giant cells are engulfing elastotic fibers. (H & E)
A similar granulomatous response can occur in relation to some basal cell carcinomas and keratoacanthomas. 645 Elastoclasis has also been described in granuloma annulare, 659 elastosis perforans serpiginosa, and other lesions occurring in sun-damaged skin. 643 In these cases, elastoclasis may represent a secondary response to elastotic fibers which have been altered in some as yet unknown way by the primary process, whereas in actinic granuloma there is no obvious provoking cause. It has been suggested that there is a cell-mediated immune response to antigenic determinants on actinically altered elastotic fibers. 660 Elastophagocytosis may also be seen in sun-protected skin in association with a variety of inflammatory conditions. 661
In one study comparing actinic granuloma and granuloma annulare, absence of elastotic material in the center of the lesions and the presence of scarring and giant cells with up to 12 nuclei were characteristic of actinic granuloma. By comparison, granuloma annulare was characterized by moderate amounts of elastotic material within granulomas, scarring was absent and giant cells contained fewer nuclei. 662 Similar findings have been made in two subsequent comparative studies,663. and 664. although in one of these studies, two cases with some features of granuloma annulare were described. 664
As already mentioned, this term has been used by some authors to describe all cases characterized by annular plaques with histological evidence of elastophagocytosis by multinucleated giant cells.640.641.666.667.668.669. and 670. It is used here in a more restricted sense to exclude cases with severe solar elastosis, discussed here as actinic granuloma (see above). They are both variants of elastolytic granulomas, the preferred group generic term.
It presents with multiple papules and annular plaques, sometimes spread over large parts of the body.671. and 672. Lesions are usually more extensive than in actinic granuloma. The plaques grow slowly. Covered areas are often involved. Infants are rarely affected; lesions resolved after the use of oral tranilast and topical pimecrolimus in one such infant. 673
Annular elastolytic giant cell granuloma has been regarded as a prodromal stage of mid-dermal elastolysis. 674
There are granulomatous infiltrates, composed mostly of multinucleated giant cells exhibiting elastophagocytosis. There is no mucin, necrobiosis, or palisading. Rare lymphocytes are sometimes present. There is variable loss of elastic fibers; it is complete in late stages of the disease.
A condition characterized by annular lesions of the upper face and scalp has been called ‘atypical necrobiosis lipoidica’. 638 It occurs predominantly in females. The average age of onset is around 35 years. The lesions resolve spontaneously or persist for many years. Unlike necrobiosis lipoidica, they heal without scarring or alopecia. Some patients have necrobiosis lipoidica at other sites.
Lesions with similar clinical and histological features to those seen in atypical necrobiosis lipoidica have been described as Miescher’s granuloma of the face. 639 It has been suggested that both conditions represent actinic granulomas although solar elastosis has not been a conspicuous feature in either. 637 The issue is further confused by reports of actinic granuloma with areas of necrobiosis.658. and 675.
These lesions are characterized by a central healing zone, in which there is loss of elastic tissue, and a peripheral raised edge. In the latter region there is a lymphocytic and histiocytic dermal infiltrate which is distributed between collagen bundles. The infiltrate includes multinucleate giant cells, some of which contain asteroid bodies. Necrobiotic areas and increased dermal mucin have not been described.
The granulomatous dermatitis, granuloma multiforme, was originally recognized because of its potential importance in the differential diagnosis of tuberculoid leprosy, which it resembles clinically and, to some extent, histologically.676. and 677. First reported in Nigeria, granuloma multiforme has also been reported in other central African countries, in Indonesia and in India.676. and 678. Papular and annular lesions occur on exposed regions of the trunk and arms. 679 Both sexes are affected and most of the patients are aged 40 years or more. There was a marked female predominance in one series. 680 It has been suggested that this is a variant of granuloma annulare or necrobiosis lipoidica. 680 Others consider it to be related to actinic granuloma. 637
The zonal histology described in actinic granuloma is also seen in this condition (see above). There is destruction of dermal elastic tissue, with mild fibrosis in the center of annular lesions. In the raised active edge of the lesion there is a granulomatous reaction which includes histiocytes, multinucleate giant cells, lymphocytes, eosinophils, and plasma cells. Elastoclasia (elastic fiber phagocytosis by histiocytes) is seen in this region. Areas of necrobiosis have been described, surrounded by a palisaded rim of histiocytes, in the middle and upper dermis in the annular rim. 680 Solar elastosis may occur in black-skinned people but it is not clear whether it is present in the lesions of granuloma multiforme in black patients. 681
In one series of cases there was no evidence of fat within these lesions on special staining; mucin stains were inconclusive. 680
There have been several reports from South Africa of an annular eruption in ochronotic areas of the face in a group with hydroquinone-induced ochronosis.682.683. and 684. The lesions clinically resemble actinic granuloma and have a zonal appearance with a peripheral hyperpigmented ochronotic zone, an elevated rim and a central hypopigmented area.
Sections of the rim show a granulomatous response with histiocytes, epithelioid histiocytes, giant cells, lymphocytes, and plasma cells. Phagocytosis of ochronotic fibers is seen, these fibers representing pigmented swollen collagen fibers. There may be epidermal changes associated with transepidermal elimination of ochronotic material in this region. The central zone has an atrophic epidermis with underlying absence of elastotic material and ochronotic fibers together with mild fibrosis. Elastophagocytosis was not seen despite the absence of elastotic material. Sarcoidal granulomas have also been reported in these lesions. 682 It has been suggested that these lesions may represent a manifestation of sarcoidosis since some but not all cases are associated with systemic sarcoidosis. 684
Granulomas of various types have been described in cutaneous lesions in persons with genetic and acquired immune deficiency disorders. 685 They are listed in Table 7.3. In those with non-AIDS-related immune deficiency, various granuloma types have been described in cutaneous lesions. 686 Although, as might be expected, some are associated with a variety of infectious agents to which these patients are prone, many are not. Excellent reviews of the primary immunodeficiency disorders have been published.687. and 688.
Chronic granulomatous disease
X-linked hypogammaglobulinemia
Common variable immunodeficiency
Ataxia-telangiectasia
Nijmegen breakage syndrome
Severe combined immunodeficiency
Primary acquired hypogammaglobulinemia
In chronic granulomatous disease, despite the name, true granulomas are not common in cutaneous lesions. There are a variety of reports of suppurative granulomas with organisms, foreign body granulomas with and without organisms, and caseation necrosis.686.689.690.691.692.693.694. and 695. Carriers of X-linked chronic granulomatous disease (OMIM 306400) may present with lupus erythematosus-like lesions. 696 Several types of autosomal recessive chronic granulomatous disease occur (OMIM 233700, 233710, 233690). Caseating granulomas have been described in X-linked infantile hypogammaglobulinemia (OMIM 300300). Lymphocytes in the granulomas were almost exclusively of CD8 phenotype. 697 Sarcoid-like and caseating granulomas have been reported in lesions of common variable immunodeficiency (OMIM 240500).698.699.700.701.702.703.704. and 705. This disease, which has multiple phenotypes, is the most commonly diagnosed primary immunodeficiency disease in adults, after selective IgA deficiency. 706 Onset of symptoms is not until the second or third decade of life.706. and 707. It results from a dysfunction of B-cell differentiation resulting from mutations in the TNFRSF13B gene on chromosome 17p11.2. 708 Tumor necrosis factor-α (TNF-α) is elevated in this condition, and specific inhibition of this cytokine has been successful in moderating the disease. 709 Cutaneous lesions in ataxia-telangiectasia (OMIM 208900) have contained necrobiotic and tuberculoid granulomas.521.710.711. and 712. Sarcoid-like granulomas have also been reported in this condition and in the related Nijmegen breakage syndrome (OMIM 251260). 713 Necrobiotic and tuberculoid granulomas have also been reported in combined immunodeficiency, an old term for a heterogeneous group of conditions. 714 Sarcoidosis with typical granulomas may also be associated with combined immunodeficiency. 715 There is a lower CD4+/CD8+ ratio in the sarcoidal granulomas of the immunodeficiency group than in the granulomas of sarcoidosis. 716 In one case of primary acquired agammaglobulinemia, non-caseating granulomas were described. 717 Two neonates with perforating neutrophilic and granulomatous dermatitis have been reported. This pattern was said to be a clue to an immunodeficiency which took the form of agammaglobulinemia. 718






