Fig. 72.1
Incidence of firearm-related injuries stratified by age groups (Zit.)
72.2 Age-Related Physiology and Effect on Trauma: What You Should Know
Functional changes with age, preexisting diseases, and pre-injury medications result in limited physiological reserves and a decreased ability of the elderly patient to mount an adequate response to stress. A summary of anatomic and physiologic changes with aging is provided in Table 72.1 and Fig. 72.2.
Table 72.1
Age-related anatomic and physiologic changes
Central nervous system |
Brain atrophy |
↑ subdural space |
↑ tension on bridging veins in subdural space |
Adherent epidural space |
Cardiac system |
↓ cardiac function/output |
↓ maximal tachycardic response |
↓ response to intrinsic and extrinsic catecholamines |
Vascular system Thickening and calcification of vessels |
↓ elasticity of vessels |
Respiratory system |
↓ pulmonary compliance |
↓ vital capacity |
↑ residual capacity |
↓ surface area for gas exchange |
↓ cough reflex |
↓ mucociliary clearance |
↑ chest wall rigidity |
Renal system |
↓ renal mass |
↓ GFR |
↓ response to ADH/aldosterone |
↓ urine concentration ability |
↑ renal sensitivity to contrast |
↑ urethral outflow obstruction |
Skeletal system and soft tissue |
Osteoporosis |
Skin atrophy |
↓ subcutaneous fat |
↓ cutaneous microcirculation |
↓ muscle mass |
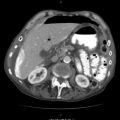
Fig. 72.2
Clinical consequences of age-related changes
72.2.1 Cardiovascular System
Cardiac function declines by 50 % between the ages of 20 and 80 years, mainly due to increasing myocardial stiffness, slowing of electrophysiologic conduction, and loss of myocardial cell mass. The cardiac index falls off linearly with age and the maximal heart rate begins to decrease from about 40 years of age. The response of the aging myocardium to circulating catecholamines decreases, limiting its ability to maintain cardiac output in the presence of hypovolemia.
Baseline hypertension is common in the elderly patient; thus, a normal blood pressure may actually indicate significant hypovolemia.
Medications such as β-blockers and calcium channel blockers limit the normal tachycardic response to shock. Chronic use of diuretics results in intravascular depletion and limited intravascular reserve.
72.2.2 Renal System
There is a progressive loss of renal mass, with a corresponding decrease in creatinine clearance and urine concentrating ability. Although the serum creatinine level may remain normal because of age-related declines in muscle mass, there is a decreased tolerance to hypotension and nephrotoxic drugs.
72.2.3 Respiratory System
The pulmonary system demonstrates decreased compliance and vital capacity. There is increased dependence on diaphragmatic breathing, increased work of breathing, impaired mucociliary clearance, and a reduced ability to cough, all of which decrease the ability to tolerate even minor chest trauma and increase the propensity for developing complications.
72.2.4 Central Nervous System
The human brain loses approximately 10 % of its weight between the ages of 30 and 70 years.
A decrease in autoregulation of cerebral blood flow increases the vulnerability to cerebral ischemia associated with systemic hypotension and decreases the tolerance to injury.
Dementia and other underlying chronic CNS diseases (e.g., degenerative brain disease, hydrocephalus, cerebrovascular disease, etc.) may make the clinical evaluation difficult.
72.3 The Geriatric Patient in the Field: Prehospital Evaluation
The injured geriatric patient should not be exposed to prolonged field stabilization attempts at the expense of transport time. The triage process begins in the field, where prehospital providers must decide on the basis of very little clinical information whether a patient should bypass nearby facilities in favor of a designated trauma center. The American College of Surgeons Committee on Trauma recommends patients greater than 55 be considered for transport directly to a verified trauma center, irrespective of the severity of injury. This recommendation is based on the finding that there is a sharp increase in mortality that occurs at this age independent of injury severity, mechanism, and body region involved. Unfortunately, several studies have documented that the opposite may actually be occurring with elderly trauma patients being frequently undertriaged to non-trauma hospitals putting them at risk for admission to a level of care that may be unsuitable. In one study, trauma patients over the age 65 were half as likely as younger patients with similar injuries to be transported to a designated trauma center. In another recent study, undertriage in patients older than 70 years was five times higher than in those younger than 70 years old.
72.4 The Geriatric Patient in the Emergency Room: Initial Evaluation and Management
72.4.1 Trauma Team Activation: Be Ready!
On admission, geriatric trauma patients warrant rapid and aggressive evaluation by a trauma team. In a recent clinical series, traditional hemodynamic criteria for mobilizing the trauma team demonstrated 63 % of patients aged 70 or above and with an ISS >15 were missed by traditional physiologic criteria. In a follow-up before and after study, for patients older than 70 with an ISS >15, the authors examined the impact of including age alone (>70 years old) as a criteria for activation of the trauma team. This age trigger, resulting in the presence of an attending trauma surgeon and ER physician at patient arrival, continuous cardiopulmonary monitoring, and attending or senior resident presence at the bedside at all times, resulted in a significant decrease in mortality from 53.8 to 34.2 %, p = 0.003. So for elderly patients, have the trauma team ready when an elderly patient arrives.
72.4.2 Primary Survey: The “Geriatric ABCs”
In general, the primary survey in the geriatric patient does not differ from that in the younger patient and adheres to the ATLS protocol. However, preexisting comorbidities and medications may impact patient evaluation (Table 72.2).
Table 72.2
Preexisting conditions and possible systemic medications and their clinical consequences
Preexisting conditions and comments | Systemic medications and comments |
|---|---|
Dementia Difficult neurologic assessment | Cholinergics, antidepressants ↓ seizure threshold ECG changes |
Prior stroke Neurologic deficits | Aspirin, clopidogrel, warfarin ↑ bleeding |
Arterial hypertension Normal BP may signify hypotension Heart failure Exclude myocardial infarction Expect arrhythmias | β-blocker, calcium channel blocker, ACE inhibitor, diuretics, antiarrhythmics ↓ tachycardic response ↓ peripheral vasoconstriction → ↑ bleeding |
Peripheral vascular disease Difficult vascular assessment and repair | Aspirin, clopidogrel, warfarin ↑ bleeding |
Chronic obstructive pulmonary disease (COPD) Hypoxia, hypercarbia Early intubation and ventilation | Steroids ↓ PLT function → ↑ bleeding ↓ wound healing ↑ infection |
Chronic renal failure Fluid overload Hypertension Electrolyte disturbance Contrast-induced nephropathy | Diuretics, antihypertensives Exclude electrolyte disturbances ↓ intravascular volume → ↓ tolerance of hypovolemia |
Diabetes mellitus Exclude hypoglycemia Difficult neurovascular assessment | Hypoglycemics Check serum glucose |
Osteoporosis ↑ fractures Careful intubation (C-spine precautions!) | – |
Rheumatoid arthritis ↑ difficulty in opening mouth → difficult intubation | NSAID, steroids, immunosuppressives ↓ PLT function → ↑ bleeding ↓ wound healing ↑ infection Monitor renal function closely |
Airway Management
The elderly have a significant loss of protective airway reflexes, and therefore, aspiration is more common. Mouth opening may be limited, and immobility of the cervical spine, due to stiffening of the atlanto-occipital joint, may make visualization of the glottis during orotracheal intubation difficult. Deterioration of the gums may increase the chance of damage to the teeth. Additionally, many elderly individuals wear dentures. If these become dislodged, airway obstruction may result. Removal of dentures often results in difficulty with mask fit during assisted ventilation. Accordingly, well-fitting dentures should be left in place to assist mask ventilation but should be removed for intubation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree