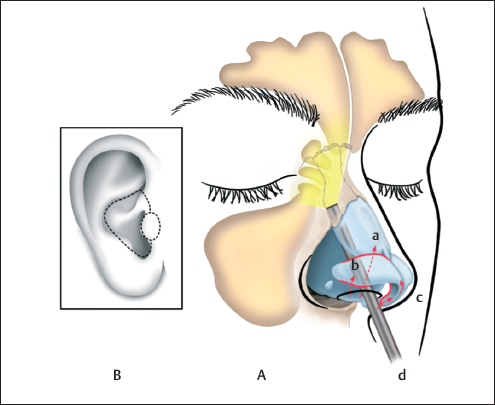
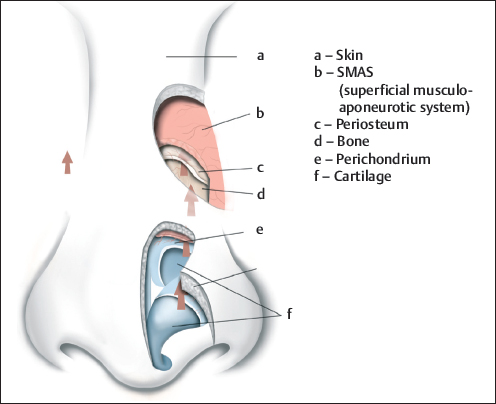
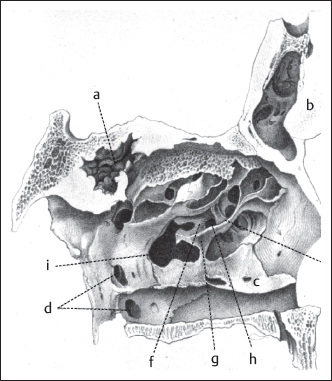
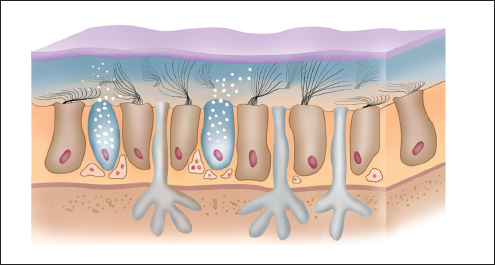
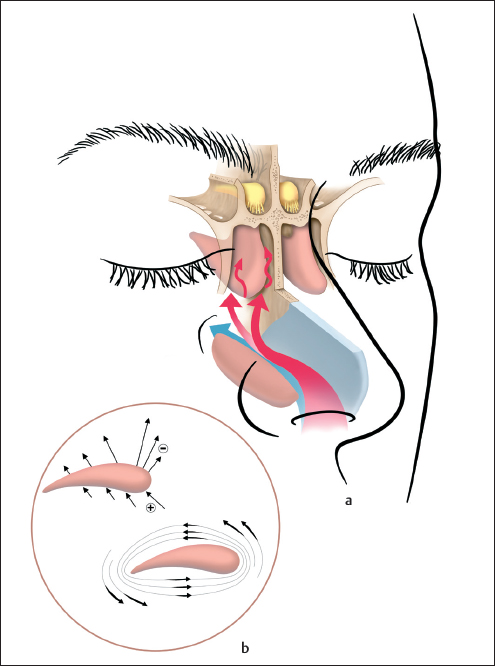
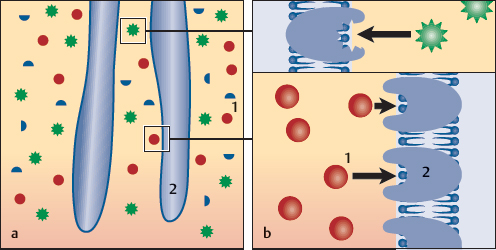
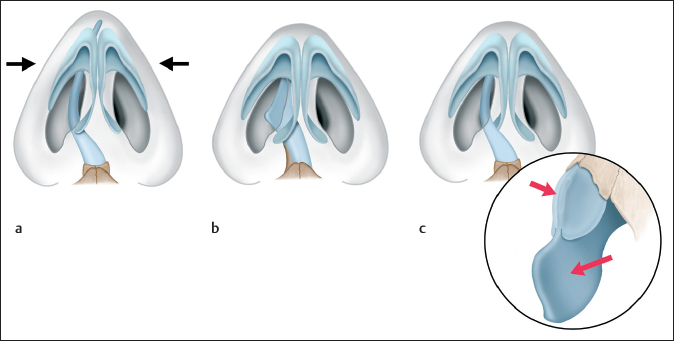
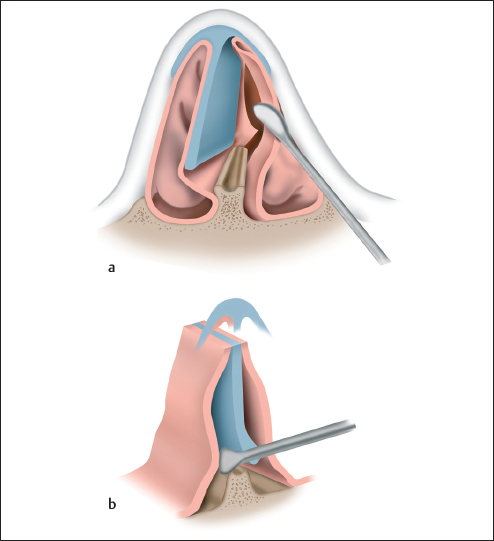
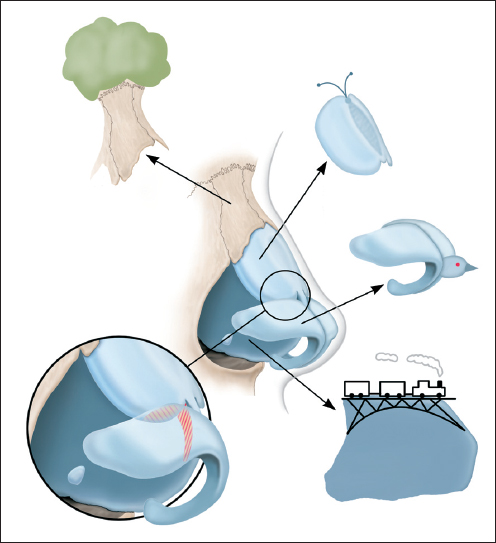
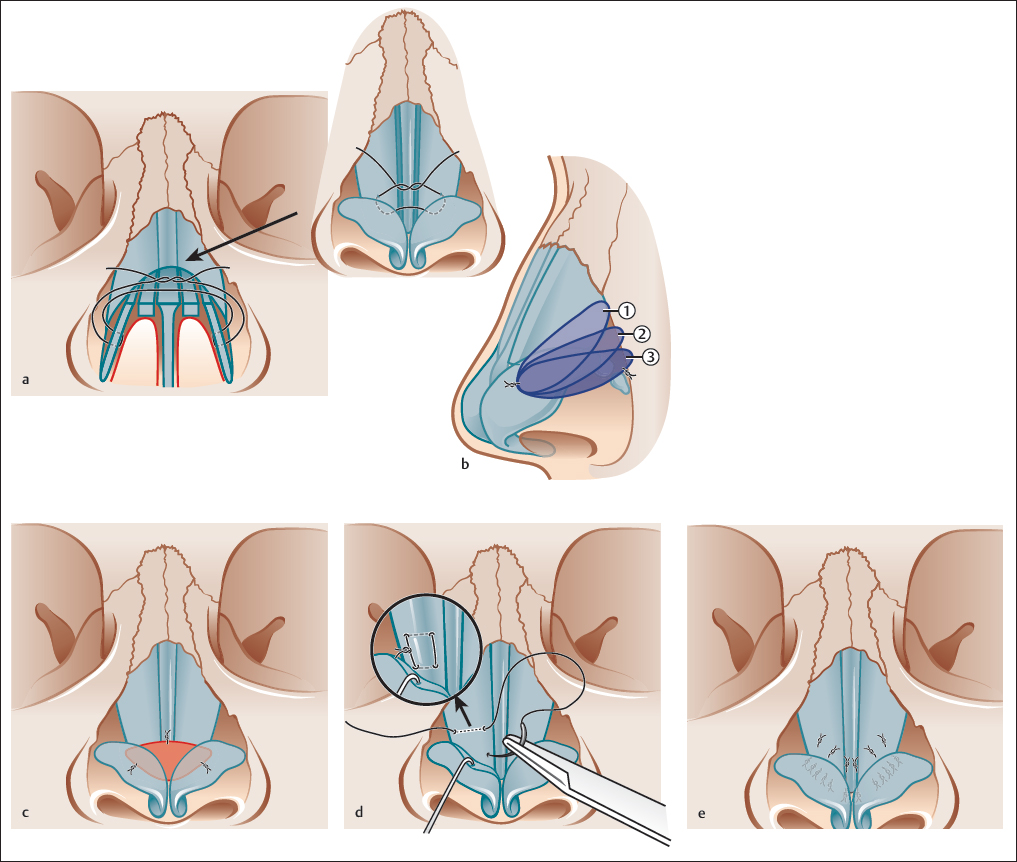
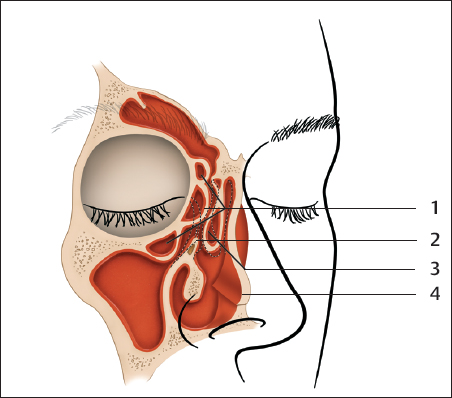
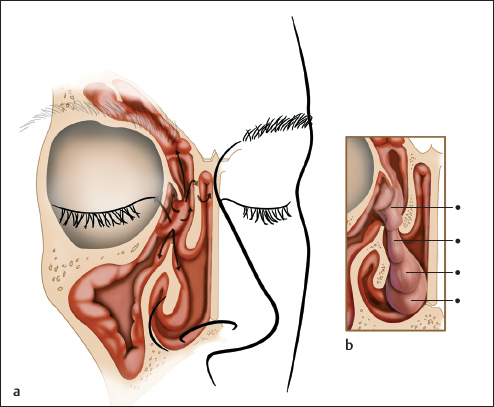
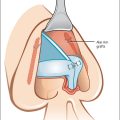
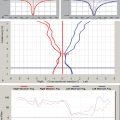
Chapter 1 1.4 The Nose as a Respiratory Organ 1.5 The Nose as a Sensory Organ 1.6 Prerequisites for the Concept of Functional-Aesthetic Nasal Surgery 1.7 Functional Aspects of Septorhinoplasty 1.8 Aesthetic Aspects of Septorhinoplasty 1.9 Selecting an Approach for Septorhinoplasty Young sailors in the International Optimist class trim their sails with the help of a tensioning pole called a sprit. The stronger the wind, the more tightly the sprit is set. The lower the tension on the sprit, the more the sail will billow open. This change in the shape of the sail is clearly reflected in the adjacent top triangles. A similar mechanism is at work in the nose. The height and tension of the anterior septum significantly affect the aperture angle of the nasal valve and the tension and shape of the tip and supratip area. The goal of any structure-conserving surgery of the nose, as in the spritsail, is to change the shape of the internal and external nose by altering the tension and traction on specific structural elements (Fig. 1.1). The nose performs a variety of functions. It is a respiratory and sensory organ and has a special aesthetic importance as a central feature of the face. It is a reflex organ and adds resonance to phonation. The functional and aesthetic aspects of the nose are inseparably linked in a morphological sense.1 It is our experience that functional and aesthetic problems of the nose almost always coincide. Rhinosurgery aimed exclusively at improving function will very quickly reach its limits if it disregards external form. This is clearly illustrated by the “tension nose,” deviated nose, and saddle nose. Conversely, rhinosurgery that is done purely for aesthetic goals forfeits valuable opportunities, as in the cases where the impact of septal surgery on nasal tip aesthetics is not used to modify tip definition, projection, and rotation.2,3 Goldman found that in more than 70% of his cases, the presence of septal deviation coexisted with a deformity of the external nose.4 Meyer performed a concomitant septoplasty in 80% of his primary and secondary rhinoplasties.5 Masing explained the importance of external nasal shape in respiratory function by noting the smaller cross-sectional areas of the external nose compared with the internal nose.6 Fig. 1.1 As in a sail, the shape and function of the nose can be influenced by altering (cartilage) tensions. Farrior states that surgical correction of the external nose is often the prerequisite for normal, unobstructed nasal breathing.7 Our own experience confirms the results of Schulz-Coulon,8 who addressed the question of whether rhinoplasty is a predominantly aesthetic or functional procedure.9 When statistical analysis was applied based on patients’ motivations for surgery and their satisfaction or dissatisfaction with the outcome, this question could not be answered in terms of a predominantly aesthetic or functional operation. This led the author to agree with Haas that both terms should be discarded in favor of the more accurate term, corrective rhinoplasty.8,10 But the concept of functionality does not apply just to the improvement of nasal breathing. It includes the following aspects as well: • Peripheral olfactory disturbances. • Recurrent and chronic sinusitis. • Middle ear ventilation problems. • Rhinogenic headache. • Poor vocal quality. • Nasal ventilation problems due to rhonchopathy. Functional–aesthetic rhinoplasties are among the most demanding procedures in facial plastic surgery. In themselves, they pose a significant challenge to the rhinosurgeon. It is logistically and technically feasible to include the above indications without getting lost in too many details while still addressing the patient’s desire to solve multiple problems in a single operation.11 Surgeons should have all the techniques and approaches of rhinoplasty and endoscopic endonasal microsurgery in their repertoire. We caution against the current trend toward the exclusive use of the open approach, because the advantage of clear operative exposure is offset by a substantial increase in tissue trauma and subcutaneous scarring. Circumstances will dictate the best choice from among the available options: the cartilage-splitting approach, delivery approach, or open approach (Fig. 1.2). To avoid drawback of a limited overview of the depth of the surgical field in the closed techniques, the desire arose to adopt endoscopic surgical procedures in septoplasty and rhinoplasty for both functional and aesthetic indications. The approach should be as effective as possible and as invasive as necessary. Minimizing surgical trauma is of key importance, as it is the best means that the surgeon has for influencing postoperative wound healing and scar formation. While surgeons can directly alter the size and position of cartilage and bone, they can influence wound healing, and ultimately the definitive outcome, only by working atraumatically in the appropriate favorable surgical planes, creating small and appropriate graft beds, and reducing bleeding by preserving the muscular and vascularized planes of the nose (Fig. 1.3). Besides selecting the approach, surgeons can choose from among several techniques (incision, suturing, or grafting) to achieve the desired goal in various ways. Nevertheless, most techniques are rarely of equal suitability. The technique of choice will depend upon skin type, connective-tissue type, and factors such as the age of the patient and the resiliency of the cartilage. Fig. 1.2 (A) All approaches to the nasal tip and nasal dorsum can be combined with the endoscopic endonasal approach to the internal nose and paranasal sinuses. (a) Intercartilaginous or transcartilaginous route. (b) Alar cartilage rim incision combined with intercartilaginous incision in the delivery approach. (c) Columellar incision, columellar rim incision, and alar cartilage rim incision in the open approach. (d) Endoscopic approach to the posterior septum and ethmoid—the gateway to the paranasal sinuses. (B) “The external ear exists as a marvelous storehouse of skeletal spare parts for the nose.” M.E. Tardy Jr.107 Partial or complete loss of the nose causes severe disfigurement of the face. This kind of trauma injures not just the human body, but also the mind. The destruction of the aesthetic and psychological integrity of a personality is among the cruelest testimonials of bygone eras. Many ancient sculptures bear witness to this act in symbolic form.12,13 Cutting off the ears and nose as a form of punishment motivated the earliest attempts at reconstructive plastic surgery in India approximately 1,500 years ago.13–15 The Indian rhinoplasty was performed with a midline forehead flap in a concept that resembles methods still in use today. This technique was described by Sushruta in approximately 600 BC. Galenus mentioned that the Egyptians performed nasal operations, but they kept their methods a secret.14 Much later, around 1430, the Branca family (first the father, later the son) developed a procedure for reconstructing the nose with a flap from the upper arm. Gaspare Tagliacozzi (1545–1599), writing in the first textbook on plastic surgery, described techniques for nasal reconstruction that he adopted from Branca and refined. Although that occurred about a century after the Brancas used the upper arm flap, Tagliacozzi is still considered the founder of Italian rhinoplasty.12,14–16 The human desire for the aesthetic rehabilitation of traumatic or congenital disfigurement, with an opportunity for social reintegration, was definitely the original motivation for reconstructive rhinoplasty. The age of corrective aesthetic rhinoplasty was inaugurated by John Orlando Roe (1848–1915), an otorhinolaryngologist from Rochester, New York. This surgeon corrected saddle nose deformities through an endonasal approach.17 In 1891, Roe also used intranasal approaches for dorsal hump removal.6,14 Innovations in the functional aspects of rhinoplasty were later introduced by Mink, van Dishoek, Cottle, and others.18–20 Surgeons and rhinologists who practiced in Berlin from the 18th to the 20th centuries greatly influenced the subsequent development of functional–aesthetic rhinosurgery. Carl Ferdinand von Graefe (1787–1840) was appointed from Wilhelm von Humboldt (1767–1835) as a first professor in ordinary of the Institute of Clinical and Ophthalmological Surgery at the newly founded Friedrich-Wilhelm University in Berlin in 1810 when he was just 23 years old. He was a skilled surgeon who had a keen interest in plastic surgery of the face and jaws. He performed the first successful repair of a cleft palate in 1816. For autologous nasal reconstruction, he used both the Indian and Italian techniques and added his own refinements. He corrected deformities of the face, especially those involving the lips, eyelids, cheek, and nose21,22 (Fig. 1.4). His son, Albrecht von Graefe (1828–1870) became the founder of ophthalmology as a medical specialty (Fig. 1.5). He developed several principle surgical techniques for the therapy of cataract, strabismus, and glaucoma. He is the inventor of the ophthalmoscope. Johann Friedrich Dieffenbach (1792–1847) succeeded von Graefe, who kindled his enthusiasm for facial plastic surgery. Dieffenbach dedicated himself to refining the plastic surgical procedures of his day. He did pioneering work in such areas as cleft lip and palate repair, blepharoplasty, the surgical correction of strabismus, and tenotomy for the treatment of clubfoot. He promoted modern rhinoplasty by developing a dual-flap technique that repaired both cutaneous and mucosal defects, thereby reducing the problem of flap shrinkage. He became internationally known through his first strabismus operation and numerous monographs. Along with Guillaume Dupuytren of France, Ashley Cooper of England, and Nikolai Pirogow of Russia, Dieffenbach was among the greatest surgeons of his time and is considered the founder of plastic surgery22–24 (Fig. 1.6). The following episode helped to establish Dieffenbach’s special reputation in 19th-century Berlin: A charming young woman who attended society balls in 1831 and 1832 attracted considerable attention by always hiding her face behind a golden mask. Elvira Tondeau’s secret was that her face had been disfigured by deep ulcerative lesions of the nose, presumably a result of tuberculosis cutis luposa. Dieffenbach was able to reconstruct her nose in several sittings. One year later, Elvira entered into a much-publicized engagement. Dieffenbach’s accomplishment was immortalized in a contemporary folk song that claimed that “… he makes the nose and ears like new.”22 General anesthesia was developed in 1846, making painless surgery a reality. In 1878, Robert Koch published his paper “Studies on the etiology of wound infections.” Joseph Lister (1827–1912) paved the way for germ-free operations. Berhard von Langenbeck (1810–1887) was Dieffenbach’s successor at the Berlin Charité Hospital, specializing in plastic surgery. Langenbeck’s successor, Ernst von Bergmann (1836–1907), was one of the most influential surgeons of his time, introducing the principle of asepsis to surgery. His guiding rule was that everything that came into contact with the operative field and especially with the surgical wound had to be absolutely sterile (Fig. 1.7). Jakob Lewin (Jacques) Joseph (1865–1934) was a pioneer of modern rhinoplasty. He studied medicine in Berlin, graduated in Leipzig in 1861, and opened a private practice in Berlin. Shortly thereafter, he joined the Berlin University Orthopedic Hospital, headed by Julius Wolff (1836–1902), where he received extensive surgical training. In 1896, he was referred to the hospital for the correction of prominent ears.12 In 1898, Joseph performed the first reduction rhinoplasty at his office, using an external approach. He also did pioneering work in several other areas, including the treatment of both morphological and functional abnormalities in one sitting, the use of intranasal approaches, and the establishment of aesthetic surgery as a medical specialty. It is “not vanity which is the driving motivation, but the feeling of being disfigured and, conversely, the aversion to disfigurement and its psychological consequences.”15 Rhinoplasty “seeks to cure psychological depression by restoring a normal shape to the nose. Its social importance is beyond question, and it represents a significant branch of surgical psychotherapy.” Fig. 1.10 The restored gravestone was consecrated by a ceremony in the Jewish cemetery in Weissensee, Berlin. In 1904, Joseph reported on the first operation in which the intranasal removal of a dorsal hump was combined with correction of the anterior septum.25 At that time, intranasal operative techniques were considered “unsurgical” procedures that were handicapped by poor exposure and a high infection risk (Fig. 1.8). From 1916 to 1921, Joseph was director of the Department of Facial Reconstruction at the Charité Ear and Nose Clinic in Berlin, headed by Passow (1859–1926).26,27 At that time, he worked mainly in the plastic reconstructive surgery of extensive facial injuries that were sustained during World War I. Owing to his great success, Joseph received an honorary professorship in 1919. Later, he started his own hospital and specialized in aesthetic surgery with an emphasis on rhinoplasty and mammoplasty. His colleagues included Gustav Aufricht and Joseph Safian.28 Jacques Joseph is considered the founder of modern rhinoplasty. Curiously, three professors named Joseph were working in Berlin at the same time. The nasal surgeon among them was popularly known as “Noseph” to distinguish him from his gastroenterologist and dermatologist colleagues. Aufricht later traveled to America, published numerous works, and became a respected nasal surgeon in the United States. He died in New York in 1984. Joseph summarized his experience in an atlas and textbook with the lengthy title “Rhinoplasty and Other Facial Plastic Surgery with an Appendix on Mammoplasty and Several Other Operations in the Area of External Plastic Surgery.” Joseph was buried in the Jewish Cemetery in Berlin-Weissensee, not far from our hospital. His gravesite was destroyed by bombs during World War II and considered as given up for many years. Joseph’s wife, Leonore, emigrated to the United States, where she died at a grand old age, impoverished, in 1968. In 2003, Walter Briedigkeit, a retired professor of pediatric cardiology from Berlin, found the destroyed gravesite and remnants of the gravestone of Joseph’s grave (see Fig. 1.9). During the international course “Essentials of Septorhinoplasty” in the same year, he initiated a worldwide campaign for collecting money for the restoration of the gravesite. The project was generously sponsored by many personal gifts and donations and by scientific societies such as the American Academy of Facial Plastic and Reconstructive Surgery and the European Academy of Facial Plastic Surgery. Great support during all activities of rebuilding the destroyed gravesite by the Privat-Institut für Medizinische Weiterbildung und Entwicklungen auf dem Gebiet der HNO-Heilkunde e.V Berlin (www.imwe-berlin.de) came from Gene Tardy Jr. On October 17, 2004, Joseph’s gravestone was consecrated by a ceremony in the Jewish Cemetery in Berlin-Weissensse (see Fig. 1.10). The stone reflects the eventful history of the grave: on the front is the new inscription on polished Swedish granite. The back of the stone has been left just as it was when it was found—broken, overgrown, damaged, with fragments of the original inscription.29–32 Diseases of the “internal nose” have their own history. The oldest documented record of medical treatment in which the patient and physician were named is that of the ancient Egyptian rhinologist Ni-Ankh Sekhmet, the physician to King Sahura, who presumably suffered from nasal polyps.33 For centuries, efforts were made to improve the dreaded, bloody techniques for the operative treatment of nasal diseases, especially nasal polyps. New instruments, approaches, and techniques were constantly devised for that purpose. This brought no real improvement, however, because surgeons knew little about the actual location and origin of the diseases. During the Renaissance, intense study was devoted to the anatomy of the skull, including the nose and paranasal sinuses (Leonardo da Vinci [1452], Vesalius [1514], Highmore [1651]).34 Many new discoveries were made about the human skull. In the late 19th century and early 20th century, the anatomical studies of Zuckerkandl (1882), Onodi (1893), and Grünwald (1925) yielded precise information on the anatomy of the nose, facial bones, and paranasal sinuses35–40 (Figs. 1.11 and 1.12). By first describing narrow anatomical passages in the ethmoid bone and middle meatus, Zuckerkandl promoted the development of new, endonasal operative procedures such as ostial enlargement, maxillary sinus fenestration, and ethmoid infundibulotomy.41–43 Gustav Killian, who became a professor in the Department of Otorhinolaryngology of the Charité Hospital in Berlin in 1921, already recognized the pathogenic significance of the anterior ethmoid cells. He introduced median rhinoscopy with a specially developed speculum for examining the middle meatus (Fig. 1.13). Without optical aids, the endonasal operations were hazardous and were practiced by only a few pioneers.41 The fact that other operative methods were developed at the same time was another reason for the lack of popularity of endonasal operations. Mikulicz was the first surgeon, in 1887, to open the maxillary sinus from the inferior meatus. Caldwell published his technique of maxillary sinus surgery in New York in 1893.44 Boenninghaus modified the technique by transposing a mucosal flap into the maxillary sinus window. Luc published the same operative technique as Caldwell in Paris.45–47 In 1867, Leinhardt described the first submucous resection of the nasal septum for correction of the anterior septum. Hartmann and Petersen expanded the method, also applying it to deviations of the posterior septum. The septum was approached through a horizontal and vertical incision of the mucosa on the deviated side. The major problem with this method and its refinements48 was the poor exposure caused by heavy mucosal bleeding. Rethi48 helped to control this problem by the local administration of cocaine.48–53 Killian injected a cocaine–epinephrine solution beneath the two mucosal layers and elevated the mucosa from the cartilage on both sides, developing the technique of the submucous resection.54 This procedure involved a broad resection of the septal cartilage, leaving a dorsal and caudal strut in place for support. It also involved removing portions of the bony septum (i.e., the perpendicular plate of the ethmoid and vomer) that were believed to obstruct nasal airflow.55 Special emphasis was placed on gaining “sufficient working room to resect the bony septal wall”56 (Fig. 1.14). The principle of the submucous resection was later abandoned because the over-resection of cartilage from the anterior septum tended to cause unfavorable late sequelae. Destroying the supportive function of the septum between the rhinion (keystone area) and the anterior nasal spine often led to depression of the cartilaginous nasal dorsum and retraction of the columella, with the functional and aesthetic problems of a saddle nose and hidden columella.18 Corresponding mucosal lesions or poor vascularization of the scarred mucosal layers led to perforations. When the supportive function of the cartilaginous septum is withdrawn, there is a general tendency for the mucosa to become dry and atrophic. Although the septal layers are located near the midline and the nose appears broadened, the rhinitis sicca still causes a subjective feeling of nasal stuffiness. Another problem is the “septal flutter” that occurs during forced respiration and phonation. In 1884, Sir Morrell MacKenzie founded the specialty of otorhinolaryngology when he published his first standard work on rhinology and laryngology.57 Rhinology began to be established as a separate field in the early 20th century. When the anatomical studies of Emil Zuckerkandl40 supplied the first accurate information on the structural anatomy of the nose and paranasal sinuses in the late 19th century, interest also grew in using endoscopy to explore the complex spaces of the nose and its connections with the paranasal sinuses. The first instruments used for this purpose were cystoscopes, because special endoscopes for the nose were not yet available. In 1901, A. Hirschmann first examined the maxillary sinus endoscopically through an enlarged dental alveolus, also examining the middle meatus.58 Despite the progress made in optical examinations, these initial steps in nasal endoscopy did not lead at once to new approaches in diagnosis and treatment. Substantial progress in these areas was not made until the postmortem studies of Walter Messerklinger59,60 on mucous transport in the human nose and paranasal sinuses. Such studies are possible because the respiratory epithelium continues to show ciliary activity for up to 48 hours after death. Messerklinger discovered that secretions from the large paranasal sinuses are transported along specific pathways to the ostia and flow from there through narrow passages in the lateral nasal wall to the mucosa of the nose.59,60 The nose and sinuses constitute a physiological and morphological unit. This principle seems obvious today, but before it was discovered, textbooks devoted separate chapters to diseases of the nose and diseases of the paranasal sinuses. In recent years, the nasal mucous blanket has again attracted special interest because of its central role in the hypothesis of fungus-induced sinusitis. Fungal spores are trapped by the two layers of the mucous blanket. They penetrate the mucus and reach the epithelial surface, where they evoke an eosinophilic reaction. A mucosal inflammation is incited by major basic protein and other cytokines, leading to polyposis.61 On July 16, 1959, a patent for the “rod lens system” was filed by its inventor, the English physicist Harold Horace Hopkins. It attracted considerable attention when unveiled as a new optical system at the Photokina photo exposition in Cologne. Karl Storz recognized the innovative potential of the invention for medicine and signed a licensing contract with Hopkins in 1965. The Hopkins rod lens system employs special glass rods with optically finished ends that replace conventional lenses. This has distinct advantages over a conventional lens system: better resolution and contrast, a wider viewing angle, superb clarity and brilliance, and an extremely fine depiction of details over the entire visual field.62 Messerklinger used the new endoscopes to examine the lateral nasal wall, where he observed both normal and abnormal mucosal findings. He discovered that recurrent and chronic sinusitis had a rhinogenic cause in the great majority of cases. This led him to develop an endoscopic diagnostic strategy for the nose and paranasal sinuses.63–65 Endoscopy could reveal the often subtle signs of mucosal inflammation, septal deformities located in the deeper areas of the nose, as well as anatomical factors predisposing to sinusitis. The pathways for the spread of rhinogenic sinusitis could be traced by endoscopic visualization. One challenge at this point was to make this optical pathway accessible for a new type of surgery. The endoscopic surgeon would be able to reach the pathogenic nidus of recurrent or chronic-hyperplastic sinusitis and, by restoring ventilation and drainage, create the conditions necessary for the hyperplastic epithelium of the functionally dependent sinuses (maxillary and frontal) to heal.66 The operative techniques and indications for this type of surgery have been constantly expanding along with the development of increasingly fine instruments and new endoscopes.8,67–70 Phylogenetically, the necessity of having a nose is based upon the transition from aquatic to terrestrial life. Originally, all vertebrates breathed through gills, but this type of respiration was preserved only in lampreys (agnathians) and fish. Ectothermic amphibians marked the metamorphosis from gill-breathing to lung-breathing animals, with only a few water-dwelling forms continuing to breathe with gills. Amphibians have other mechanisms of respiration through their gland-studded outer skin and oral mucosa. Reptiles are obligate lung breathers that have become independent of aquatic life and have adapted to various environments. Some groups, like the sea turtles, have returned to life in the water. The development of choanae, which are the morphological prerequisite for nasal breathing, first appeared in primitive amphibians and later arose in all vertebrates. This development is reflected in human ontogenesis. Through active growth, the epithelium of the nasal mucosa leads to the formation of the lateral nasal wall in the third month of fetal development. The rudiments of the nasal turbinates and paranasal sinuses also appear at this stage. Over the course of evolution, the human nose has developed into a highly efficient aerodynamic body with specialized functions.71–73 Only nasal breathing is physiological in humans. Mouth breathing tends to dry out the lower respiratory tract, predisposing to various diseases (pharyngitis, laryngitis, bronchitis, bronchial hyperreactivity, asthma). The nose has an immense regulatory capacity. Although the mucociliary apparatus is affected by the temperature and humidity of the inspired air and by the pH and osmolarity of the surrounding medium, air entering the nose is warmed to a relatively constant 31 to 34°C in the epipharynx. This occurs largely independently of the external temperature.74 The nose also humidifies the inspired air to a relative humidity of 90 to 95%.75 Most warming and humidification takes place in the anterior part of the nose.76 Both functions are linked to the ability of the nose to undergo rapid changes in cross section. The nasal mucosa is the “front line” of the human immune system. With each breath, it responds to and defends against a variety of antigens and allergens. The mechanisms of this response include nonspecific (e.g., interferon, protease inhibitors) and specific humoral reactions (immunoglobulins A, M, and G), as well as cellular reactions by macrophages, mast cells, and granulocytes. At the same time, entirely different reactions such as absorption and secretion can take place on the mucosa. The phylogenic development of the upper and lower airways accounts for their functional interrelationship. The upper and lower airways form a functional unit. The mucosa, submucosa, and vascularity are similar in both regions. Also, the biochemical control mechanisms in the upper and lower airways have the same mediators. The mucosa of both the upper and lower airways responds to allergic and physical stimuli, chemical irritants, and inflammatory microbial irritants with cellular infiltration (mostly eosinophilic granulocytes), mucosal edema, and increased mucus production.77,78 The time required for a mucosal disease to “change levels” by spreading to the posterior wall of the pharynx, trachea, and bronchi varies in different individuals. The rhinologist should always keep in mind the principle of one airway, one disease78 (Fig. 1.15). The area of respiratory epithelium located in the human olfactory groove measures approximately 2 × 5 cm. This area is many times larger in numerous mammalian species. In the speechless world of animals, the olfactory sense is the most important means of communication next to vision. Humans have approximately 10 million olfactory cells. These are bipolar sensory cells with an elongated cell body and a short process, the dendrite, with numerous cilia extending into the nasal mucous blanket. At the opposite end of the cell is a long neural process, the axon. The olfactory cells are classified as primary sensory cells. The axons pass through the basement membrane of the olfactory epithelium and join to form the fila olfactoria. These filaments pass through the cribriform plate to enter the olfactory bulb in the brain. There they synapse with the dendritic tree of the mitral cells. Approximately 1,000 olfactory cells converge toward one mitral cell. The processes of the approximately 60,000 mitral cells form the olfactory tract, which passes to the olfactory cortex, the primitive rhinencephalon. Information is relayed from there to the thalamus, hypothalamus, and amygdala. This intimate contact with the hypothalamus, which controls behavior patterns such as eating, drinking, sexual behavior, hormonal regulation, and the perception of emotions, probably explains why olfactory stimuli have rapid and direct access to the deepest centers of human emotion. Information is relayed from the thalamus to the neocortex, where the pathways terminate in old, nonspecific brain regions.79,80 The human olfactory sense is less rooted in the conscious mind than seeing and hearing, for example. Fig. 1.15 The mucociliary apparatus of the respiratory epithelium is an important defensive and regulatory mechanism of the nose. Goblet cells and seromucous glands secrete a substance onto the surface of the mucosa, forming a two-layer film. The beating cilia located in the deeper, less viscous mucous layer actively propel the superficial, more viscous layer toward the esophagus. Generally speaking, olfaction must still be considered the “neglected” sense. The analytical perception of visual and auditory stimuli is constantly being trained and reinforced, whereas the processing of odors is a more intuitive process.2,81 Cortical representation in the phylogenically old brain areas of the limbic system establishes a close, essentially nonverbal link with affect, emotions, and distant memories. For example, the smell of freshly polished linoleum can bring back vivid memories of grade school simply because that is how the school used to smell. Often it is difficult to describe an odor in words, and the best we can do is compare the smell to something else or describe it as “flowery,” “fruity,” etc. The olfactory epithelium can regenerate within 100 days, which is unique for sensory organs. The sense of smell, like other senses, demonstrates the phenomenon of adaptation. The sensitivity of olfaction also depends on hunger. A very hungry individual can perceive several olfactory stimuli better than one who has eaten. This is a useful physiologic regulation mechanism.82 In the isthmic region of the limen nasi, the inspired air is slowed and separated into two streams. The main stream is directed over the nasal floor to the choana. A smaller stream is directed upward and sweeps over the dorsum of the inferior nasal turbinate. At this point, the air is warmed and continues to move upward. On reaching the head of the middle turbinate, the “updraft” splits into a lateral stream that ventilates the paranasal sinuses and another stream that is directed medially upward. The alignment of the middle turbinate is crucial for ventilation of the olfactory groove. It has the shape of an airfoil suspected between three points of attachment. A negative pressure prevails on the medial or “lee” side of the turbinate, causing the inspired air to rise into the olfactory fossa. Gustatory olfaction is subject to the same basic flow patterns following convection of the flow around the body of the turbinate (see Fig. 1.16). Respiratory hyposmia can result from obstruction or deficient aeration of the olfactory groove caused, for example, by septal deviation, polyps, or tumors. Deformities of the nasal turbinates (e.g., lateralization, atrophy, paradoxical curvature) can also lead to hyposmia (Fig. 1.16). Richard Axel and Linda Buck were the first to examine the sense of smell at the molecular level. They discovered that every olfactory cell is specialized for only a single class of scent and is equipped with only one type of receptor. Human beings have 350 types of receptor. One receptor can recognize up to a hundred molecules with structural similarities. Scent molecules have to fit into a receptor like a key into a lock. Docking of a molecule activates a chemical cascade. The scent is transformed into an electric signal, which is transmitted to a scent center in the brain (see Fig. 1.17a, b). The two scientists were awarded the Nobel Prize in 2005 for this discovery.82 A. Butenandt, the Nobel Prize winner from Munich, coined the term pheromones for molecules that are produced by a species and evoke certain reactions in animals of the same species. The vomeronasal organ (Jacobson’s organ) is essential for the social and mating behavior of all mammals.83 Except for some higher primates, mammals mate only when the female is fertile. Information on the timing of ovulation is conveyed to males by means of pheromones. Numerous observations and studies indicate that pheromones also convey signals in humans. The vomeronasal organ consists of tiny, paired, blindly terminating canals located in the anterior nasal septum. Its morphology suggests that the vomeronasal organ is a functioning sensory epithelium. Further studies are needed to identify its central connections with the hypothalamus and elucidate its functional significance.84 Several prerequisites have been essential in developing a common concept in rhinosurgery that places equal emphasis upon functional and aesthetic demands. The nasal septum is the central connecting link between the internal and external nose.85,86 It supports the lateral cartilages and provides a secure attachment of the cartilaginous nose to the facial skeleton between the rhinion (keystone area) and the anterior nasal spine, premaxilla, vomer, and perpendicular plate of the ethmoid. The successful correction of axial deformities of the nose is not possible without fully utilizing the capabilities of the submucous septoplasty. Aufricht87 said: “Where the septum goes, there goes the nose.”88 This is equally true for the reconstruction of saddle nose deformities, where a stable buildup of the septum is the key to a successful outcome. While the nasal septum may be affected by numerous deformities, three patterns are most commonly encountered (Fig. 1.18): • The septum is too long in the basal-to-dorsal direction. This situation is common in the overprojected nose and functional tension nose with hyperplasia of the upper lateral cartilage or alar cartilage. • Phylogenically, the connection between the vomer and basal septal cartilage is a zone of “tectonic unrest.” Originally, it had the form of an articulation.73 Even slight growth or forward movement of the vomer, usually during puberty, leads to elevation of the cartilaginous nasal dorsum due to the wedged shape of the underlying vomer or to characteristic vomerine ridges that run obliquely upward. Fig. 1.17 (a) 1, scent molecules; 2, scent receptors. Each olfactory cell bears only a single type of receptor in humans. A receptor can recognize up to 100 structurally similar molecules in a scent category. (b) Scent molecules only fit one specific receptor. They trigger a biochemical reaction and a subsequent electrical signal, which is transmitted to the olfactory center in the brain. Reproduced from Behrbohm H, Kaschke O, Nawka T, and Swift A. Ear, Nose and Throat Diseases: With Head and Neck Surgery, 3rd edition © 2009 Georg Thieme Verlag/Thieme Publishers. • The septum is too long in the craniocaudal direction. This situation is often seen in axial deformities and is associated with two sites of nasal airway obstruction. Subluxation is common (Fig. 1.18). The external shape of the septum can be selectively modified in septal operations. Resections of the anterior septal margin can be helpful in shortening the nose and in establishing a symmetrical nasal tip with an equilateral rhomboid shape. An infratip triangle that is too long can be shortened. Also, the anterior septal margin can be beveled to rotate the tip upward and accentuate the double brea k in the nasal profile. Septal modification is an essential part of creating a subtle, aesthetically pleasing supratip break in women.3 Cottle (1948) introduced his cartilage-conserving operation as an alternative to the Killian septal resection (see pp. 6 and 7). The Cottle operation attempts to preserve the supporting function of the septal cartilage and the physiological function of the nasal mucosa. After the anterior margin of the septum has been exposed, the mucoperichondrium is undermined to create a superior tunnel on the left side and an inferior tunnel on both sides. The mucosa remains adherent to the septal cartilage on the right side. This provides good septal mobility. The classic Cottle operation has been continually modified over the years. One modification is the swinging door technique in which the septal cartilage is detached just anterior to the perpendicular plate to increase the mobility of the cartilage during the operation (Fig. 1.19a). The mucoperichondrium is left in place. Also, small strips or wedges can be excised from the cartilage to eliminate redundant material that would create undesired stresses. The cartilage can also be scored or cross-hatched to modify its bending properties. In our experience, a large percentage of septal deviations can be managed with this technique. For greater, sharp-edged deviations that are combined with axial deformities, the mucosa can be completely elevated from the septal cartilage to form two superior and inferior tunnels in preparation for an extracorporeal septoplasty.89 In this technique, the cartilaginous and bony septum is completely removed, straightened, stabilized for instance with spreader grafts and reimplanted and fixed by sutures at the k-stone region and the anterior nasal spine. A compound graft is made by suturing pieces of septal cartilage in a mosaiclike pattern to a sheet of polydioxanone suture material (PDS). This sheet gives the composite implant the necessary mechanical stability until the material is absorbed.89,90 A complete tunneling of the nasal septum is useful in deviated noses, because the unwrapping effect might help to analyze and correct deviations. If the potential of the septoplasty is to be fully realized in terms of improving function and aesthetics, this procedure must take the form of a technically demanding plastic operation. As Adamson put it, “The only easy septum is the one which has no need to be done”88 (Fig. 1.19a). Traditionally, the main argument against septal surgery in childhood has been the belief that the septal cartilage is an essential pillar for the primary growth of the midfacial region.91 Today it is known that the septum, maxilla, and premaxilla develop independently of one another.92,93 Strict criteria should be applied in selecting children for septal operations. Nevertheless, even small children can be successfully operated for traumatic deformities or malformations of the septum that cause significant nasal obstruction. Deformities of the anteroinferior septum are the most common problem.94 It is important that the surgery preserve the perichondrium, the growth zones (e.g., the caudal septum), the premaxilla, and the sutural junctions with the perpendicular plate and vomer.95 The pediatric septum consists mainly of the quadrilateral plate; the vomer and perpendicular plate are relatively small. This calls for an atraumatic, chondroplastic mode of surgery. Pieces of cartilage that are removed should be straightened and reimplanted. Even after surgical trauma, the septal cartilage still has considerable regenerative capacity.93 As early as 1882, Zuckerkandl described the nasal valve as follows: “The fold of the upper lateral cartilage and the wall of the nasal septum form a space leading into the nasal cavity that is much narrower than the external naris.” Mink called this area the nasal valve because of its dynamic function in regulating the cross-sectional area of the nasal airway.20,40 The resistance to nasal airflow is to a large degree determined by the nasal valve.19 Over the years, numerous operations have been described for widening the nasal valve and preventing alar collapse.45,96–100 A history of obstructed nasal breathing plus visual inspection of the external and internal nose (preferably with an endoscope) will direct attention to the underlying problem and suggest the best technique for widening or stabilizing the nasal valve. A positive Cottle maneuver indicates a problem with the nasal valve: when the ala is pulled laterally upward, the nasal valve opens and breathing improves (Fig. 1.20). Some surgical techniques to enlarge or stabilize the internal nasal valve are shown in Fig. 1.21. Fig. 1.20 The flexible structure of the nose and the nasal valve. The flexibility of the nose increases in the craniocaudal direction. The bony portion is completely rigid, and the flexible cartilaginous portion begins at the rhinion. The distal caudal lateral cartilages are mobile and similar to the wings of a butterfly. This flexibility is supported by the upper alar cartilages, which perform an important supporting function medially and distally along with the septum. This arrangement imparts a special functional elasticity to the nasal valve. The nasal skin shows an opposite pattern: it is thin and mobile over the bony nasal pyramid but is relatively thick and immobile over the nasal tip. Neither “internal” nor “external” nasal operations should needlessly traumatize this sensitive system of flexible and inflexible elements. Our experience in the treatment of speed skaters at the Olympic Center in Berlin has demonstrated an interesting phenomenon. Good nasal breathing is particularly important in this sport, where very cold, dry air is forcibly inspired in short, deep breaths taken through the mouth or through the nose and mouth combined. Twelve top athletes who had septal deviation, turbinate hyperplasia, inflammatory ethmoid changes, or an anatomical variant (concha bullosa, paradoxical curve of the middle turbinate, pneumatized agger nasi) underwent a septoplasty that usually included an endoscopic ethmoidectomy or turbinate reduction. But even patients who showed very good postoperative nasal breathing by rhinomanometry reverted to oronasal breathing during exercise. The reason is a physiological collapse of the nasal valve that occurs with extreme inspiration to protect the lower airways and lungs from unconditioned air that is too cold or too hot. Activation of the sympathoadrenergic system in response to physical exercise leads to a decongestion of the nasal mucosa. This results in increased airflow through the nose and a lowering of nasal resistance, accompanied by an acceleration of mucociliary secretion.71 Nevertheless, the resistance to open mouth breathing is still less than the resistance to nasal breathing. The athletes adopt a combined oronasal mode of breathing that includes a degree of nasal breathing while regulating the airway resistance so that the work of respiration (pressure and volume) does not become too great6,101–103 (Fig. 1.22). The description of new principles of rhinoplasty, especially by Tardy, has changed the fundamental character of this surgery.104–107 The key is a detailed analysis of the presenting anatomical problems, taking into account other fundamental factors such as skin type, connective-tissue type, and the age of the patient.108 Surgical access is gained through adequate approaches that are as minimally invasive as possible. The surgery is structure-conserving and aimed at preserving and reorienting the cartilages. The strategies include circumscribed resections and the use of suture and graft techniques to shape the nasal tip. Any unnecessary tissue trauma is avoided. The following measures are helpful in achieving these goals: • Selective, local vasoconstriction is added to general anesthesia to minimize bleeding. • Osteotomies are performed with micro-osteotomes that do not damage the periosteum or the overlying vascular and muscle plane. Traditional transverse osteotomies are avoided. • Intranasal sutures or splints eliminate the need for laborious packing.109 Fig. 1.22 Typical combined oronasal breathing, demonstrated by five-time Olympic ice-skating gold medalist, Claudia Pechstein. • By minimizing tissue trauma, intraoperative bleeding is reduced. A well-defined surgical concept based on an analysis of the specific morphological problem and of preoperative photographs helps to shorten the operating time. Less bleeding and shorter operating times are the prerequisites for expanding the range of indications for rhinosurgical operations that include endoscopic microsurgery. An understanding of the tip-supporting mechanisms will protect against unnecessary destabilization of the nasal tip and dorsum during the operation. The dynamics of rhinoplasty refers to a system of surgically induced interactions to fine-adjust the position of the nasal tip. Dissection strictly in the favorable surgical planes can minimize unnecessary bleeding, edema, and subsequent scarring.110 The task of the surgeon is to lay the groundwork for a stable long-term result.107,111–113 Disturbances of olfaction are the second most common leading symptom of nasal obstruction reported by our patients. Olfactory disturbances may be described as quantitative or qualitative. Hyposmia and hyperosmia signify a change in the olfactory threshold, while anosmia denotes an absence of the smell sensation. This may affect the perception of certain odors or of all smells. Parosmia refers to an altered perception of smells under certain physiological conditions, such as pregnancy. Pseudosmia refers to the misidentification of perceived smells, as in cacosmia. Phantosmia is an olfactory hallucination, or the perception of an odor with no stimulus present. In anosmia, olfactory information is perceived but is not recognized. The most important distinction for the rhinosurgeon is between respiratory and sensory hyposmia.2,81 The modern classification distinguish two kinds of olfactory disorders: sinonasal olfactory disorders and nonsinonasal olfactory disorders. These are the most common disorders encountered in otorhinolaryngology. Inflammatory or noninflammatory changes impede the transportation of scents to the olfactory epithelium directly. • Infectious causes: chronic rhinosinusitis. • Noninfectious causes: allergies, polyposis, hyperplastic rhinosinusitis, postirritative and toxic, postinfectious, rhinitis sicca. • Noninflammatory causes: anatomic (malignant and benign tumors, stenosis, choanal atresia, adhesions, septum deviations) or nasal congestion, idiopathic rhinitis, side effects of drugs. Viral infections can lead to primary damage to the olfactory cells. Typically, patients experience a subjective loss of the sense of smell immediately after an infectious disease. Neurologic, congenital, toxic, and psychiatric conditions may involve olfactory disorders, as well as head injuries. Dysosmias may be an initial symptom of Alzheimer’s disease, preceding loss of cognition, and abnormal behavior. In Parkinson’s disease, olfactory disorders often occur before motoric disorders. Noxious substances such as carbon dioxide, formaldehyde, or tobacco smoke can directly damage the olfactory cells. Congenital dysosmias (e.g., Kallmann syndrome) are rare.82 Olfactometry should precede every surgical operation on the nose or paranasal sinuses. First, a precise case history is taken that includes triggering events, associated symptoms, relevant illnesses, operations, drugs, and noxious influences. This is followed by nasal endoscopy, with exploration of the nasopharynx and olfactory cleft. Assessment of olfactory function is based on a standardized, validated test. We prefer the Kobal Sniffin’ Sticks.114,115 Sixteen scents on felt-tip pens are presented to the patient, who is asked to identify them. This test is widely used in Europe. It combines threshold, identification, and discrimination of scents. The identification test is suitable for screening. For more information about clinical olfactory tests, you may refer to the textbook Ear, Nose, and Throat Diseases.82 Active anterior computerized rhinomanometry with a decongestion test can be used to differentiate between fixed stenoses, dynamic stenoses, and pseudostenoses. In our practice, rhinomanometric measurements are an indispensable tool in selecting patients for septoplasty or septorhinoplasty.2 Computed tomography (CT) in the coronal plane or a digital volume tomography provides an excellent overview of the ethmoid region and paranasal sinuses. The marked individual variations in the degree of ethmoid pneumatization can be appreciated on CT scans. CT can also demonstrate pathological mucosal changes, the relative locations, and special features of major structures like the optic nerve, the presence of Onodi cells, the depth of the olfactory fossa, and the distance from the medial infundibular wall to the orbit. Thus, CT can provide both an inventory of pathological changes and a “roadmap” for endoscopic operations. Nasal endoscopy, with its ability to explore the internal nose, has become an essential tool for modern finding-oriented rhinological diagnosis and treatment. The endoscopist looks for signs of inflammatory mucosal disease such as abnormal mucous tracks, areas of mucosal edema, or mucosal polyps on the lateral nasal wall. Attention is also given to anatomical variants of pathogenic significance such as conchae bullosa or paradoxical middle turbinates. Nasal endoscopy also permits the topographic evaluation of aerodynamic obstructions such as ridges or spurs on the posterior septum or perpendicular plate, nasal valve stenosis, and alar collapse. • Large deviations of the nasal septum. • Septal deviation with compression or lateralization of the middle turbinate. • Prominent spurs and ridges. • Nasal and sinus polyps. • Papillomas. • Morphological variants of the middle turbinate (e.g., concha bullosa, large pneumatized labyrinth-turbinate complex). • Synechiae. • Rhinitis sicca. Surgical manipulations in the olfactory groove should be carried out with extreme care. Olfactory and respiratory epithelia are indistinguishable from each other. The Storz minishaver has proved especially useful for operations in the olfactory groove. Floating tissue is aspirated into the window of the outer sheath and cut off cleanly with a rotating blade. The sheath protects the opposing mucosa from accidental injury. Significant deviation of the nasal septum, like that often found in axial deformities of the nose, is a predisposing factor for recurrent sinusitis. Fig. 1.23 illustrates the most important cellular structures and their variants that may have causal significance in recurrent sinusitis. Endoscopic surgery of the paranasal sinuses is a minimally invasive microsurgical operating technique. Dissection through a well-exposed field will cause minimal intraoperative bleeding. With some practice and good anatomical orientation, it is our experience that endoscopic microsurgery and septorhinoplasty can be effectively combined. The recommended sequence of surgical steps is shown below, based on the example of a long, humped nose: 1. Decongestion of the nasal mucosa with nose drops. 2. Local anesthesia plus vasoconstriction of the external nose and septum. 3. A pledget soaked with tetracaine and epinephrine is placed in each naris for 10 minutes for vasoconstriction. 4. Infiltration of the lateral nasal wall under endoscopic control. 5. Endoscopic microsurgery of the ethmoid and paranasal sinuses, including adjunctive measures. This presumes that a strong septal deviation is not obstructing the middle turbinate. The beginner can determine this by noting whether a 4-mm telescope can be easily positioned at the antrum of the middle meatus. If not, a submucous septoplasty should be performed first. 6. A pledget is inserted into the ethmoid at the end of the ethmoid surgery. 7. Submucous septoplasty is carried out, usually through a hemitransfixion or superior transfixion incision, paying attention to aesthetic aspects such as: a) Shortening the entire caudal or dorsocaudal edge to shorten the nose, reducing an infratip triangle that is too long, or tip rotation. b) Resecting a narrow basal strip to relax a tight nasal valve. c) Removing or shortening the nasal spine if there are signs of vestibular tension or an obtuse nasolabial angle. The soft tissues of the nasolabial angle are augmented as required. 8. The nasal tip and dorsum are accessed through a nondelivery or delivery approach or an open approach. In the splitting approach, the transcartilaginous or intercartilaginous incision is combined with a hemitransfixion or transfixion incision. The intracartilaginous incision may also be combined with these incisions (e.g., for a delivery approach). 9. The nasal tip is corrected, according to the anatomical situation. 10. The cartilaginous hump is removed first, then the bony hump. 11. Medial oblique and lateral curved osteotomy. Fig. 1.23 Anatomical variants of the ethmoid that may contribute to the pathogenesis of recurrent sinusitis. 1. Cells of the medial orbital wall. • Large ethmoid bulla, often in contact with the middle turbinate. • Orbital ethmoid cells near the maxillary sinus ostium. • Frontal cells. 2. Variants of the uncinate process. • Shape: free-standing, varying curvature, length, and thickness. • Insertion: lamina papyracea, anterior skull base. • Pneumatization. 3. Middle turbinate. • Pneumatization: head, neck, attachment. • Curvature: paradoxical. 4. Septum. • Deviation: anterior, posterior, high, low. • Ridge: vomer, traumatic. • Prominent premaxilla. • Septal tubercle. 5. Agger nasi. • Pneumatization. 6. Combination of several variants. A detailed endoscopic evaluation is an essential prelude to microsurgery of the lateral nasal wall and paranasal sinuses. The endoscopic and imaging findings provide the basis for designing an individualized concept for operative treatment. The value of this endoscopic–microsurgical concept is that it provides the means for detecting and eliminating the often subtle causes of recurrent or chronic inflammatory diseases of the maxillary, frontal, and sphenoid sinuses. The mucosal pathology begins in the anterior ethmoid and spreads from there in a centrifugal pattern. Foci of mucosal edema in the tight spaces of the lateral nasal wall hamper mucous drainage from the frontal and maxillary sinuses, causing infected secretions to dam back. If the mucosal disease persists, the edematous foci become organized. This leads to disturbances of the mucociliary apparatus such as restricted ciliary beating and rheological mucus changes. These are followed by morphological mucosal changes such as an altered ratio of ciliated cells to goblet cells, loss of cilia, and mucous transformation of the seromucous glands (Fig. 1.24). Fig. 1.24 Phases of the generation of a nasal polyp from the anterior ethmoid: • Mucosa inflammation, edema. • Subsidence of the growing polyp. • Obstruction of the middle meatus, the anterior ethmoid, and compression of the polyp tissue. • Complete nasal obstruction. This sets up a vicious circle that should be interrupted as soon as possible to halt the spread of inflammation to the entire ethmoid labyrinth and to the frontal, maxillary, and sphenoid sinuses. The goal of mucosa-conserving surgery is to create the conditions necessary for morphological and functional reparative processes to occur in the epithelium. The metabolic products of eosinophilic granulocytes are toxic to the epithelium and play a central role in the pathogenesis of chronic hyperplastic rhinosinusitis. A mixed-cell inflammation is perpetuated by immune mechanisms, in most cases by T lymphocyte–activated eosinophilic granulocytes. Against the backdrop of these immune responses, eosinophil-associated “rhinosinubronchopathy”—especially the triad of analgesic intolerance, bronchial asthma, and sinonasal polyps, the Samter’s triad—should be viewed as a separate disease entity.78 Surgery in these cases is only one component of a treatment concept consisting of finding-oriented endoscopic aftercare and topical medical treatment, with systemic therapy added in selected cases. Based on our experience in more than 3,000 simultaneous septorhinoplasties with endoscopic microsurgery of the paranasal sinuses, we can recommend the following indications: Indications • Recurrent ethmoid and maxillary sinusitis. • Recurrent ethmoid and frontal sinusitis. • Chronic hyperplastic sinusitis with circumscribed mucosal changes. • Cysts of the maxillary and sphenoid sinus. • Postinflammatory or postoperative synechiae. As a general rule, any complications of inflammatory diseases, tumors, and suppurative inflammations should be excluded prior to the simultaneous operative treatment of extensive pansinusitis. Revision procedures (e.g., of the ethmoid or frontal sinus) for mucoceles or obliterative scarring of the frontal recess should be performed separately. One should never compromise the functional or aesthetic outcome in order to achieve a one-stage operation. Contraindications • Chronic hyperplastic pansinusitis. • Acute exacerbation of chronic or recurrent sinusitis. • All types of complication (orbital, central, vascular). • Tumors. • Revisions. The complication of endoscopic endonasal microsurgery can be classified as orbital, central, or vascular. The most frequent orbital complication is injury to the lamina papyracea, resulting in a hematoma of the upper or lower eyelid. If the periorbita is injured, orbital fat will herniate into the ethmoid cells. The ocular compression test described by Stankiewicz can be used to assess the magnitude of the injury.116 It is important for the surgeon to detect any orbital injuries at once so that the use of sharp and cutting instruments can be avoided. If an orbital perforation is suspected, the eye should be opened to check for concomitant movement of the globe. Lesions ≥ 0.4 cm2 should be repaired with fascia or perichondrium, while smaller lesions can be covered with mucosa. Injury to the anterior ethmoid artery can lead to the formation of an intrabulbar or retrobulbar hematoma. In severe cases, the associated effect on intraorbital pressure can lead to blindness. The best first aid in these cases is to compress the orbital contents with external pressure on the closed eyelid. If this does not stop the hemorrhage, the pressure can be relieved by a lateral canthotomy or endonasal incision of the periorbita. The bony canal of the optic nerve forms a typical prominence in the lateral wall of the sphenoid sinus. It may also encroach upon the posterior ethmoid, especially in the presence of Onodi cells. This is the area in which most optic nerve injuries occur. Pupillary response should be checked during the operation. Direct or indirect injuries are manifested by a reflex mydriasis. Injuries to the orbit always require specific or empirical antibiotic therapy as an adjunct.117–119 CSF leak is the most common intracranial complication. Particular danger sites are located in the cribriform plate and anterior skull base at the level of the canal of the anterior ethmoid artery. The skull base is very thin in that area, and the surgeon approaches it directly after opening the anterior ethmoid. The surgeon should be alert for any leakage of the colorless fluid. Small defects can be covered with free grafts of nasal or turbinate mucosa. Lesions of the bony skull base larger than 4 mm should be repaired with autologous fascia lata harvested from the thigh. Fibrin glue is excellent for attaching the graft. The fascia should be supported for 1 week with antibioticimpregnated packing. Coverage with an antibiotic agent that will enter the subarachnoid space is also required. The most serious vascular complication is injury to the carotid artery in the lateral wall of the sphenoid sinus. The surgeon should take every precaution to avoid this disaster. This includes the use of coronal CT scans and high-performance endoscopes with a wide-angle view that will encompass peripheral surgical landmarks. Even when opening the sphenoid sinus, the surgeon should proceed very carefully while noting key landmarks such as the attachment of the middle turbinate, the choana, the sphenoethmoid recess, and the posterior ethmoid artery.120 When dissecting in the ethmoid labyrinth, the surgeon should always work in a medial and caudal direction. The sphenoid sinus is not always the last posterior ethmoid cell, and the latter may project past the sinus. The posterior ethmoid cell may even be larger than the sphenoid sinus itself. The sphenopalatine artery runs level with the floor of the sphenoid sinus and may bleed profusely when injured. This vessel is easy to locate, however, and can be coagulated with a bipolar cautery even through the mucosa. The anterior and posterior ethmoid arteries may or may not traverse a bony canal in the anterior skull base. The vessels are easily identified and can be coagulated. There is a danger of vessel retraction into the orbit.66,70 Based on author’s own experience, the following procedures and the principles of biostatic surgery can be recommended in simultaneous procedures. The biostatic surgery is based on the principles of FESS described by Messerklinger und Stammberger.59,60,63–66,121 The ethmoid bone is a suspended, lightweight frame structure that forms the ethmoid sinuses and gives central support to the midfacial region (see Fig. 1.25). It has a T-shaped configuration in which the vertical member is formed by the perpendicular plate of the ethmoid bone and the horizontal member is formed by the paired ethmoid labyrinths.122
The Dual Character of Nasal Surgery
1 The Dual Character of Nasal Surgery
1.1 Introduction
1.2 Historical Review
1.2.1 Origins of Plastic Nasal Surgery
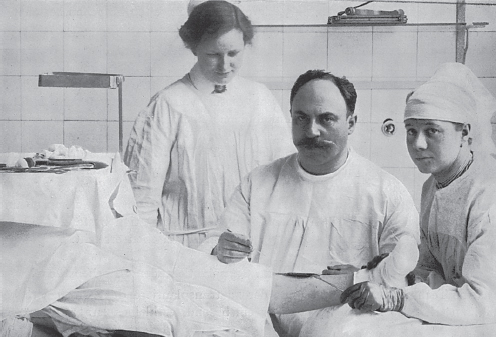
1.2.2 The Development of Plastic Surgery in Berlin and at the Charité Hospital from the 18th to 20th Centuries
1.2.3 History of Surgery of the “Internal Nose”
1.3 Phylogenesis
1.4 The Nose as a Respiratory Organ
1.5 The Nose as a Sensory Organ
1.5.1 The Olfactory Sense
Sense of Smell at the Molecular Level
1.5.2 The Vomeronasal Organ
1.6 Prerequisites for the Concept of Functional-Aesthetic Nasal Surgery
1.6.1 Septal Surgery with Functional and Aesthetic Goals
1.6.2 Principles of Submucous Septoplasty
1.6.3 The Pediatric Nasal Septum
1.6.4 The Nasal Valve
1.6.5 Physiological Limits of Nasal Breathing
1.6.6 Atraumatic, Structure-Conserving Techniques of Septorhinoplasty
1.7 Functional Aspects of Septorhinoplasty
1.7.1 Olfactory Disturbances
Sinonasal Olfactory Disorders
Nonsinonasal Olfactory Disorders
Basic Diagnostic Workup of Olfactory Disturbances and Paranasal Sinus Diseases
Olfactometry
Computerized Rhinomanometry
Computed Tomography
Endoscopic Examination of the Nose
Frequent Causes of Respiratory Hyposmia
Surgery in the Olfactory Groove
1.7.2 Recurrent and Chronic Sinusitis
Endoscopic Surgery of the Paranasal Sinuses
Algorithm for Simultaneous Septorhinoplasty and Endonasal Microsurgery
Principles of Endonasal Microsurgery
Indications
Contraindications
Complications
Orbital Complications
Intracranial Complications
Vascular Complications
Biostatic Endoscopic Surgery
Plastic Surgery Key
Fastest Plastic Surgery & Dermatology Insight Engine