CHAPTER 4 The Diagnosis and Treatment of Entropion
Introduction
There are four types of entropion (Box 4-1). A congenital form of entropion exists, but it is so rare that it is hardly worth mentioning.
We will discuss the anatomy of the lower eyelid as it relates to the causes of entropion in some detail. The two most important causes of involutional entropion are horizontal lid laxity and disinsertion or laxity of the lower eyelid retractors. As discussed in Chapter 3, any horizontal laxity of the eyelid contributes to instability. Without the normal tension of the lower eyelid retractors pulling the lower edge of the tarsus inferiorly and posteriorly, the eyelid may invert. The concepts of anterior and posterior lamellar shortening are also important in the discussion of entropion. Scarring of the posterior lamella, conjunctiva, and tarsus causes a cicatricial entropion.
Cicatricial entropion is less common than involutional entropion. Trachoma is the “textbook” cause of posterior lamellar scarring that leads to cicatricial entropion. Trachoma is rarely seen in the United States. The typical patient with cicatricial entropion has severe conjunctival scarring with the eyelid margin inverted, causing skin and lashes to rub against the eye. In reality, the patient with the most commonly seen type of cicatricial entropion has a mild form, called marginal entropion. The eyelid margin is turned in slightly, bringing the lashes against the eye. We will spend a considerable amount of time covering marginal entropion in Chapter 5. The aim of treatment of all forms of cicatricial entropion is to restore the normal length of the posterior lamella using either incisions alone or incisions with grafts. The tarsal fracture operation is a great procedure to add to your list of competencies for repair of marginal entropion or mild degrees of cicatricial entropion of the lower eyelid. We will also talk about an upper eyelid everting incisional procedure called the terminal tarsal rotation operation. When the entropion is too severe for incisional lengthening, mucous membrane grafts are necessary. You should learn to recognize patients with severe entropion who will need the more advanced operations involving grafting. It is not likely that you will do many of these grafts.
Spastic entropion is an unusual form of eyelid entropion. You will occasionally see this form of entropion occurring with squeezing of the lids in association with ocular pain or inflammation, often after eye surgery. Frequently, the entropion resolves as the postoperative discomfort disappears. If corneal irritation is severe, treatment with Quickert sutures will return the lid to its normal position. Although you won’t see many patients with spastic entropion, Quickert sutures are easy to learn and are an easy solution for spastic entropion.
Anatomic considerations
The normal eyelid margin
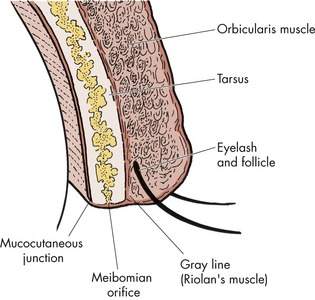
Understanding exactly how the eyelid sits against the eyeball is important for understanding cicatricial entropion. We take the eyelid margin for granted, but there is a very specific relationship between the mucosal tissues on the back of the lid and the keratinized skin on the lid margin. The next time you are performing a slit lamp examination, start to become familiar with this eyelid margin anatomy. The normal eyelid margin is flat, ending at right angles anteriorly and posteriorly to form a long thin rectangle of tissue (Figure 4-1). The most posterior aspect of the normal lid margin is the mucocutaneous junction. It is at this point that the mucosa of the palpebral conjunctiva stops and the keratinized skin of the eyelid margin begins. Look at several normal patients to see this junction. The next time you see a patient with cicatricial entropion, you may be able to appreciate the fact that the mucocutaneous junction moves forward as the eyelid margin inverts (Box 4-2).
Just anterior to the mucocutaneous junction are the meibomian gland orifices extending out from the tarsal plate. Evert the eyelid during the slit lamp examination, and you will see the faint vertical lines of the meibomian glands visible in the tarsal plate. Anterior to the meibomian gland orifices is the gray line. Initially, this line was thought to result from the fusion of the anterior and posterior lamella. In reality, the gray line is a specialized muscle of the pretarsal orbicularis, known as the muscle of Riolan. The gray line is still used as a landmark to surgically separate the anterior and posterior lamella of the eyelid in some procedures. You will recall that posterior to the gray line is the posterior lamella (the tarsus and the conjunctiva). Anterior to the gray line is the anterior lamella (the skin and muscle). The eyelashes arise anterior to the gray line, usually in one or two irregular rows in the lower lid and three or four irregular rows in the upper lid. The eyelash follicles originate on the surface of the tarsal plate. Learn these subtle anatomic features of the eyelid. They are especially important when you are evaluating patients with mild cicatricial entropion or trichiasis. We will emphasize the changes that occur in the lid margin later in this chapter and more completely in Chapter 5.
The stable lower eyelid
Let’s go over the anatomic factors that are important for understanding and treating entropion. Remind yourself of the layers of the eyelid inferior to the tarsal plate (see Figure 2-28). Starting at a point below the tarsus from anterior to posterior, the layers of the eyelid are:
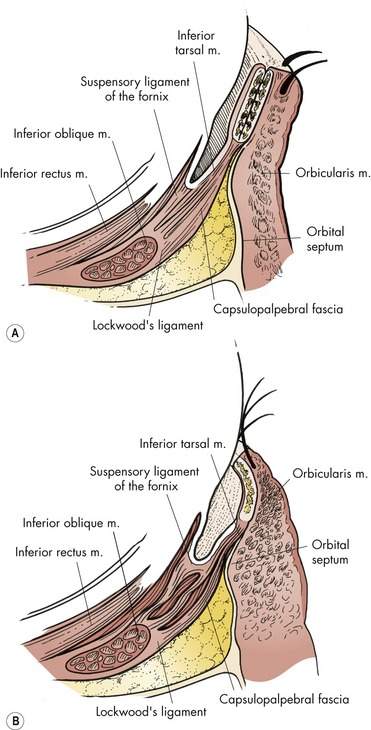
Several factors contribute to the stability of the lid. In general, a tight lower eyelid, without horizontal lid laxity, is a stable lid. Laxity predisposes the lower lid to either ectropion or entropion, as we have seen in Chapter 3. Think about what the lower eyelid retractors do. As the eye looks down, the lower lid retractors pull the lower eyelid downward. If the retractors did not work in synchrony with the eyeball, the eyelid would block the pupil in downgaze. This synchronous movement results from the connection of the capsulopalpebral fascia portion of the lower eyelid retractors with the inferior rectus muscle.
The lower eyelid retractors also help to keep the eyelid margin in normal position. The retractors pull the lower margin of the tarsus inferiorly and posteriorly, in the direction of the pull of the inferior rectus muscle. This keeps the lower edge of the tarsal plate “tucked in” against the eye with the eyelid margin in the normal position. Normal tension on the lower eyelid retractors is essential for maintaining a stable eyelid and preventing entropion (Box 4-3).
Box 4-3 Factors Contributing to the Stability of the Lower Eyelid
• Appropriate horizontal tension of the lower lid so that the eyelid is apposed to the eyeball
• Lower lid retractors applying appropriate tension to the inferior margin of the tarsus, pulling the lower edge of the tarsus inferiorly and posteriorly and thus preventing the lid margin from turning inward toward the eye
• Synchronous movement of the inferior rectus and lower lid retractors so that the eyelid moves downward as the eye travels in downgaze
• Balance between the anterior and posterior lamellar tension
Involutional entropion
Laxity of the lower lid retractors is the primary cause of involutional entropion (Figure 4-2). Lower lid horizontal laxity is usually present, making the lid unstable. Laxity of the lower lid retractors allows the inferior edge of the tarsus to rotate away from the eye. This allows the lid margin to invert (Figure 4-3). In many cases, the preseptal orbicularis muscle actually seems to “push” the lower eyelid margin inward. Variations of Figure 4-2 are shown in all texts discussing entropion. Make sure that you understand this figure.
Spastic entropion
Spastic entropion occurs when the eyelids are held in a closed or “guarded” position. The sustained “squinting” of the lower lid is the initiating force for the entropion. The most common situation for this reflex blepharospasm is after surgery, usually an anterior segment trauma repair or an extensive posterior segment procedure. The spasm or squeezing of the lid seems to push the lid margin against the eye. This condition most often occurs in patients who have predisposing factors to involutional entropion, such as horizontal laxity and lax lower lid retractors. The retractors cannot hold the lid in normal position against the forceful “overriding orbicularis” pushing the lid margin inward.
Cicatricial entropion
Cicatricial entropion is caused by shortening of the posterior lamella, which pulls the eyelid margin inward (Figure 4-4). Cicatricial entropion is common throughout the world, especially where trachoma is endemic. Cicatricial entropion is less common than involutional entropion, but it is still seen in the United States. Any problem that causes scarring of the conjunctiva may cause a cicatricial entropion (Box 4-4). Common causes include:
• Ocular cicatricial pemphigoid (OCP)
• Surgical or accidental trauma
• Recurrent chalazia or blepharitis
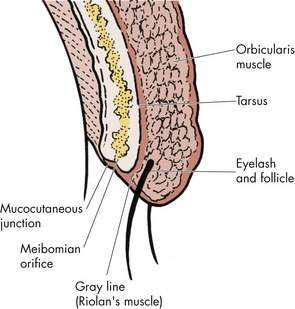
Figure 4-4 Cicatricial entropion. Note that the posterior lamellar shortening pulls the eyelid inward.
In most patients with cicatricial entropion, the conjunctival scarring is easy to see and the etiology is usually obvious (Figure 4-5). As I said earlier, all instances of upper lid entropion are cicatricial. There is no upper lid involutional entropion.
Marginal entropion
Patients with cicatricial entropion have eyelashes against the eye. The problem is classified as entropion, not trichiasis, because the eyelid margin is obviously inverted. Most patients diagnosed with “trichiasis” have a subtle form of cicatricial entropion known as marginal entropion
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree