CHAPTER 11 Diagnosis of Malignant and Benign Lid Lesions Made Easy*
Introduction
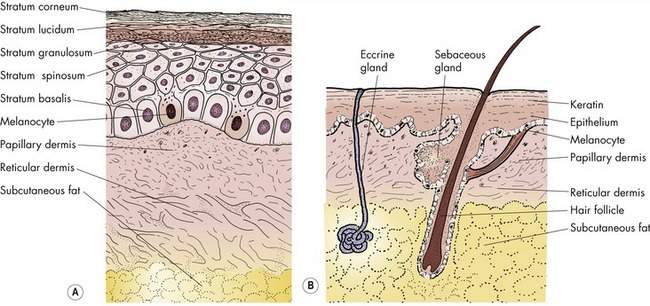
The skin has two layers, the epidermis and the dermis. Basal cell and squamous cell carcinomas arise from the epidermis. The dermis contains the skin appendages or adnexa (“added on”). The adnexae include hair follicles, oil (sebaceous) glands, and sweat glands. The most common adnexal malignancy is sebaceous cell carcinoma. This malignancy does not have a characteristic appearance. Sometimes a yellow pigmentation of sebaceous cell carcinoma may be noted. A chronic unilateral blepharoconjunctivitis or an eyelid margin lesion extending from the posterior lamella onto the skin should suggest a possible diagnosis of sebaceous cell carcinoma.
Skin anatomy
Layers of the skin
The eyelid skin is the thinnest skin in the body. This skin contains two layers:
The epidermis is the continually dividing superficial layer of the skin that covers the body. The dermis is the deep layer of the skin. Other than in the eyelid, there is a layer of subcutaneous fat deep to the dermis (Figure 11-1). The eyelid skin is tightly bound to the underlying orbicularis muscle.
Appendages of the skin
The dermis contains the skin appendages or adnexa (Figure 11-1). The adnexa are the specialized tissues added on to the skin including:
Each adnexal tissue contains specialized cells that may create both solid or cystic cell proliferations. Common tumors arising from the adnexa include chalazia and various cysts. Chalazia arise from the specialized sebaceous glands of the tarsal plate, the meibomian glands. The most common cyst in the periocular area, the apocrine hidrocystoma, arises from the apocrine sweat glands along the lid margin. We will talk about this later. For now, just remember that there can be solid and cystic tumors of each adnexal tissue.
The dermis also contains a number of other tissues including vascular, fibrous, and neural elements. Each of these tissues may give rise to tumors that are rarely seen in the eyelids. You are not likely to see many of these lesions so they will not be covered in this text (Box 11-1).
Malignant tumors of the epidermis
Characteristics of malignancy
This is the most important section of this chapter. Remember that the main goal of evaluating a lid lesion is to rule out malignancy. The most common skin malignancy is basal cell carcinoma, which arises from the epidermis. Basal cell carcinoma represents more than 90% of lid malignancies. If you can recognize basal cell carcinoma, you will be able to recognize the majority of skin cancers affecting the eyelids. Review the characteristics of skin malignancy listed in Box 11-2. Remember these characteristics and you will have little difficulty in diagnosing cutaneous malignancies.
Box 11-2 Characteristics of Skin Malignancy
• Ulceration: Malignant lesions tend to ulcerate; benign lesions don’t
• Lack of tenderness: Malignant lesions are not painful or tender to touch
• Induration: Malignant lesions tend to be firm
• Irregularity: Malignant lesions have irregular borders and asymmetric shapes
• Loss of lid margin architecture: Malignancies tend to destroy normal anatomic features
• Telangiectasia: Focal telangiectasias on the periphery of a tumor suggest malignancy
• Pearly borders: Rolled translucent margins that are whitish in appearance are characteristic of basal cell carcinoma
Pearly borders and telangiectasia
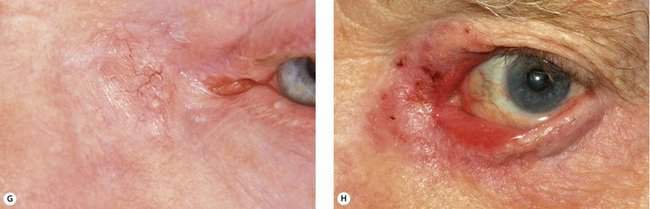
Pearly borders and telangiectasias are pathognomonic for basal cell carcinoma. Heaped up edges often surround an area of central ulceration. With the slit beam focused on the edge of these lesions, there appears to be a translucency to the lesion itself allegedly from the proliferating cells in the basal layer of the epidermis. Telangiectasias refer to the dilated and irregular vessels accompanying the pearly margins of the basal cell carcinoma. Review the photographs of typical basal cell carcinomas and make sure in your mind that you recognize all the features of epithelial cell malignancy (Figure 11-2).
Loss of eyelid margin architecture
Remember, the goal is to diagnose malignancy. When your diagnostic skills become more sophisticated, you may be able to tell the type of skin cancer based on the location and how the lesion affects the lid margin. Study the skin carefully during the slit lamp examination. Use the slit lamp as the equivalent of the gynecologist’s colposcope used to diagnose potential malignancies of the cervix. Remember that squamous cell carcinoma tends to be the most superficial of skin cancers initially, and often only scaling is seen in its early phases. Basal cell carcinoma begins a little deeper with rolled edges at the periphery “pulling” normal skin into the lesion. You will not see keratinization on the examination. Because basal cell and squamous cell carcinomas are epithelial lesions, they affect the anterior lamella initially. Sebaceous cell carcinoma affects the posterior lamella first in most patients. Look at the area of distortion or destruction of the lid margin for these clues to the type of malignancy. Don’t lose sight of the goal: learning to differentiate malignant from benign lesions first.
Basal cell carcinoma
Basal cell carcinoma and squamous cell carcinoma may be recognized by the company that they keep. Other signs of actinic damage to the skin, especially in a patient with light skin and blue eyes, should heighten your suspicion of a skin malignancy. Look for signs of sun damage on your patient’s face to help you diagnose basal cell carcinoma (Figure 11-3).
Squamous cell carcinoma
Squamous cell carcinoma can appear as a nodule or an indurated plaque with some hyperkeratosis. Often the scaly skin will fall off—strongly suggesting a squamous cell cancer or its precursor, actinic keratosis (discussed later in this chapter). Ulceration is sometimes present. Generally, the pearly margins and telangiectasia of basal cell carcinoma are not seen.
Squamous cell carcinoma is usually more aggressive than basal cell carcinoma. The margins of squamous cell carcinoma may be diffuse, resulting in a large area of subclinical tumor involvement (Figure 11-4). Neurotrophic spread (along nerves) occurs in squamous cell carcinoma but is uncommon in basal cell carcinoma. Squamous cell carcinoma in the periocular area with the presence of cranial nerve palsy suggests neurotrophic spread into the cavernous sinus.
Like basal cell carcinoma, squamous cell carcinoma arises in sun-damaged skin. The features of cutaneous actinic damage, such as deep wrinkles, skin thinning, generalized telangiectasia, and mottled pigmentation, may be seen (see Figure 11-19). Scaling keratotic lesions, actinic keratoses, the precursors of squamous cell carcinoma, are often present.
Malignant tumors of the adnexa: sebaceous cell carcinoma
Sebaceous glands in the periocular area
• Meibomian glands located within the tarsal plates
• Glands of Zeis associated with the eyelash follicles
• Sebaceous glands of the periocular skin
• Sebaceous glands in the caruncle
Clinical characteristics
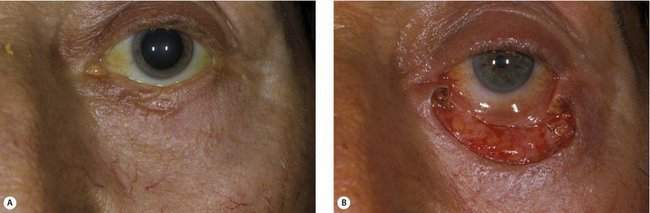
Sebaceous cell carcinoma has no characteristic appearance; consequently, it is known as a “masquerader.” You won’t see many sebaceous cell cancers, but be suspicious if you see a unilateral blepharoconjunctivitis or a chronic or recurrent chalazion. In my experience, the classic recurrent chalazion is the more unusual presentation. An inflamed or swollen lid with conjunctivitis is more common. This blepharoconjunctivitis may present as a chronic condition (Figure 11-5). In some patients, many medical or surgical treatments will have been tried without relief, and the diagnosis of sebaceous cell carcinoma will not have been considered. Biopsy should be performed for chronic unilateral blepharoconjunctivitis or recurrent chalazia. In some cases, the conjunctival spread will predominate, so don’t forget to evert the eyelid. In other patients, sebaceous cell carcinoma may present as a more subtle thickening of the lid and lid margin (Figure 11-6). You should consider the diagnosis if you see a lid margin lesion that appears to arise from or extend over the margin onto the tarsal conjunctiva. The presence of any yellowish material within a malignant-appearing lesion should suggest the diagnosis of sebaceous cell carcinoma.

Figure 11-5 Sebaceous cell carcinoma presenting as an advanced unilateral chronic blepharoconjunctivitis.
Tumor excision
Sebaceous cell carcinoma is an uncommon tumor. It is difficult to diagnose because of its many manifestations. It is difficult to excise because of pagetoid spread and noncontiguous tumor origins. Unlike with basal cell carcinoma and squamous cell carcinoma, there is a possibility of regional lymph node metastasis (Figure 11-7). In most patients, no regional disease is present at the time of diagnosis. Fortunately, local resection is usually curative. If all four lids are involved or orbital fat is invaded, orbital exenteration is required. Death caused by sebaceous cell carcinoma is possible, but rare.
Checkpoint
• At this point in this chapter, you should be able to diagnose the majority of malignant lid lesions you will encounter in practice
• The diagnosis of most cutaneous malignancies is based upon recognition of the clinical characteristics of malignancy that will help you identify basal cell carcinoma and squamous cell carcinoma
• Important! What are the clinical characteristics of skin malignancy?
• What growth characteristics make sebaceous cell carcinoma difficult to resect?
• Chronic unilateral conjunctivitis or a “chalazion” resistant to treatment should alert you to the possible diagnosis of sebaceous cell carcinoma
Pigmented lesions: ruling out melanoma
General concepts
Although eyelid melanomas are rare, we are all concerned about the possibility of a pigmented lesion being a melanoma. This section will help you to differentiate benign from malignant pigmented lesions of the skin. Let’s start with these basic concepts (Box 11-3).