Surgical Correction of Pediatric Midface Fractures
Eric Lowry Cole
Shelby R. Lies
DEFINITION
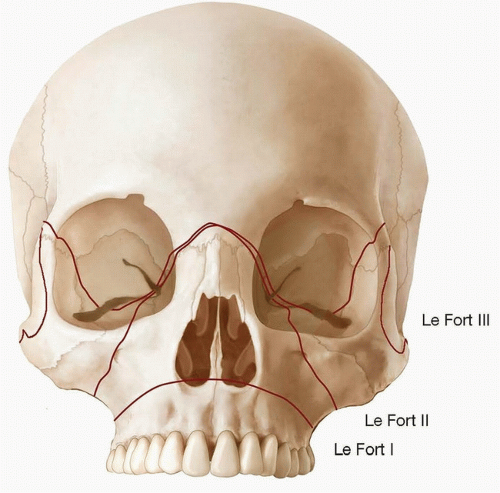
Le Fort fracture
Le Fort I dentoalveolar separation including pterygoid plates
Le Fort II bilateral pyramidal fracture including pterygoid plates
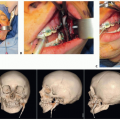
Le Fort III craniofacial separation involving the frontonasal articulation, traversing the orbital walls with disjunction of pterygoid plates and zygomatic arch (FIG 1)
Nasal bone fracture
Naso-orbitoethmoid fracture
Zygomaticomaxillary complex fracture
Frontal bone fracture
ANATOMY
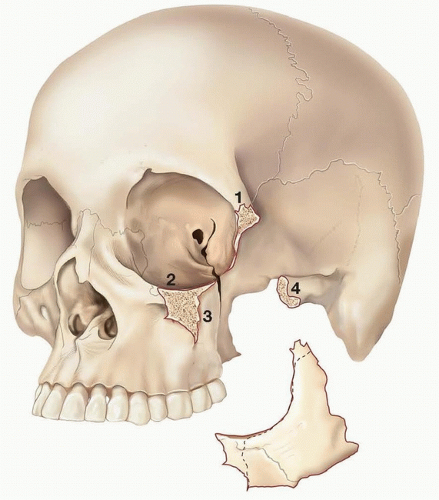
The zygoma articulates with the frontal bone, maxilla, temporal bone, and sphenoid. All fractures of the zygoma affect the orbital floor or lateral orbital wall.
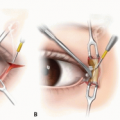
The zygomaticosphenoid junction is the key anatomical articulation in the reduction of these fractures (FIG 2).
Naso-orbitoethmoid (NOE) fractures are defined as a comminuted fracture of the nose and orbit involving the medial orbital walls, ethmoid sinus, and bony and cartilaginous structures of the nose.
PATHOGENESIS
Motor vehicle collisions and assault are the most common causes of facial fractures in children.1
Consider possible nonaccidental injury if the history does not match the injury or if there are multiple emergency room visits.
The prominent cranium and mandible in children make isolated midface fractures uncommon, and their presence should prompt a search for associated intracranial and cervical spine injuries.2
Pure Le Fort fractures are rare and oblique hemi-Le Fort patterns are more common in children.
Relative underdevelopment of the maxillary sinus allows the zygomaticomaxillary buttress to resist classic Le Fort I level fractures, and instead, force is transferred to dentoalveolar segments causing alveolar and dental injuries.
Le Fort II and Le Fort III level injuries often present with NOE fractures combined with zygomaticomaxillary complex and orbital wall fractures.
PATIENT HISTORY AND PHYSICAL FINDINGS
Blunt trauma causes fractures at articulations.
Direct impact to the lateral face may cause an isolated depressed zygomatic arch fracture.
Significant medial displacement may result in the loss of lateral facial width or trismus through impingement on the coronoid.
Higher-velocity injuries often cause comminution and deformity in facial width, orbital rim step-offs, flattening of malar prominence, and globe malposition.
Assess facial symmetry and occlusion; palpate to determine integrity of frontal bones, orbital rims, and malar eminence of zygomatic arch.
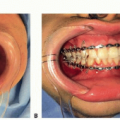
Check stability of the maxilla including dentoalveolar segments by stabilizing the head and attempting to mobilize the dentition. Ecchymosis may be present in the gingivobuccal sulcus.
Visual acuity and globe integrity must be documented. Examine extraocular movement and pupillary response.
Enophthalmos. Lateral and/or inferior displacement of the zygoma may increase orbital volume and lead to enophthalmos. Greater than 3 mm change in globe position compared to contralateral eye appears clinically significant. Relation of the corneal surface to the lateral orbital wall can be measured with a Hertel exophthalmometer device.
Diplopia. Symptoms occur mostly in upward gauze due to hypotropia where the focus is on the eye with a visual axis lower than the contralateral fixating eye, most commonly with injury to the inferior rectus muscle.
Traumatic optic neuropathy can present with subtle findings of diminished color perception. Consult an ophthalmologist.
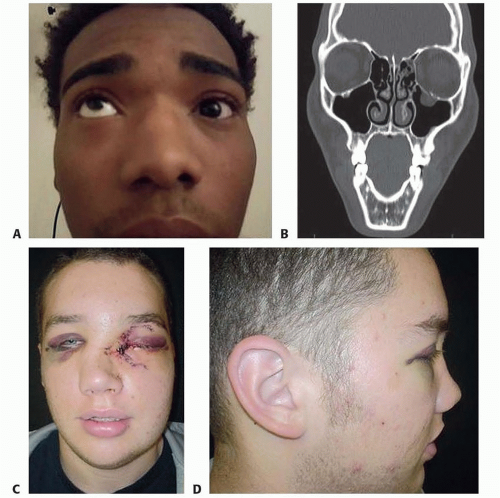
Oculocardiac reflex involves classic triad of bradycardia, nausea, and syncope. If symptoms occur in any phase of treatment, suspect periorbital entrapment, which necessitates release. Pediatric patients are more prone to sustain a trapdoor deformity of the orbital floor, leading to entrapment and persistent nausea (FIG 3A,B).
Cheek numbness as a result of infraorbital nerve injury.
NOE fracture deformity includes loss of nasal bridge projection, upturned nose, and telescoping nasal length (FIG 3C,D).
The varying degree of loss of canthal attachment creates an increase in intercanthal distance with blunting of the palpebral fissures. A bowstring test can assess for tendon avulsion.
Intranasal speculum examination for epistaxis and septal hematoma
Rule out CSF leak with a tilt test for halo sign and/or betatransferrin analysis.
IMAGING
Plain occipitomental views demonstrate distraction of articulations and zygomatic arch anatomy.
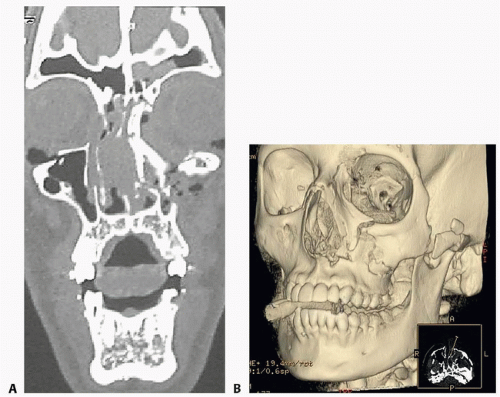
Computed tomography (CT) max-face is the diagnostic study of choice to evaluate the characteristics of fracture patterns. Considerable information can be obtained from CT imaging.
Manson’s classification according to degree of displacement/comminution is useful based on CT3:
Minimal displacement, no comminution
Moderate displacement, mild comminution
Severe displacement, major buttresses comminuted in multiple locations
Three dimensional (3D) reconstruction offers interpretation of complex fractures (FIG 4).
DIFFERENTIAL DIAGNOSIS
Skull fractures from frontal impact are more common in young children, and older teens have a higher probability of facial fractures.2
Intracranial abnormalities
Cervical spine injury
Nasal bone
Mandible, particularly the subcondylar region
Frontonasoethmoid region
Orbit, most frequently involving the orbital roof in children under 7, as compared to the floor in adults
NONOPERATIVE MANAGEMENT
In the pediatric patient, rigid skeletal fixation can do more harm than good. Children have significant capability of bony remodeling and dental compensation.
Fractures should be managed conservatively whenever possible.
Nondisplaced and minimally displaced fractures, in the absence of orbital dysmorphology or malocclusion, may be treated with nonoperative care.
Close follow-up and a soft diet for 4 weeks are recommended.
Bone fragment displacement can be caused by muscles of mastication; therefore, parents should be advised to provide appropriately “mushy” meals that can be squeezed between the fingers and instruct children to avoid force while eating.
SURGICAL MANAGEMENT
Many of the same principles in the treatment of adult midface fractures apply to children.
Notable exceptions include the avoidance of implants in tooth-bearing areas to prevent damage to tooth buds and the use of resorbable plates.
Resorbable plating systems composed of polylactic and polyglycolic acids are readily available and preferred when possible.
The plates are usually resorbed within a year and are of adequate strength for fixation of thin bones.4
The goals of reconstruction include obtaining pretraumatic occlusion along with re-establishing the buttresses (medial nasomaxillary and lateral zygomaticomaxillary) to restore the width and projection of the midface.
The indications for surgical treatment of fractures include malocclusion, trismus, and significant displacement causing enophthalmos or a noticeable contour deformity.
Treatment involves open reduction and fixation with miniplates, preferably resorbable.
Le Fort I displaced fractures require MMF and ORIF of the medial nasomaxillary and lateral zygomaticomaxillary buttresses.
Le Fort II fractures are often unilateral (hemi) and can present with NOE fractures. Treatment of displaced fractures requires fixation of the medial and lateral buttresses and the orbital rim. A coronal incision may be necessary to address the nasofrontal region.
NOE fractures are particularly difficult to manage in children.
Complete avulsion of the medial canthal tendon is the strongest indication for surgery.
Avulsion of the canthal tendon is best managed with open transnasal canthoplasty.
Cantilever bone graft should also be considered during primary reconstruction.
Le Fort III fractures are often unilateral with multiple fragments and present with NOE combined with zygomaticomaxillary complex fractures.
Synchronous ORIF of each subunit fracture through existing lacerations, a coronal approach, or a glabellar incision.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree