CHAPTER 21 Superolateral Pedicle Breast Reduction with Vertical and Inverted T Patterns
Key Points
Patient Selection
The superolateral dermoparenchymal pedicle has been adapted for surgery on a myriad of breast types using differing skin excisions. A simple classification system that reflects the versatility of the superolateral pedicle operation has been developed and is used to select appropriate patients for this technique.1
Type I: Superolateral dermoparenchymal pedicle using the modified Wise pattern:2
Type II: Superolateral dermoparenchymal pedicle using the vertical pattern:
Indications
The evolution of procedures designed to reduce breast volume and improve breast shape has been an ongoing process since the first reports by the Greek physician, Paulus Aegineta, probably during the seventh century ce (sixth book of the Synopsis of Medicine in Seven Books). Since that time, almost every conceivable pedicle type, both dermal and parenchymal, has been successfully employed. This flexibility in pedicle selection is afforded by the rich blood supply network to the breast, which includes the internal mammary artery, lateral thoracic artery, multiple intercostal perforators, thoracoacromial artery, and thoracodorsal artery. As Aufricht stated: ‘There is sufficient blood supply from any direction of the breast hemisphere to nourish the corresponding tissue.3
The anatomic innervation to the breast has been described by several authors. A detailed description of the anatomy was provided by Sir Astley Cooper in 1840.4 Craig and Sykes5 have elucidated the importance of the third, fourth, and fifth anterior cutaneous nerves, and the fourth and fifth lateral cutaneous nerves, in supplying sensation to the nipple–areola complex. Courtiss and Goldwyn6 identified the lateral cutaneous branch of the fourth intercostal nerve as the major source of innervation to the nipple–areola complex. Attempts at preserving maximal nipple–areola sensation during breast surgery must take these anatomic features into account.
The superolateral dermoparenchymal pedicle technique integrates elements from several other operations. Strombeck7 developed a horizontal bipedicled dermoparenchymal flap for breast reduction in 1960. Skoog8 is credited with describing the first lateral pedicle, modifying the Strombeck procedure by elevating the nipple–areola complex on a lateral dermal pedicle alone. In 1982, Nicolle9 presented his experience with the lateral dermoparenchymal pedicle for breast reduction. Cardenas-Camerana and Vergara10 described their successful use of the superolateral dermoglandular pedicle.
The superolateral dermoparenchymal pedicle has been successfully employed by the authors in over 1500 breast operations, including reduction mammaplasty and mastopexy procedures, using differing patterns of skin excisions. For many years the procedure was performed using a modified Wise pattern only, for skin excision. During the past 7 years, following the presentations of Lassus,11 Lejour and Abboud,12 and especially Hall-Findlay,13 a vertical pattern of skin and breast excision has been offered to patients. Follow-up for some patients has been for 15 years (Figs 21.13 and 21.14). Routinely, patients are followed for a minimum of 5 years.
Operative Techniques
Wise pattern procedure (types Ia (Fig. 21.1), Ib (Fig. 21.2), Ic (Fig. 21.3))
Markings
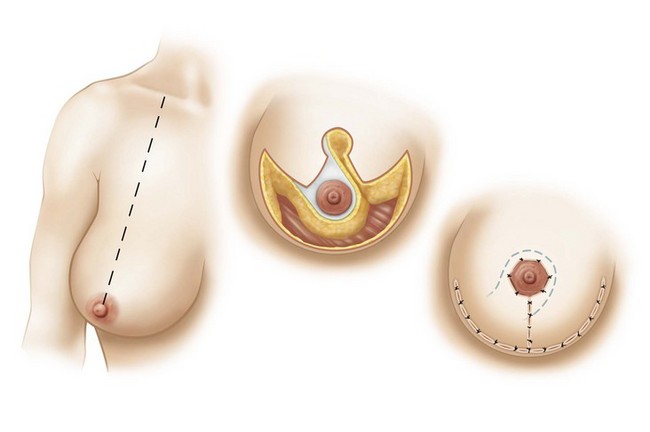
Fig. 21.1 Wise-type pattern variation (Ia).
With permission from Strauch B, Elkowitz M, Baum T, Herman C. Superolateral pedicle for breast surgery: an operation for all reasons. Plast Reconstr Surg 2005;115(5):1269–77; discussion 1278–9.
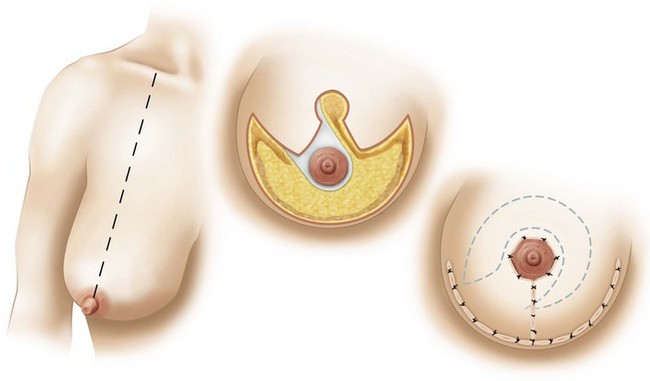
Fig. 21.2 Wise-type variation (Ib).
Wise-type pattern resection with SLDP for mastopexy for correction of ptosis.
With permission from Strauch B, Elkowitz M, Baum T, Herman C. Superolateral pedicle for breast surgery: an operation for all reasons. Plast Reconstr Surg 2005;115(5):1269–77; discussion 1278–9.
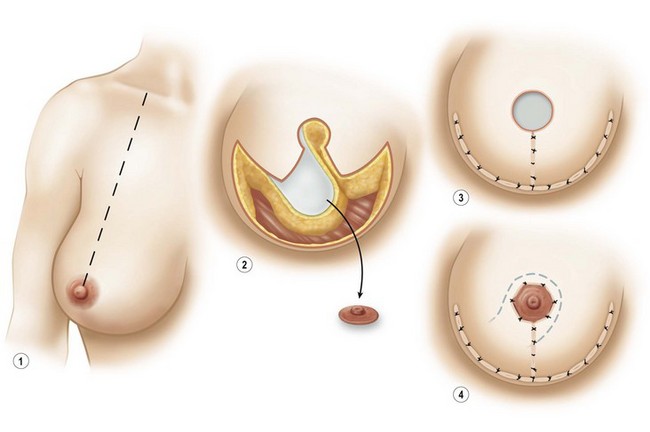
Fig. 21.3 Wise-type variation (Ic).
With permission from Strauch B, Elkowitz M, Baum T, Herman C. Superolateral pedicle for breast surgery: an operation for all reasons. Plast Reconstr Surg 2005;115(5):1269–77; discussion 1278–9.









