CHAPTER 25 Subfascial Breast Augmentation
Summary/Key Points
According to the most accurate statistic databases all around the world, the number of breast augmentation procedures has been increasing over the years.1,2 The surgical approach, implant selection, and especially implant plane or pocket plane have been subjects of controversy. This chapter will discuss different approaches used to insert a breast implant subfascially, including anatomical considerations, patient selection and indications, operative techniques, advantages, pitfalls and postoperative care.
Anatomical Considerations
The breast is essentially a skin appendage contained within layers of the superficial fascia. The superficial layer of this fascia is near the dermis and is not distinct from it. The deep layer of the superficial fascia is more distinct and is identifiable when the breast is elevated in a subglandular augmentation mammaplasty.3 There is a loose areolar tissue between the deep layer of the superficial fascia and the fascia that covers the pectoralis major and continues to cover the adjacent rectus abdominis.4
The pectoral fascia is a dense connective tissue that originates from the clavicle and sternum and covers the pectoralis major muscle and continues to cover the adjacent rectus abdominis, serratus anterior, external oblique muscle and extends toward the lateral border of the pectoralis major muscle to form the axillary fascia, as we can see in Figure 25.1. At the caudal border of the pectoralis muscle, the clavipectoral, pectoral, and serratus anterior fasciae become continuous and form the suspensory ligaments that extend to the breast inframammary fold.5
The pectoral fascia can be bluntly dissected along the subfascial plane and it has some specific characteristics. At the level of the second rib, the pectoral fascia tightly connects with the superficial fascia of the breast and it is difficult to dissect bluntly. Along the point that corresponds to the fourth intercostal space, the horizontal septum originating from the pectoral fascia connects with the nipple. At the inframammary crease, a dense connective tissue is found connecting the skin crease and the pectoral fascia. Fascial thickness has been found to vary from 0.2 to 1.14 mm along its different portions. Perforating vessels and nerves emerge mainly from the medial, lateral and lower part of the fascia.6
Patient Selection and Indications
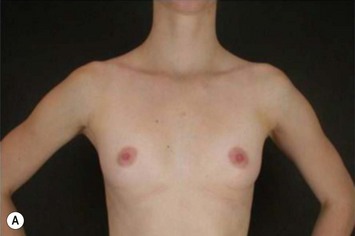
The pectoral fascia helps to support the implant and even in slim patients it gives a smoother transition in the upper pole of the breast, improving the final aesthetic result (Fig. 25.2).5,7,8 The exception would include thin patients who desire relatively large implants. In these patients it is better to use a round implant in the retromuscular pocket, or an anatomical/shaped implant subfascially (Fig. 25.3). Some other possible advantages clinically noticed with subfascial breast augmentation still need to be investigated. We have had the impression of reducing postoperative breast ptosis due to fascial support, and minimizing incidence of capsular contracture, possibly due to contact of the muscle fibers with the implant.
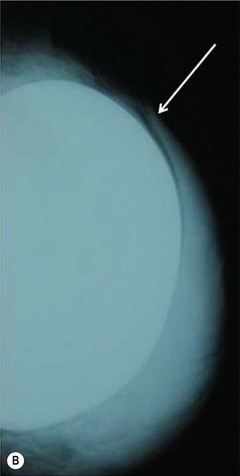
Transaxillary subfascial breast augmentation can be indicated for every patient who does not need mastopexy. Augmenting the breasts without leaving a scar on them is the major advantage in this technique and has been frequently desired by young patients (Fig. 25.4). The fact of creating a scar in a low tension area, far from the breasts, makes this approach the preferred technique in patients with known history or risk factors for hypertrophic scars and keloid. Preoperative conversation regarding axillary lymphatic drainage of the breasts and sentinel node implications is advisable. Recent studies published by our group showed that the sentinel node in the axilla can be preserved after transaxillary breast augmentation if some technical details during dissection are respected.9,10 This technique requires special instruments (long lighted retractors or video-endoscopic apparatus) and has a longer learning curve. Any kind of implant can be used through this access, however special attention should be given to avoid misplacement of anatomical implants.
The periareolar approach can be indicated for patients with medium or large size areolae, since the lower half perimeter of the areola must allow an incision of at least 4 cm. A well defined transition between areola and breast skin is also important to have a less visible scar. Patients who have breasts with mild ptosis that will probably not be corrected by the breast implant chosen are good candidates for a periareolar mastopexy (Fig. 25.5). Patients with tuberous breasts usually present with lower pole hypoplasia and some degree of nipple–areola complex weakness and prolapse. In these cases we have also used the circumareolar approach with nylon round-block suture to improve nipple–areola complex herniation. The subfascial pocket is created, but the fascia is radially incised in the lower breast in order to allow more skin distention. Round implants can be used for mild tuberous breasts, however in more severe cases anatomical shaped implants are better indicated to obtain greater lower pole projection.
The inframammary breast augmentation is the simplest and most direct access to insert silicone gel implants. It is not limited by the size of the implant, because the incision can be extended if necessary. It is also the most conservative approach relative to disturbing the breast parenchyma and preserving lymphatic drainage. The scars are usually of good quality and hidden under the brassiere (Fig. 25.6E). Correct planning of the incision is important to leave the final scar positioned right in the new inframammary fold. This approach can be indicated for every patient who is not a candidate for periareolar mastopexy, and for those patients with a previous history of hypertrophic scar or keloid. Disadvantages include a visible scar when the patient is lying down, greater risk of implant exposure compared to other approaches, and higher incidence of Mondor’s syndrome.11
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree