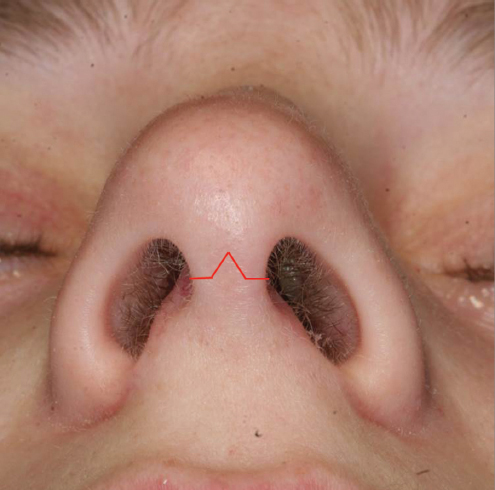
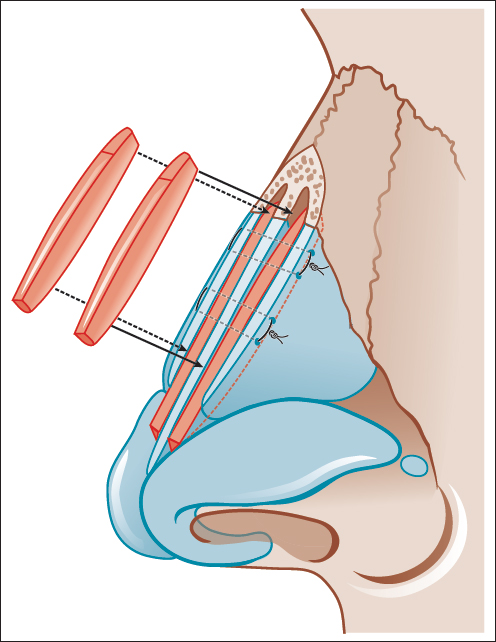
Chapter 7 Rhinoplasty is consistently ranked in the top five cosmetic surgical procedures performed annually in the United States. The primary objective of rhinoplasty is to create predictable changes in nasal contour while maximizing nasal function. Reproducible, consistent outcomes in rhinoplasty come with the surgeon’s ability to create a stable nasal structure and predict the effects of scar contracture on this structure over time. In complex cases, endonasal approaches may not provide the exposure needed to execute complex grafting. The external approach allows maximal exposure of the cartilaginous nasal structures, bony vault, and septum. The surgeon is thus able to directly visualize the repositioning, alteration, and augmentation of the nasal structures. Joseph and Gillies both reported cases using an open approach to rhinoplasty in the early part of the 20th century. Over the ensuing decades, the technique evolved to include a transcolumellar incision that extended onto the vestibular skin, allowing for wider exposure. In North America, the approach has gained in popularity since its introduction by Padovan in 1970. Early criticism of the visible columellar scar has been addressed by numerous reports of favorable results with scar camouflage. One must remember that external rhinoplasty is only a means to access the underlying nasal structures. Once exposure is achieved, there are a multitude of maneuvers that may be executed depending on the patient’s individual anatomy. A description of the external approach itself and the maneuvers commonly performed during structural rhinoplasty is presented in the following. While there are no absolute indications to external rhinoplasty, there are certain problems that are best corrected through techniques requiring wide exposure. In general, these methods involve extensive rearrangement of existing structures or addition of structural grafts. Indications include the following: 1. Significant tip deformity with an asymmetric, ptotic, over-projected/underprojected, bulbous, or buckled tip structure. 2. Secondary rhinoplasty—previously disrupted structural supports may need to be reconstituted or replaced. 3. Non-Caucasian rhinoplasty—may require significant increases in projection and support of inherently weak alar cartilages. 4. Cleft lip nasal deformity. 5. Crooked nose—may require precise repositioning of upper lateral cartilage (ULC) or lower lateral cartilage (LLC) or extensive septal correction or reconstruction. 6. Major nasal reconstruction. 7. diagnosis—in the cases in which the surgeon is uncertain as to the anatomical cause of the deformity, the external approach allows for accurate diagnosis prior to structural modification. A relative contraindication to the external approach for rhinoplasty is the presence of severely damaged or thinned skin. Such conditions may occur following multiple previous operations, particularly in thin-skinned individuals. The presence of acquired cutaneous telangiectasias, purple or blue discoloration of the nasal skin with cold temperature, and visible irregularities are signs of such a condition. In these cases, an endonasal approach with limited soft-tissue elevation may reduce the risk of further cutaneous compromise. Although there are no absolute contraindications to the external approach during rhinoplasty, an endonasal approach may be a reasonable alternative in the cases in which minimal changes are required. Nondelivery approaches have the advantage of preserving all major tip support mechanisms of the nose. Access may be gained through a cartilage-splitting or retrograde approach. The main disadvantage of these approaches is the limited exposure of the tip cartilages. While the delivery approach provides greater exposure than nondelivery approaches, it does so at the cost of potentially compromising tip support. Specifically, the intercartilaginous incision disrupts the attachment of the ULCs and LLCS. Although the lower lateral crura are widely exposed with this method, the chondrocutaneous flap is delivered in a nonanatomical orientation, creating potential difficulty for the inexperienced surgeon. In all rhinoplasty, a clear understanding must be reached between surgeon and patient regarding the perceived nasal deformities, surgical plan, and expected outcomes. The relationship between nasal airway function and appearance must be emphasized. It is imperative that the patient understand that the postoperative period is a prolonged and dynamic process. Initially, the patient must anticipate a significant amount of swelling which will slowly subside. Over the ensuing months and years, ongoing resolution of edema and contraction of the soft-tissue envelope will create more definition to the nose. The patient must therefore be prepared to wait for several months for a significant improvement from surgery. This is especially true for thick-skinned individuals, revision patients requiring extensive manipulations, or patients with only subtle problems. The patient should be aware that the incision on the columella will be visible for several weeks and will fade with time. Photographic documentation is essential before and after surgery. Full face frontal, oblique, lateral images, close-up base views, and smiling views are essential. Images should be obtained with dual flash sources angled 45 degrees toward the patient. An additional frontal view taken with a single flash placed in front of and above the patient allows for shadowing that highlights the dorsal line. A blue screen or wall is ideal for establishing contrast between the patient and the background. Photography views include the following: • Full face (expressionless) frontal, three-fourths, and lateral views, as well as (smiling) frontal and lateral views. • Close-up views of nose (brow to philtrum) from frontal, three-fourths, lateral, and base views. • Brow to mentum frontal view expressionless and smiling. This is especially important in ethnic rhinoplasty as some patients will request cosmetic enhancements that preserve their unique ethnic characteristics, while others seek a more westernized Caucasian standard. A consensus can be quickly reached with the visual aid that the computer image modification provides. A NOSE questionnaire is used to ascertain a subjective preoperative nasal obstruction score.1 A rhinoplasty preference sheet is used to subjectively obtain aesthetic goals related to the morphed images for intraoperative reference. The patient should be advised to stop all blood thinning agents such as aspirin, ibuprofen, and vitamin E for at least 2 weeks prior to surgery. The individual should be in relatively good health and free of active nasal infection at the time of surgery. Any concerning medical condition should be cleared by the patient’s primary care physician or appropriate consulting specialist. It is our preference to perform the operation under general anesthetic in order to protect the airway from dependent blood drainage. A single dose of intravenous cephalexin is given prior to the start of the case. If ear or costal cartilage is to be harvested, an antipseudomonal agent such as ciprofloxacin is administered. A standard rhinoplasty set should be available. The following is a list of essential instruments—the preference of the senior author is indicated in italics: • #11 and #15 blade scalpels. • Assorted fine skin hooks. • Fine dissecting scissors —Converse. • Fine needle holders—Webster and Castroviejo. • Fine forceps—Toothed Adson and Bishop-Harmen. • Tissue forceps —Brown-Adson. • Freer elevator. • Retractors—Converse. • Suture—5.0 and 6.0 polydioxanone suture (PDS) for stabilization of cartilaginous grafts; 5.0 clear nylon for permanent suture for modification to the shape of native cartilage; 4.0 plain gut on a straight septal needle (SC-1) for closure of septal flaps; 5.0 chromic for closure of vestibular skin incisions; 6.0 PDS for subcutaneous closure of columellar incision; and 7.0 nylon for columellar skin closure interspersed with 6.0 fast absorbing gut. The surgeon must note the thickness and sebaceous quality of the nasal skin–soft-tissue envelope (SSTE). In darker skinned individuals with thick skin, incisions may take longer to heal with increased potential for a visible scar. In addition, the underlying structural framework of the nose must push into the thick soft-tissue envelope in order for form to project through. Moreover, a significant tissue void in such patients will result in exuberant scar formation and poor definition, particularly in the tip and supratip areas. Thus, the postoperative soft-tissue pollybeak may be prevented by avoiding overreduction of the structural framework of the thick-skinned nose and opting instead to achieve balance by augmentation to areas of relative deficiency (Fig. 7.1). In thin-skinned patients, there is more tolerance for leaving a small amount of dead space as a greater degree of soft-tissue contracture will allow for “truer” redraping. This advantage in thin-skinned noses is counterbalanced by the added risk of contour irregularities becoming visible or palpable over time. Care must therefore be taken in ensuring that all existing bony and cartilaginous structures, grafts, and implants are precisely positioned and smoothly contoured.2 It is crucial to obtain a clear idea of the patient’s nasal airflow. Many patients present to the rhinoplasty surgeon with functional complaints, while others display variant anatomy that predisposes to postsurgical obstruction. Assessment should be undertaken prior to and after decongestion in order to differentiate between inflammatory and anatomical causes of obstruction. The surgeon must note the external stigmata of an obstructed nose or one that is prone to develop postoperative problems. These characteristics include thin SSTE, a narrow middle vault, short nasal bones, supra-alar pinching, narrow nasal base, a prominent supra-alar crease, narrow nostrils, and thin lateral nasal walls. Intranasal exam may reveal a narrow internal valve angle, dynamic lateral wall collapse, septal deviation, and inferior turbinate hypertrophy.3 All of these factors must be considered in formulating a surgical plan that will preserve a functional airway. Fig. 7.1 Treatment and prevention of pollybeak deformity in patients with thick skin requires primarily augmenting areas of deficiency. Augmenting a low nasal dorsum and increasing nasal tip projection are effective means of correcting a pollybeak deformity. Blue area indicates adding structure, red area indicates removing scar tissue, and yellow area indicates adding dorsal graft. Analysis should then continue with a systematic assessment of each view of the nose. While analysis of the patient is done in the office setting, quality preoperative photographs allow for more detailed study at a later time. On the frontal view, symmetry and width should be assessed in each of the vertical thirds of the nose. The brow-tip aesthetic lines should follow a gentle, unbroken curve following the relative normal variation of nasal width: slightly wider cephalad at the brows nasal root transition, narrower in the middle vault, and wider again at the tip. If the brow-tip aesthetic lines are irregular or asymmetrical, the anatomical cause of the problem should be noted. Bony and cartilaginous vault irregularities are easily discernable with a single light source placed above the patient to enhance shadowing. The general tip shape should be determined from the frontal and base views (e.g., bulbous, deviated, wide, amorphous, asymmetrical). The base view also provides information about the shape and size of the columella, alar base, nostrils, and lobule. In general, the frontal and base views should reveal a triangular shape of the nose in which the nasal base (interface of nose and face) is wider than the tip and dorsal line. The triangularity of the tip depends on the presence of an unbroken line from the nasal tip-defining points to the lateral alar margin.4 Poor structural support in this area will manifest as alar pinching or concavity of the alar margins on frontal and base views. In cases of variant anatomy in which the base is excessively narrow or the tip is too wide, the correct relationship must be restored. On the lateral view, the nasofrontal angle should be approximately 120 degrees. This angle is measured at the nasal starting point and is determined by the height of the radix and the angle of the forehead. A deep nasofrontal angle creates an illusion of a shorter nose, independent of the actual vertical position of the nasal starting point. Conversely, a shallow angle creates an appearance of a longer nose. The dorsum is assessed for smoothness, convexity or concavity, and presence of a supratip break. In the lower third, the overall projection and rotation of the nasal tip must be assessed. Using Goode’s method, the nasal tip projection, as defined from the alar crease to the tip-defining point, should be just over half the length of the nose.5 The nasolabial angle should be between 90 and 95 degrees in men and between 95 and 105 degrees in women. This angle can be affected by variations in the size and shape of the upper lip and premaxillary bone. Therefore, the nasolabial angle does not always reflect the degree of tip rotation. The alar–columellar relationship and degree of infratip break should also be noted. In ethnic rhinoplasty, the relationships may be different from the traditional ones above. They frequently require increased tip projection and augmentation and may have weaker cartilage than Caucasians to begin with. Prior to injection, preoperative photos and measurements are made. These measurements and photos are repeated intraoperatively and postoperatively. They include nasolabial/nasoseptal angle, projection, subnasale and infratip length (medial canthus as reference point), dorsal nasal length (nasion to nasal tip), upper lip length, and base width and flare. This information allows for accurate manipulation, within 1 mm, of each parameter during rhinoplasty. Up to 10 mL of local anesthetic with 1:100,000 epinephrine is placed intranasally in the submucoperichondrial plane on both sides of the septum, nasal floor, and inferior turbinate if turbinate surgery is planned. This larger volume generally will not cause significant hemodynamic disturbances in a healthy patient. The anesthetic is useful in providing vasoconstriction and hydrodissection. The external nasal SSTE is infiltrated with a smaller volume in order to prevent distortion of the baseline shape. The areas injected include the columella, the intradomal area to the nasal spine, the tip and supratip, and the dorsum and side walls. It is useful to mark the salient anatomy and abnormalities with a pen prior to injection. The marginal incisions may be scored lightly with a 15 blade while everting the alar rims with a wide skin hook to provide direct visualization. The incision should be designed at the caudal margin of the lateral crura. The cephalic border of the nasal vibrissae is an inconstant landmark that may help in localizing the caudal edge of the lateral crura. Palpation of the cartilage with the back of the scalpel is a more reliable localizing technique. The transcolumellar incision is then made with an 11 blade at the level of the midcolumella in an inverted V orientation. The apex of the V should form an angle approaching 90 degrees (Fig. 7.2). Creating an overly acute angle will increase the chance of skin ischemia and breakdown at the apex. The incision should be connected to the columellar extension of the marginal incisions that follow the caudal margin of the medial crura and lie 2 to 3 mm posterior to the lateral border of the columella. Particularly in thin-skinned patients and in patients with prominent medial and intermediate crura, these incisions must be placed superficially in order to avoid cutting the underlying cartilage. Elevation of the soft-tissue envelope then proceeds cephalad toward the domes. Three-point retraction greatly aids in the development of the correct plane of dissection. A fine double-prong skin hook retracts the superior flap of the columella cephalically; another fine skin hook is placed at the undersurface of the dome in order to retract the intermediate crus and dome inferolaterally; and a third wide double-prong skin hook is placed at the alar rim margin to expose the marginal incision. Dissection is performed with Converse scissors in a plane immediately superficial to the perichondrium. The scissors should be slightly angled downward toward the cartilage and the plane developed using the tips of the scissors rather than through a spreading motion. As the dissection plane is developed cephalad, the vestibular skin is incised flush with the caudal border of the lateral crura. The second fine double-prong skin hook may be advanced laterally on the lateral crus as dissection continues cephalad and laterally. Dissection should be taken to the lateral 25% of the lateral crus in order to gain enough exposure for work in the upper two-thirds of the nose. Once both lateral crura are exposed, dissection may be continued cephalad over the middle vault. Dissection below the muscle is critical to avoid thinning the overlying skin–soft-tissue envelope. Dissection of the soft-tissue envelope over the upper third should be elevated in a subperiosteal plane. Starting at the rhinion, a Joseph elevator is used to incise the periosteum. Dissection proceeds cephalad in this plane. The size of the subperiosteal pocket depends on the planned surgical maneuvers. If significant reduction or rasping of the bony dorsum is needed, a wider area of dissection may be required. If placement of a radix graft is planned, a narrow pocket may be preferred over the radix for better positioning of the radix graft. The middle vault has significant functional and cosmetic implications for the nose. Functionally, the internal nasal valve area is partly dependent on the relationship of the ULC and the dorsal septum. Excessive narrowing of the angle between these structures will lead to obstruction at the internal valve. Previous surgery causing destabilization of this area will result in inferomedial collapse of the ULC into the airway. In particular, patients with short nasal bones and long ULCs are at risk of collapse. The width and symmetry of the front view of the nose depends on symmetrical reconstruction of the ULC and septum. Spreader grafts are long, rectangular cartilaginous grafts placed between the dorsal cartilaginous septum and ULC.6 These grafts are useful for correcting functional and cosmetic problems related to a narrow or asymmetrical middle vault. In addition, these grafts should be used in primary rhinoplasty to prevent middle vault collapse in high-risk patients such as those with shorter nasal bones and thin skin. In particular, when reduction of a cartilaginous dorsal hump leads to excision of the horizontal articulation of the dorsal septum and ULCs, spreader grafts will stabilize the middle vault and help restore appropriate horizontal width. The dimensions of spreader grafts will vary depending on specific needs and anatomy, but range from 10 to 30 mm in length, 3 to 5 mm in height, and 2 to 4 mm in thickness. More than one graft may be needed depending on available grafting material and the deformities. In general, the thicker aspect of the spreader graft is beveled and then positioned cephalad at the rhinion in order to create the normal appearance of slightly increased width in this area (Fig. 7.3). The grafts may be placed from a dorsal approach after the ULCs are freed from the septum. Mucoperichondrial flaps must first be elevated from the junction of the ULC and septum in order to prevent injury to the mucosal lining and subsequent cicatrix. Two 5.0 PDS mattress sutures placed through the ULC, spreaders, and septum should be used for stabilization. The caudal ULC should be pulled caudally during the suture stabilization in order to straighten any redundancy or curvature. The dorsal profile of the spreader grafts, ULC, and septum should be coplanar and smooth. In situ trimming of the grafts may be needed to ensure an even dorsal surface. An alternative method of placing spreader grafts is through a tight subperichondrial tunnel at the junction of the ULC and dorsal septum. In this method, elevation of the septal flaps during septoplasty must not include the dorsal aspect of the quadrilateral cartilage. A mucoperichondrial incision is made high on the septum just caudal to the junction of the ULC and septum. A narrow dissection instrument, such as a narrow Cottle elevator, is then used to create a long, tight pocket just beneath the dorsal junction between the ULC and septum. Snug placement of a spreader graft into this tunnel will cantilever the ULC away from the dorsal septum, effecting additional widening of the internal nasal valve, as compared to placing spreaders through an open dorsal approach. In the latter, the ULC is lateralized, but the absolute angle between the septum and ULC does not change. The precise pocket spreader graft placed under an intact connection between the ULC and dorsal septum creates a cantilever effect and lateralization and mild flaring of the ULC, leading to increased width and angulation (Fig. 7.4). This effect is achieved because of the bulk of the spreader graft placed below the intact connection between the dorsal margin of the septum and the ULC. This translates to additional airway improvement. This method should be considered in patients with severe obstruction referable to the internal valve where the middle nasal vault does not need to be opened (no dorsal hump reduction and not deviated). A drawback to this method is the additional width that is incurred. Careful patient selection is therefore required.
Structural Grafting via the External Rhinoplasty Approach
7 Structural Grafting via the External Rhinoplasty Approach
7.1 Introduction
7.2 Indications
7.3 Contraindications
7.4 Alternative Techniques
7.5 Preoperative Considerations
7.6 Special Surgical Requirements
7.7 Preoperative Analysis
7.8 Surgical Technique
7.8.1 Incisions: Nuances and Technique
Middle Nasal Vault
Plastic Surgery Key
Fastest Plastic Surgery & Dermatology Insight Engine