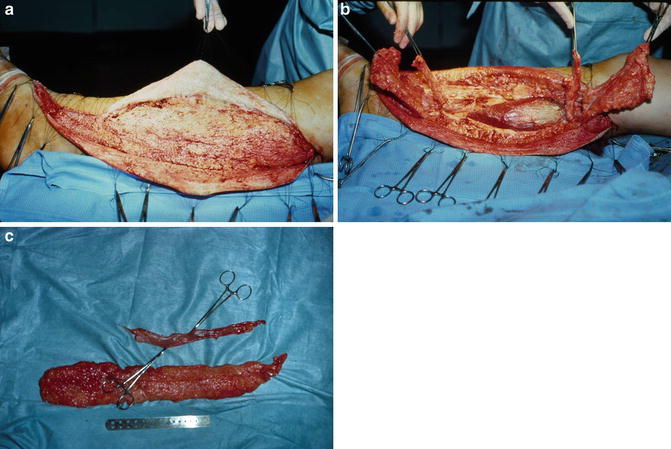
Fig. 27.1
The Charles Procedure

Fig. 27.2
This patient had a Charles procedure in childhood given her lymphedema present in the left lower extremity. “Mulliken and Young’s Vascular Anomalies: Hemangiomas and Malformations” edited by Mulliken, J.B., Burrows, P. E. & Fishman, S.J. (2013) by permission of Oxford University Press, USA

Fig. 27.3
(a) This is the same patient who had the Charles procedure in childhood (see Fig. 27.2). Lymphedema is gone, but removing all subcutaneous tissue and applying split thickness skin grafts to the underlying muscle results in an abnormal configuration of the extremity. (b) This is the same patient who had the Charles procedure in childhood (see Fig. 27.2). Lymphedema is gone, but removing all subcutaneous tissue and applying split thickness skin grafts to the underlying muscle results in an abnormal configuration of the extremity. “Mulliken and Young’s Vascular Anomalies: Hemangiomas and Malformations” edited by Mulliken, J.B., Burrows, P. E. & Fishman, S.J. (2013) by permission of Oxford University Press, USA

Fig. 27.4
This is the same patient who had the Charles procedure in childhood (see Fig. 27.2). Note the multiple Band-Aids® covering the areas of chronic breakdown, a common late sequelae of the Charles procedure. “Mulliken and Young’s Vascular Anomalies: Hemangiomas and Malformations” edited by Mulliken, J.B., Burrows, P. E. & Fishman, S.J. (2013) by permission of Oxford University Press, USA

Fig. 27.5
Long-term results of the Charles’s procedure. There can be concern for cutaneous breakdown, disfigurement of the extremity, and concern for squamous cell carcinoma of the grafted site. “Mulliken and Young’s Vascular Anomalies: Hemangiomas and Malformations” edited by Mulliken, J.B., Burrows, P. E. & Fishman, S.J. (2013) by permission of Oxford University Press, USA
Epstein, in 1984, reported a case of squamous carcinoma developing in a patient’s foot arising in association with long standing verrucous hyperplasia of congenital lymphedema [8]. Some authors still advocate Charles procedure for very severe lymphedema [8, 9]. There is no doubt that the procedure is the most effective for reduction in size of the extremity, but the secondary problems are too formidable to justify this operation, except as a last resort.
Homans extended Sistrunk’s operation, as suggested by Auchincloss [10, 11] (see Figs. 27.6 and 27.7). He excised the subcutaneous tissue and the deep fascia and created thin cutaneous flaps to cover the excised areas. The operation was done in four stages. The medial and lateral sides were done within weeks of each other. The subsequent procedures were carried out 2 months later [12]. Homans reported on eight cases: four patients needed only two or three excisional procedures, and the others had all four procedures. All patients were said to have a satisfactory result. Thus, the ablative principle, i.e., excision of large amount of edematous tissue, was established [10].
Fig. 27.6
John Homans (1877–1954): Born and bred in Boston he was educated at Harvard College and Harvard Medical School and served as surgical “House Pupil” at the Massachusetts General Hospital. While a staff member at the Peter Bent Brigham Hospital he wrote a textbook, Circulatory Diseases of the Extremities (date). His name is remembered for the sign of pain in the calf on active or passive dorsiflexion of the foot in patients with deep venous thrombosis of the calf. Homans once remarked (with a slight lisp) “If they had to name a sign after me; why didn’t they pick one that was damn good?” Courtesy of Harvard Medical School Alumni Assoc. Arch Surg 134:1019, 1999
Fig. 27.7
John Homans procedure
In 1967, Fonkalsrud was the first to advocate staged subcutaneous lymphangiectomy for congenital lymphedema in infants and children and a follow-up report in 1973 confirmed his earlier impressions [13]. Miller et al. presented excellent results using staged subcutaneous excisions in adults with lymphedema [14]. Lymphatic function was estimated using radioiodinated human serum albumin injections before and after staged excision. Their patients cleared 39 % in 24 h preoperatively, 43 % in 24 h 1 month postoperatively, but averaged 80 % per 24 h at 1 year postoperatively. These findings provided the first objective evidence that staged resection significantly increased clearance at 1 year.
Suction-assisted lipectomy (SAL) can be a first line operative intervention for extremity lymphedema because of its superior efficacy, consistent results, and low morbidity [15]. Excellent results are achieved using modern liposuction techniques (circumferential suctioning, tumescence, and power-assisted cannulas), with minimal morbidity and short recovery. This technique removes the excess, subcutaneous adipose tissue present in chronic lymphedema. The ideal candidate for SAL has moderate disease. Patients with minor disease do not require operative intervention. If major skin excess is predicted after (SAL) (as in severe lymphedema), the patient may be better managed by staged skin/subcutaneous excision [15].
Personal Surgical Protocol
Preoperative Preparation
We use a modified Homan’s procedure, or a modified staged subcutaneous excision, for lymphedema of the lower extremities [16]. The patient is placed on strict bed rest at home for 3–14 days before the procedure. One patient lost 54 lb by mobilization of lymphedematous fluid, without a diuretic. I do not routinely use a diuretic. The extremity is painted with povidone–iodine ointment every 8 h and wrapped with Kerlix™. A Jobst™ air splint is placed around the extremity; this is the simple model used for emergency treatment of fractures. The pressure is set at 30 mmHg and the splint is released every 4 h for 15 min, or as is necessary. A plastic margarine cup is stuffed with cotton and placed over the toes to prevent painful compression of the distal foot. This regimen results in a rapid shrinking of the edematous extremity in preparation for resection. Penicillin or erythromycin, if there a history of allergy to penicillin, is given 1 h preoperatively and continued for 7 days postoperatively or as long as drains are in place.
Technique
The first operation is on the medial aspect of the leg, as this incision is less visible. In patients with moderate and even severe edema, only one excisional procedure may suffice. If the lymphedema involves the foot and extends above the knee, we mark the incision on the medial aspect of the foot, continue behind the malleolus up the medial aspect of the knee, and proceed up the thigh (see Fig. 27.8). If the edema does not involve the thigh, the incision is gently curved and ends at the medial aspect of the popliteal fossa. The flaps are full thickness, but as thin as possible (see Fig. 27.9). The skin flaps are developed 1/6th the circumference of the leg medially and 1/6th laterally for a total of 1/3rd the circumference of the leg. The total length of the skin flaps is not made beyond 1/3rd the circumference of the leg to minimize the chance of necrosis (see Fig. 27.8). Using a Kelly clamp, a tunnel is developed beneath the subcutaneous tissue and removal of most of the edematous tissue is done by blunt finger dissection. The greater saphenous venous system invariably is removed and/or interrupted during the excision. Intradermal silk sutures are placed along the entire incision: there are used for traction during development of the cutaneous flaps (see Fig. 27.10a) [17].
Fig. 27.8
Incision on the medical aspect of the foot. The vertical arrow indicates length. The horizontal arrows indicate the width of the skin flaps. Each flap developed for one-sixth the circumference of the leg for a total exposure of one-third of the extremity. “Mulliken and Young’s Vascular Anomalies: Hemangiomas and Malformations” edited by Mulliken, J.B., Burrows, P. E. & Fishman, S.J. (2013) by permission of Oxford University Press, USA
Fig. 27.9
Flaps are full-thickness, but very thin. Holding sutures are placed in the dermal layer and used for traction to minimize manipulation of the skin. The exposed subcutaneous tissue and underlying fascia are removed entirely. “Mulliken and Young’s Vascular Anomalies: Hemangiomas and Malformations” edited by Mulliken, J.B., Burrows, P. E. & Fishman, S.J. (2013) by permission of Oxford University Press, USA