Fig. 21.1
a The expander prosthesis is placed in a submusculofascial pocket. b The musculofascial pocket is closed with a 2/0 Vicryl continuous suture, and two drains are placed in the subcutaneous space. c The skin is closed neatly with 4/0 Monocryl and the port is located using a magnet. It is possible to place up to half of the expander volume at this point, depending on the pocket size and the vascularity of the skin flaps
The patient is educated prior to discharge about drain stripping and emptying, and is followed up in the clinic in less than 1 week. Expansion usually begins 2 weeks postoperatively and 60–100 ml is placed on each visit until the goal volume is reached. If indicated, patients often have chemotherapy during this period. Total expansion to a volume of about 10–20 % over the required final implant volume generally requires five or six visits to the clinic. The expansion is allowed to consolidate for 2 weeks, and implant exchange may take place any time after that. Radiotherapy can be safely initiated 4 weeks after implant exchange.
When the patient returns for implant exchange, it is performed as an outpatient procedure. Implant sizers are selected preoperatively on the basis of the shape and dimensions of the tissue expander that was used, and the projected volume of the reconstructed breast. It is worthwhile stocking the correct sizers so that the surgeon has an accurate idea of how any given implant will look. It saves time, and avoids wastage of expensive implants. The operating room setup is critical to a satisfactory aesthetic outcome. The patient is positioned supine on the operating table so that she can be safely placed in a sitting position several times during the procedure. This is achieved by placing the arms and hands comfortably across the lower abdomen and padding and taping them securely. The head is placed in an elevated foam mold and is again taped to the operating table using a soft foam tape over a surgical pad. The skin of the forehead must be taped in order to prevent the head from slipping forward when the patient is placed in a sitting position intraoperatively. It is wise to check that the setup is secure before the patient is draped and inaccessible (Fig. 21.2).


Fig. 21.2
a For implant exchange the patient is carefully positioned with hands secured, padded, and taped across lower abdomen and with the head resting on an elevated foam mold with the forehead securely taped to the bed. b The pectoralis major muscle tends to force the expanders in an inferolateral direction, which must be addressed at the time of exchange to achieve medial fullness. c It is always wise to check that the patient is correctly positioned, and the table is functioning properly prior to preparing and draping the patient
After the patient has been draped, the old mastectomy scars are excised down to muscle and sent for pathological examination. The skin flaps overlying the muscle are carefully undermined and elevated to expose sufficient pectoralis major muscle to incise and remove the expander. The pectoralis major muscle should be incised in the line of the muscle fibers, at an angle sufficiently oblique to ensure that the muscle closure does not directly underlie the skin closure but rather bisects it. The expander is carefully removed, the capsule examined, and the patient is placed in a full sitting position. At this point, the height of the inframammary fold is set. The desired inframammary fold position is marked with ink on the skin, and a 2/0 silk suture is passed parallel to the desired fold position, approximating the dermis to the capsule and chest wall at the desired height. Four to six of these sutures are placed. The capsule anterior to this suture line is then incised to create ptosis in the inferior pole (Fig. 21.3). The remaining capsule is incised circumferentially using monopolar diathermy and a lighted retractor, and meticulous hemostasis is performed (Fig. 21.4a). It is often necessary to dissect the inferomedial pocket in order to medialize the final implant (Fig. 21.4b). A single submuscular drain is sited at mid-breast level, using the previous drain scars (Fig. 21.5a). Implant sizers are filled to their index volume and placed in the breast pockets (Fig. 21.5b). The skin is stapled closed and the patient is once again placed in a sitting position (Fig. 21.5c).
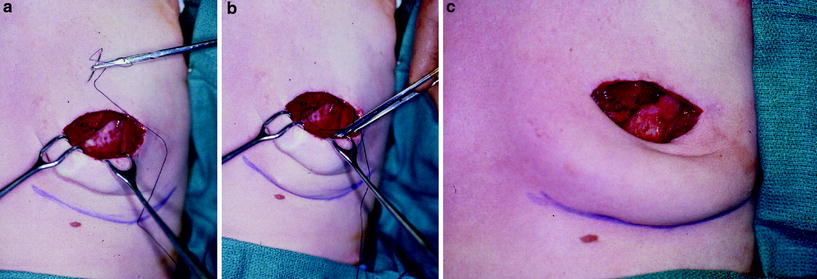
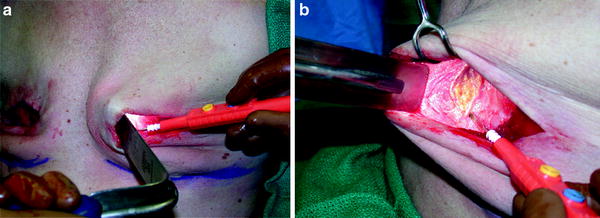

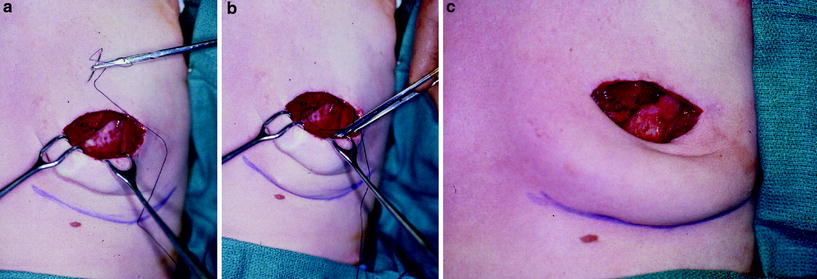
Fig. 21.3
a After removal of the expander, the inframammary fold is created with four to six 2/0 silk sutures firmly approximating the dermis of the skin flap to the capsule and periosteal tissue of the anterior abdominal wall to create a well-defined crease. b This technique requires careful inspection with the patient sitting up in order to achieve symmetry and a gentle, natural-looking crease. It is often necessary, even in experienced hands, to revise these sutures intraoperatively. c The objective is to achieve a gently curving inframammary crease
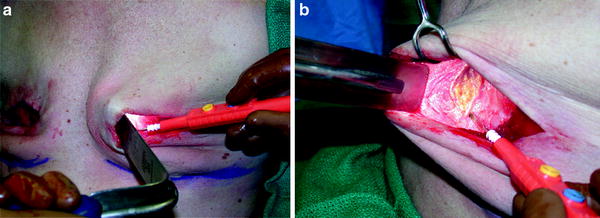
Fig. 21.4
a A circumferential capsulotomy is performed. b It is often necessary to dissect the pectoralis major origin inferomedially in order to medialize the final implant for optimal fullness

Fig. 21.5
a A single submuscular drain is placed at mid-breast level, ideally through one of the old drain scars. b Implant sizers are placed bilaterally and filled to the desired volume. c The muscle and skin are closed with skin staples, the patient is placed in a sitting position, and the breast pocket, inframammary crease, volume, and symmetry are carefully assessed. When the surgeon is satisfied, the sizers are removed and replaced with the corresponding final implant
Symmetry of the breasts is assessed by comparing inframammary fold position, medial, lateral and superior breast contours, and the degree of breast ptosis. There is a learning curve involved, and occasionally many modifications to inframammary fold position, sizer volume, and the implant pocket must be made in order to achieve a satisfactory result. This is a painstaking process, and it cannot be achieved without positioning the patient in a sitting position intraoperatively.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








