Soft-Tissue and Skeletal Injuries of the Face
Larry H. Hollier Jr.
Patrick Kelley
John C. Koshy
The treatment of the facial trauma patient continues to evolve with progress in imaging, bone fixation technology, and the application of microsurgical reconstructive techniques. Many of the principles of access, reduction, and fixation remain constant, but the application of these principles has been greatly facilitated with improvements in instrumentation and osteosynthesis technology. Facial trauma continues to be treated by a variety of specialists, including plastic surgeons, otolaryngologists, and oral surgeons. Plastic surgeons, however, are uniquely trained to handle the full range of issues present in the trauma patient.
INITIAL MANAGEMENT
Facial injuries themselves are rarely life threatening, but are indicators of the energy of injury. Initial care of all trauma patients focuses on the algorithmic protocol of ATLS (Advanced Trauma Life Support). Facial injuries should alert the examiner to the possibility of airway compromise, cervical spine injuries, or central nervous system injuries.
Airway
Airway compromise is the result of excessive bleeding from an upper airway source, foreign bodies (including aspirated teeth and bone fragments), or direct laryngeal injury. Often, upright positioning with cervical spine protection will improve airway function compromised by excessive bleeding or foreign bodies. Foreign bodies, when present, can also be mechanically removed by the finger-sweep technique. Airway compromise can also occur when the floor of the mouth and tongue lose support from a comminuted mandible fracture and can be alleviated by simple anterior traction on the mandibular symphysis.
The trauma team should have a low threshold for definitive airway protection via endotracheal intubation. The use of blind nasal intubation should be carried out with caution, as the procedure can exacerbate nasal and nasopharyngeal bleeding. Additionally, the tube may be inadvertently placed intracranially in the obtunded patient with a skull base fracture. Endoscopic nasal or oral intubation improves safety by avoiding cervical spine manipulation and further provides immediate confirmation of tracheal intubation.
Emergent tracheotomy is considered in the unusual circumstance of laryngeal fracture or inability to secure an upper airway route to intubation. Tracheotomy performed in the controlled environment of the operating room is far superior to either emergent tracheotomy or cricothyrotomy (also called cricothyroidotomy); however, certain situations will require this emergent procedure, and there should be a low threshold for performing an emergent tracheotomy or cricothyrotomy. There should also be a low threshold for a controlled, temporary tracheotomy procedure, in the patient with significant soft-tissue trauma to the floor of the mouth and tongue, especially the base of tongue, even if the airway appears stable initially. These injuries are more commonly penetrating in nature and initially misleading as there may be minimal early signs of distress. The swelling that develops over the next 24 to 48 hours, however, may be sufficient to compromise the airway, which may result in a tracheotomy under less than favorable circumstances.
Hemorrhage
The dense vascularity of the head and neck can cause significant blood loss from soft-tissue injuries. Fortunately, most of these injuries allow sufficient access to apply direct pressure and control bleeding. Pressure should be applied accurately and directly, as a number of critical structures can become collateral victims by attempting to clamp sources of bleeding with poor exposure and visualization. Bleeding that cannot be controlled with direct pressure requires packing. Packing in the nasal cavity is usually effective and only rarely requires augmentation with a transnasal balloon catheter in the nasopharynx. These catheters only serve to impede blood from entering the oropharynx where it can more easily enter the lungs. If massive hemorrhage is present, the airway should be managed first by emergent intubation, followed by packing and direct pressure. The source of bleeding is most commonly a branch of the external carotid system, which is most appropriately controlled with angiographic embolization. The radiologist frequently requires the assistance of the surgeon to remove the packing so that the bleeding source can be identified. At this time, and with all cases of significant hemorrhage, type-specific blood should be readily available. Surgical ligation of the external carotid artery is not adequate and will not control bleeding from its injured branches because of the robust collateralization present and should not be attempted (Figure 29.1).
Central Nervous System
Neurologic injury is commonly associated with severe facial trauma. A retrospective study of the National Trauma Data Bank found that the risk of head injury in the setting of isolated facial fractures ranged from 29% to 80%, with increasing rates as the fracture involved more cranial portions of the facial skeleton. In patients with multiple fractures, however, the incidence of head injury becomes more uniform, affecting between 66% and 89% of all cases presenting at major trauma centers. Identifying these injuries is important, as patients with facial trauma rarely die from facial injuries, but can die from associated injuries of the central nervous system. Most patients with facial trauma undergo computed tomography (CT) scanning. The most widely accepted method for expressing the degree of neurologic injury is the Glasgow Coma Score. This evaluates the motor, verbal, and eye-opening responses of the patient on initial evaluation, rating the patient from a lowest score of 3 to a highest score of 15 (Table 29.1).
As a general rule, concomitant head injury is not a contraindication to facial fracture repair, assuming the neurologic injury is stable and not in the process of evolution. In the event of acute brain injury, the surgical repair of facial fractures generally is delayed to avoid the fluid overload associated with surgery and, most importantly, to avoid undetected decline of neurologic function during the period of general anesthesia when clinical neurologic examination cannot be performed. Once the central nervous system injury and concomitant swelling have stabilized, facial fracture repair can generally be undertaken safely.
TABLE 29.1 GLASGOW COMA SCALE | ||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||
Facial fractures are also often complicated by cervical spine injuries. In fact, a recent study of the National Trauma Database found that 5% to 8% of isolated facial fractures and 7% to 11% of cases of multiple facial fractures will have an associated c-spine injury.1 Suspicion for injury and vigilant care of the cervical spine are key elements in the care of facial trauma patients. Cervical spine precautions are mandatory until the spine is cleared both clinically and radiographically. For the obtunded patient, the cervical spine is best evaluated with a CT scan, although a negative exam does not rule out unstable ligamentous injury. These patients require additional examination when the sensorium is clear and possibly flexion/extension radiographs or magnetic resonance imaging to definitively evaluate the cervical spine.
FACIAL TRAUMA EVALUATION
History
Use of the AMPLE acronym (allergies, medications, past history, last meal, events surrounding the accident) facilitates a complete trauma history.
Head and Neck Examination
A thorough head and neck examination is performed in a logical and consistent manner to avoid missed injuries. The examination includes the skin, soft tissue, neurovascular structures, and bone. Initially, gross examination identifies skin and softtissue defects and any exposed bone. Next, ecchymoses and soft-tissue swelling serve as red flags for potential underlying injury and are used with information regarding the mechanism of injury to develop a level of suspicion about the underlying injuries. Bony structures should be palpated in a systematic fashion to identify tenderness, deformity, or step-offs. In the acutely injured patient with facial trauma, however, the physical exam is greatly impaired by facial swelling, and facial asymmetries secondary to fractures are usually concealed. Additionally, it may be difficult to elicit tenderness because of simultaneous distracting injuries. The examiner must not be misled by more impressive injuries and overlook less obvious but potentially significant problems.
The examiner then carefully assesses the patient for neurologic deficits, including the trigeminal and facial nerves. Sensory disturbances in the forehead, cheek, and lower lip should be well documented, as should any deficits in facial nerve function. Nerve injuries that are not documented preoperatively may be attributed postoperatively to surgical intervention. Lacerations, contusions, and abrasions of the skin may focus the exam by indicating which nerves are at risk.
Much of the long-term morbidity of facial trauma is associated with ocular and orbital injury. Although there should be a low threshold to involve the ophthalmologist, the physician treating facial trauma should be well versed in the ocular examination. A complete ocular examination includes the evaluation of ocular history, acuity, light and red light perception, ocular motility, pupillary exam, and examination of the conjunctiva and eyelids. Each eye requires assessment individually.
Examination of the oral cavity is essential, especially in the obtunded patient who may have loose teeth, bone fragments, or foreign bodies. Identification and removal of prosthetics (e.g., dentures) is essential. The occlusion and intercuspation are carefully evaluated, as both mandibular and maxillary fractures can result in malocclusion. Patients are capable of sensing the slightest change in their occlusion. Even in patients with unusual bites, careful analysis of the wear facets may enable the surgeon to determine if an underlying malocclusion is present.
Proper record keeping of facial injuries includes rough sketch drawings in the medical chart and photographs to document injuries. These photographs may prove invaluable in the treatment of secondary deformities and can also be beneficial in medicolegal disputes. As such, photographic consents
should routinely be obtained as part of the treatment consent upon entrance to the emergency department.
should routinely be obtained as part of the treatment consent upon entrance to the emergency department.
Imaging
In almost all patients with facial trauma, CT scanning is performed and is acceptable for the diagnosis of essentially all facial fractures. The scan is performed with axial cuts no greater than 3 mm apart, from the top of the cranium through the bottom of the mandible. Additionally, in cases of complex facial trauma, it is helpful to have a three-dimensional reconstruction of the facial skeleton formatted so as to provide for a better overall orientation.
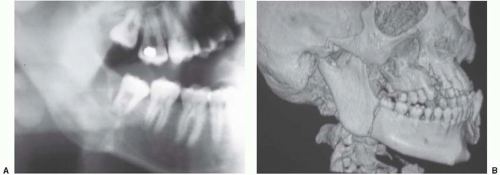
The one area where the CT scan may not be entirely sufficient is the mandible. Although the CT is essentially 100% sensitive and specific for the fractures, it does not give detailed information about dental structures. This is most critical in the region of the mandibular angle with respect to the condition of the second and third molars. Information regarding root damage and tooth position relative to the fracture affects the planning and treatment of angle fractures and is necessary to achieve optimal outcomes. For more detailed information regarding these variables, a panoramic radiograph is extremely beneficial. These radiographs evaluate the entire mandible, from condyle to condyle, in a single image and provide excellent detail of the condyles and dentition. Several downsides exist, though. First, the more commonly used panoramic devices require upright positioning and cervical spine clearance to be used, although certain less common devices allow the patient to be imaged while supine. Additionally, care must be taken when interpreting fractures based solely on a panoramic radiograph of the mandible, especially the symphysis and parasymphysis, as distortion of these regions can be misleading. In these cases, a supplemental posteroanterior film of the mandible complements the panoramic image by providing additional detail of the region. Lateral radiographs and/or CT scans can provide additional information about the regions posterior to the parasymphysis (Figure 29.2).
TREATMENT OF SOFT-TISSUE INJURIES
Preparation and Anesthesia
Facial injuries frequently involve contaminated wounds. The most important initial responsibility of the surgeon is to convert the contaminated wound to a clean one and then perform wound closure. Wounds are closed as soon as possible. Although facial wounds can usually tolerate up to a 24-hour delay in repair, the longer the wound is open, the greater the chance of infectious complications. Cleansing of wounds is best performed with a mild surgical soap with the light use of a scrub brush. More extensive wounds or those with a great deal of contamination should be irrigated with a pulsed lavage system. All foreign debris are removed from the wound prior to closure. Adequate cleansing usually requires total anesthesia of the region of concern and a cooperative patient. These are the primary factors that dictate the method of anesthesia necessary.
Although general anesthesia may be necessary for some wounds, many facial wounds can be repaired under a regional nerve block. If regional blockade is impractical, a field block may be necessary to avoid direct infiltration of excessive amounts of local anesthetic. Excess local anesthetic may cause distortion of anatomic landmarks that are useful in restoring the tissues to their anatomic positions.
Only 1 to 2 mL of anesthetic at the site of the nerve trunk is needed to provide complete anesthesia for the respective region. Often multiple regions require blockade. We recommend 1% lidocaine with 1:100,000 epinephrine solution mixed at a 9:1 ratio with 8.4% sodium bicarbonate solution (e.g., 9 mL lidocaine with epinephrine and 1 mL of bicarbonate solution). The bicarbonate solution neutralizes the pH of the lidocaine, which has two important benefits. First, it minimizes the pain of the injection. Second, the lidocaine more effectively crosses the neural membrane to affect its sodium ion channel in the neutral state and, therefore, has a quicker onset of action. Topical cocaine (4%) is an excellent choice for anesthesia in the nasal cavity as it also stimulates vasoconstriction of the nasal mucosa providing for a painless and bloodless field.
Traumatic Wounds
Traumatic wounds can be variously described as lacerations, punctures, contusions, abrasions, and crush injuries. The wound configuration, whether linear or stellate, is much less important to the final result than the degree of crush, contusion, and vascular compromise of the tissues. The importance of wound cleansing prior to closure cannot be overemphasized. Removal of all foreign bodies is essential as they are the source of a prolonged inflammatory response and possibly infection. Abrasions with residual foreign bodies will form a traumatic tattoo when not properly debrided. When tissue laxity allows removal of crushed tissue margins, a judicious sharp debridement of the wound margins is undertaken. Clearly devitalized tissue is excised. Freshening the wound margins contributes to rapid healing and improves the final result.
Perhaps the most important step in the repair of skin lacerations is excellent approximation of the deep dermal layer. By placing the tension of the closure deep to the skin, the resulting scar is improved. A good choice of the suture material for this deep layer is poliglecaprone 25 (Monocryl; Ethicon, Somerville, NJ). Because of the monofilament nature of this suture, it may have a lower likelihood of suture contamination and extrusion. It also maintains tensile strength for a sufficient period of time to allow for uncomplicated wound healing.
The choice of suture for the skin depends on the patient. Assuming a good deep dermal layer has been placed, the skin suture serves only to more accurately approximate and evert the skin edges. In children, it is beneficial to avoid a permanent suture to obviate the need for suture removal. An excellent choice in this case is 5-0 or 6-0 fast-absorbing gut suture. This suture type dissolves so rapidly that suture marks are not left on the face. It provides very little tensile strength, however, requiring the use of adhesive strips. If a skin adhesive is chosen in the pediatric population, one must take care not to place any within the wound itself, which may cause a profound inflammatory response, resulting in breakdown of the closure.
A subcuticular skin suture is also an option in the face. Monocryl is again a good choice. Should one desire to remove the suture, polypropylene may be the best choice as it slides out of the skin easily. Skin edges under a greater degree of tension are usually best closed using interrupted nylon or Prolene. In heavily contaminated wounds, interrupted sutures or running sutures in short segments can be used. This allows for removal of focal areas of suture in the case of infection, avoiding a complete wound dehiscence. As a general rule, sutures in the face can be removed by 5 to 7 days when they are load bearing. When a layer of reliable deep dermal sutures is in place, superficial skin sutures can be removed as soon as 3 days to avoid suture marks.
Injuries to Special Facial Regions
Eyelids.
The most important aspect of evaluating trauma to the eyelids is ensuring that injury to the globe has not occurred. A thorough ocular examination is an essential element. It is important to remember that the Bell phenomenon results in an upward and lateral rotation of the globe. As such, one may find penetrating injuries to the globe in locations that do not intuitively correspond to the eyelid injury.
Often a general anesthetic is required to provide sufficient anesthesia to explore eyelid injuries and allow for adequate exploration of the globe. General anesthesia is particularly recommended in the pediatric population where additional damage can be caused by working with sharp needles and instruments around the orbit in an uncooperative child. Direct injuries to the globe warrant urgent ophthalmologic consultation.
The most critical step in eyelid repair is placement of an everting suture along the lid margin. This facilitates proper alignment and makes notching of the lid margin less likely. The suture in the lid margin can be left long and taped down to the cheek to prevent the suture ends from irritating the eye. In general, all layers of the eyelid (inner, middle, and outer lamellas) should be repaired. Although the conjunctiva will heal well without sutures, injuries associated with significant deformity should be sutured with plain gut suture, burying the knots to avoid irritation of the globe. The middle lamella, including the tarsus, is repaired with resorbable suture. The skin of the eyelid is then repaired. Sutures are removed within 5 days. Depending on the magnitude of the injury, it may be helpful to place a Frost suture to support the lid position during healing, especially in injuries to the lower lids (Chapter 32).
Ears.
Ear lacerations can usually be sutured in one layer, addressing the skin only. It is typically unnecessary to place a separate layer of sutures within the cartilage. The firm adherence of the skin to the underlying cartilage framework of the ear ensures that skin approximation accurately aligns the cartilage.
The two most prominent concerns in ear injuries are hematoma and chondritis. Collections of blood in proximity to the cartilage can result in cartilage resorption or a reactive chondrogenesis, which ultimately leads to cauliflower ear deformity. Hematomas are evacuated as quickly as possible to avert this adverse sequela. Hematomas are drained through incisions in the overlying skin, making an effort to conceal incisions if possible. Because of the robust perfusion to the auricular skin, a bolster is often required to prevent reaccumulation of the hematoma. Alternatively, a small suction drain or Penrose-type drain may be used. A compression dressing is employed regardless of the type of drainage technique employed. Following treatment of significant lacerations, the convolutions of the ear are lined with antibiotic-impregnated gauze and the ear bandaged in a light head wrap, providing gentle compression of the ear.
As a general rule, ear trauma is not terribly painful. The development of pain in the posttreatment period may indicate hematoma or infection. Delayed onset of pain, therefore, warrants immediate inspection. Infection involving the cartilage (chondritis) is a serious complication. Cartilage has poor blood supply, making it difficult to treat chondritis with oral antibiotics. These patients typically require admission for intravenous antibiotics and possibly debridement. It is rare to develop a significant chondritis without concomitant pain. Chondritis that is overlooked or not treated promptly may result in loss of a significant portion of the auricular cartilage.
Nose.
Soft-tissue injuries of the nose are somewhat different from auricular trauma. When lacerations involve the underlying cartilaginous support system of the nose, all layers should be repaired after appropriate anatomic reduction. Simple reapproximation of the overlying skin does not necessarily align the underlying cartilage. As such, any lacerations or transections of the upper or lower lateral cartilages should be separately addressed. Because of the difficulty in achieving adequate anesthesia and control of bleeding with the use of local anesthetic alone, general anesthesia is warranted to maximize patient comfort and control.
Lips.
The most important consideration in repairing soft-tissue injuries involving the lips involves accurate reapproximation of the injured structures, especially the vermilion. A discrepancy in alignment of the vermilion border as little as 1 mm is noticeable at conversational distance. As such, prior to infiltration of any local anesthetic, the location of the vermilion border on either side of a laceration should be tattooed using a needle with methylene blue. The vermillion should be accurately reapproximated using a 6-0 nylon or similar suture.
Great care must be taken to separately reapproximate the underlying orbicularis oris muscle. Failure to do so will result in bunching of the muscle on either side of the laceration with attempted animation and typically results in a shortened scar with an exaggerated notching of the lip. Mucosal lacerations are repaired using a resorbable suture such as chromic or Vicryl (Ethicon, Somerville, NJ).
A careful examination is performed to rule out underlying damage to the dentition. Any loose or damaged teeth are documented. Particularly unstable teeth may benefit from a bridle wire securing them to adjacent stable teeth. Panoramic radiographs or periapical images may help to better delineate the underlying dental trauma.
Facial Nerve.
Soft-tissue injuries to the face involving the facial nerve are particularly devastating. In examining the patient with facial soft-tissue injury, particularly penetrating wounds, facial motion is examined carefully. One should specifically test elevation of brow, forced closure of the eyes, voluntary smile, and eversion of the lower lip. Eversion of the lower lip is not very well tested by asking a patient to purse
the lips; rather, it is best seen in attempted full-denture smile. Deficits in the presence of a penetrating injury likely represent transection of a facial nerve branch. As a general rule, all such injuries should be explored operatively. The exception may be suspected injuries to the buccal branches medial to the lateral canthus of the eye, as a consequence of the extensive arborization of the nerve at this level. Most such injuries will undergo spontaneous reinnervation over a 3- to 6-month period. Injuries lateral to this and any deficit in brow elevation, eye closure, or lower lip depression should be explored.
the lips; rather, it is best seen in attempted full-denture smile. Deficits in the presence of a penetrating injury likely represent transection of a facial nerve branch. As a general rule, all such injuries should be explored operatively. The exception may be suspected injuries to the buccal branches medial to the lateral canthus of the eye, as a consequence of the extensive arborization of the nerve at this level. Most such injuries will undergo spontaneous reinnervation over a 3- to 6-month period. Injuries lateral to this and any deficit in brow elevation, eye closure, or lower lip depression should be explored.
Timing is of importance in these situations. The ability to identify the distal transected nerve end is facilitated by stimulating with a facial nerve stimulator and detecting the facial motion. After approximately 48 to 72 hours, the distal nerve end can no longer be stimulated, greatly complicating accurate identification because of the small size of the nerve and the inflammatory response in the surrounding tissues. These injuries should be repaired using microscopic magnification and 9-0 or 10-0 nylon epineural sutures. The time to recovery for a repaired nerve can be approximated by measuring the distance between the site of injury and the target muscle. Nerve regeneration typically occurs at a rate of 1 mm/d after a 1-month lag (Chapter 9).
Parotid Gland/Duct Injuries.
The most significant concern in parotid injuries is the possibility of facial nerve injury. The facial nerve separates the parotid into a superficial and deep lobe, and lacerations in this region frequently injure both the parotid gland and facial nerve. A parotid gland injury does not require intervention unless the underlying parotid duct is involved. Involvement of the Stensen duct may result in a parotid fistula unless corrected. These injuries may be difficult to identify and may only be seen following repair of skin lacerations with subsequent accumulation of saliva. Identification and access to the distal segment of the Stensen duct can also be facilitated by cannulating the papilla opposite the maxillary second molar with a blunt parotid or lacrimal probe. The ends of the duct are freshened and repaired over a stent. We often employ a 5 French pediatric feeding tube brought through the papilla and secured intraorally to prevent inadvertent displacement during the healing period.
FACIAL FRACTURES
Orbital Fractures
Orbital Examination.
In patients with trauma involving the orbit, a thorough examination of the globe and associated structures is performed. If the patient has had previous iatrogenic globe penetration, such as cataract surgery or radial keratotomy, the risk of globe rupture following trauma is substantially increased. A visual examination is then performed, including an exam of the visual fields. Any damage to the optic nerve may manifest first as a limitation in the visual field rather than a significant change in gross acuity.
Additionally, one should test for color desaturation. The first indication of optic nerve compression may be red color desaturation. The easiest way to test this in the emergency department is to dim the lights and hold a penlight up to the finger. The light through the skin appears red. The patient should be asked with alternate eyes closed whether there is any difference in the intensity of the red color between the two eyes.
Direct and consensual pupillary responses are elicited to determine the function of the second and third cranial nerves. Anisocoria may be an indication of second or third nerve damage, or direct trauma to the iris. An afferent pupillary defect is indicative of optic nerve injury and can be elicited by a swinging flashlight test. Range-of-motion testing of each eye will determine the function of the third, fourth, and sixth cranial nerves. Restrictions in the range of motion of the globe should be confirmed with a forced duction test to determine if the restriction is caused by mechanical entrapment or by injury to the nerves or muscles. These emergency department maneuvers, although potentially quite informative, are no substitute for a thorough dilated exam by an ophthalmologist. Ophthalmologic consultation should be considered in every case of orbital trauma.
Indications for Surgery: Orbital Floor.
Indications for the repair of orbital fractures are an area of controversy. Mechanical entrapment of an extraocular muscle may be demonstrated on forced duction testing or on imaging studies and is an indication for surgical repair. A second surgical indication is evidence of enophthalmos. With the initial swelling present secondary to the trauma, any enophthalmos that is manifest indicates a significant deformity as it would be expected to worsen with the resolution of swelling. Deferring surgery will complicate the eventual repair that is required.
Defect size is the most controversial parameter in determining the indication for surgery. Various authors have used different guidelines.2 Many believe that any defect greater than 1 cm2 benefits from surgical repair because of the likelihood of subsequent enophthalmos. Other authors have tried to quantitate, via CT imaging, the actual increase in orbital volume compared with the uninjured side. This volume is then used to assess the risk of postinjury enophthalmos. Currently, there are no firm data confirming the usefulness of this approach.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree