CHAPTER 9 Short scar facelift
History
The short scar facelift with lateral SMASectomy was developed out of a demand from younger female patients (aged mostly in their forties) who sought facial rejuvenation but were adamantly opposed to any scarring behind the ears. These patients objected to the posterior hairline distortion, hypertrophic scars, and hypopigmentation that they often observed in their friends or mothers who had undergone facelifts. They were embarrassed to wear their hair up or in a ponytail.
Physical evaluation
Type I: The ideal candidate for short scar facelift

Fig. 9.2 Type I patient undergoing short scar facelift with plication only. A–C, Preoperative. D–F, 1 year postoperative.
Type II: The good candidate for short scar facelift
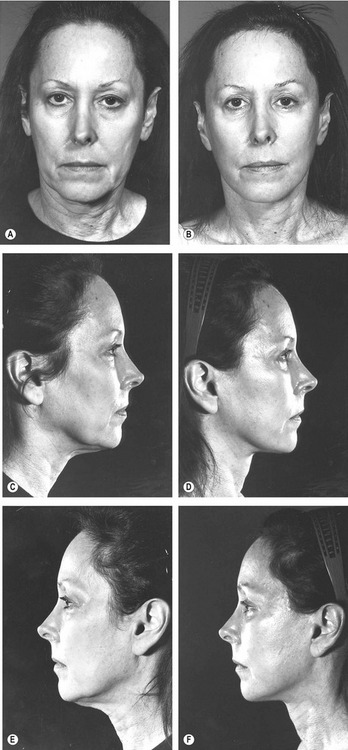
Fig. 9.4 Type II patient undergoing short scar facelift with plication only. A–C, Preoperative. D–F, 1 year postoperative.
Type III: The fair candidate for short scar facelift

Fig. 9.6 Type III patient undergoing short scar facelift with open submental SAL, liposuction, plastysmaplasty and lateral SMASectomy. A–C, Preoperative. D–F, 1 year postoperative.
Type IV: The poor candidate for short scar facelift
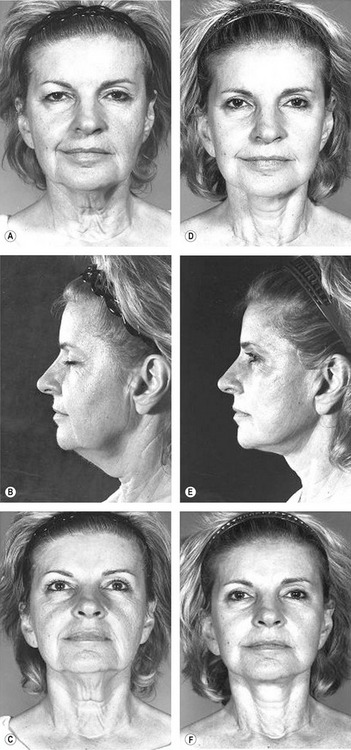
Fig. 9.8 A–F, Although this patient has a nice improvement after undergoing short-scar rhytidectomy, the 1-year postoperative result demonstrates persistent cervical laxity extending to the sternal notch. The patient was not happy and required neck revision with a classic retroauricular incision. This much cervical laxity can only be corrected with wide through-and-through undermining and removal of excess skin via the retroauricular occipital incision.
Technical steps
Incisions
When the temporal hairline shift is assessed as minimal, the preferred incision is well within the temporal hair. With this incision, it is often necessary to excise a triangle of skin below the temporal sideburn at the level of the superior root of the helix (Fig. 9.9).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree













