(1)
Klinik für Plastische Gesichtschirurgie, Marienhospital Stuttgart, Stuttgart, Germany
Electronic supplementary material
The online version of this chapter (doi:10.1007/978-3-662-49706-7_2) contains supplementary material, which is available to authorized users.
Keywords
Septal deformitySeptal reconstructionSeptal extension graftEthmoid bone splintingExtracorporeal septal reconstructionTotal septal reconstructionAnterior nasal spine transpositionDeviated noseCrooked nose2.1 Surgical Principles
The septum plays an important role in most cases of revision rhinoplasty, since residual deformity is often present. The residual deformity is often caused by an insufficient analysis and subsequent inappropriate or incomplete surgical technique. If this is the case, the long-term outcome is often disappointing, with drooping of the tip, saddling of the dorsum, and/or recurrence of the septal and/or nasal deviation.
The most challenging problem is a deformity of the anterior septum, specifically of the caudal border. To overcome this problem, we straighten the deflected part by means of suture techniques (modified horizontal mattress sutures) (Fig. 2.1) or by scoring, combined with splinting. For this purpose, we insert a straight cartilaginous piece from the posterior septum on the scored part or a thinned out perpendicular plate (Fig. 2.2). Alternatively, the whole septum can be removed for creation of a straight framework followed by replacement of the neoseptum (Fig. 2.3).
If the deformed anterior border has been resected and adequate tip support is lacking, progressive drooping of the tip will lead to an acute nasolabial angle. Additionally, a pseudo-hump deformity may result from tip ptosis and the prominence of the neighboring structures. In order to correct this, different techniques are available. Increased tip support can be achieved with a strong columellar strut. If there is not suitable septal cartilage, we prefer to use a sandwich graft from the concha (Fig. 2.4). This can be harvested easily, and by doubling the cartilage onto itself, a durable and straight graft can be created. Such a graft can be easily secured to the residual septal structure and will give reliable support to the tip. Alternatively, a septal extension graft can be used, but its stable fixation is more difficult. To stabilize the graft fixation, we use thinned and perforated perpendicular plates for splinting. Extended spreader grafts can be used as well, but they may be visible or even palpable if the grafts extend to the septal caudal border (Fig. 2.5). If shorter ones are used, the stability of the graft fixation is compromised.
Alternatively, the whole septum can be mobilized and brought into a more anterior position, which is a procedure equivalent to an extracorporeal septal reconstruction (Fig. 2.6). If adequate septal straightening is not performed during the primary procedure, a deviated dorsum and deviated axis of the nose will result. Permanent straightening requires splinting, which is best achieved with spreader grafts. These grafts have the added advantage of simultaneously widening the inner valves for better airway function (Figs. 2.7 and 2.8).
When using perpendicular plate for stabilization, the bone must be thinned thoroughly, and multiple drill holes must be added to facilitate secure fixation with multiple mattress sutures (Fig. 2.9). Furthermore, fibrous tissue will grow through the drill holes, which provides an additional means of stabilization. Although splinting with polydioxanone (PDS) foil is technically less demanding (although it has a high cost), it can be used only if the mucosal flap is intact. A review of our own cases revealed that PDS foil is unlikely to succeed without fully intact mucosa (Fig. 2.10).
If there is insufficient septal cartilage to permit spreader grafts for lining, strips of conchal cartilage can be used instead (7 see Fig. 2.7). Because conchal cartilage grafts are always curved, they must be applied to the deviated septum in a way that uses the opposing convexities to achieve a straight construct (Fig. 2.11). Alternatively, in some cases bone grafts from the perpendicular plate can also be used.
If there is insufficient septal cartilage available for creating a stable neoseptum, we prefer a total reconstruction from both conchae. To create a permanent straight cartilaginous framework, we suture the opposing convexities of the conchal cartilage opposite one another, stabilize them with several layers of through-and-through mattress sutures, and then sculpt them to the desired size and shape to create a neoseptum (Fig. 2.12).
A significant risk of any septal correction is a saddling of the dorsum. This may develop for two different reasons: (1) either the resection was too extensive and scar formation led to contracture and downward migration of the neoseptum, or (2) fixation to the anterior spine was insufficient, again leading to a saddle-nose deformity. Of course, such a deformity can be camouflaged by an augmentation graft, but this corrects only the aesthetic component. Consequently, if both shape and function are to be restored, a reconstruction using the principles of an extracorporeal septal reconstruction is required (Fig. 2.13). If there is no cartilage available, for example, because rib cartilage harvest was refused by the patient, a double-layered PDS foil used as a spreader graft may be an alternative solution (Fig. 2.14).
In all cases of extracorporeal septal reconstructions, a careful fixation to the upper lateral cartilage and the nasal bones as well as to the anterior spine is essential.
Regardless of the technique used for septal reconstruction, it is important to stabilize the caudal septum/medial crura/columellar strut complex to achieve adequate long-term tip support. For this reason, we always secure the reconstructed caudal segments with sutures. When using PDS stitches for this purpose, the stabilization is temporary, lasting for several months before the sutures are resorbed. As a minor complication, PDS sutures sometimes cause inflammation and discomfort owing to hydrolysis of the dissolving suture material. Erythema is occasionally observed in the area of mattress suture placement, but we have never seen a frank wound infection. If erythema is observed, we treat the area with topical antibiotic ointment and if necessary remove the central knot.
Transseptal mattress sutures work well only with septal or conchal (sandwich graft) cartilage. When using rib grafts, transseptal sutures may lead to an infection, most probably because the inner perichondrium, which protects the cartilage, has been resected during the procedure.

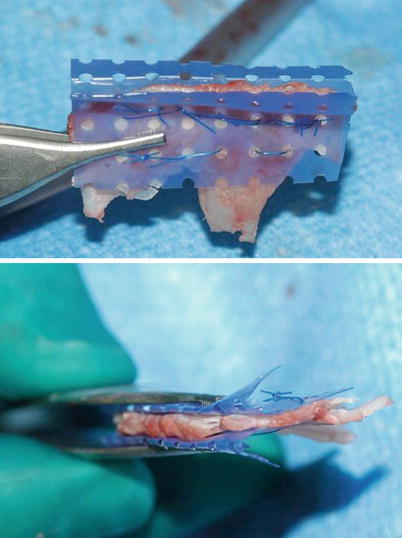
Fig. 2.1
(a–d) Straightening of the septum with suture techniques
Fig. 2.2
(a–e) Endonasal splinting of the scored anterior septum with a thinned transplant from the central septum
Fig. 2.3
(a–c) Extracorporeal straightening with thinned out perpendicular plate and spreader grafts
Fig. 2.4
(a–d) Sandwich graft from the concha used as septal extension graft
Fig. 2.5
(a, b) Septal extension graft from the central septum fixed to the anterior spine
Fig. 2.6
(a, b) Extracorporeal septal reconstruction for a deformed anterior border. The neoseptum is replaced in a more anterior position to correct the columellar retraction
Fig. 2.7
(a–c) Extracorporeal septal reconstruction in an overresected anterior border with spreader grafts from the auricle and correction of the retracted columella with a sandwich graft

Fig. 2.8
(a–d) Extracorporeal reconstruction of a straight septal frame using a unilateral spreader graft from the residual septum for the dorsum and both an onlay graft from the septum to the anterior border and a sandwich graft from the auricle for reconstruction of a retracted columella
Fig. 2.9
(a–e) Straightening with a thinned bone graft from the perpendicular plate with multiple drill holes for fixation and stabilization
Fig. 2.10
(a–d) Extracorporeal septal reconstruction in a multiple fractured septum, which had healed in dislocation. The separated straight pieces are fixed onto a PDS foil keeping it straight by spreader grafts, which are kept in position for suturing with a modified Aiach clamp
Fig. 2.11
(a–e) Extracorporeal septal reconstruction: straightening by a contralateral bent conchal cartilage graft used as a unilateral spreader graft
Fig. 2.12
(a–d) Total reconstruction of a stable septal framework by doubling conchal grafts
Fig. 2.13
(a, b) Reconstruction of a neoseptum from the residual septal components in combination with a conchal graft, both being fixed onto PDS foil
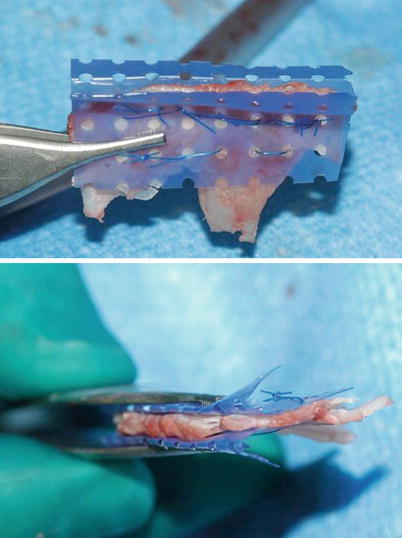
Fig. 2.14
Reconstruction of the internal valve using bended polydioxanone (PDS) foil
2.2 Case Studies
2.2.1 Case 1: Technique: Splinting of a Scored Septum with Ethmoid Bone
The ethmoid bone was thinned with a cylindrical motor drill and then perforated with multiple drill holes and applied with a Lindemann fraise. Fixation could then be performed using multiple back-and-forth mattress sutures.
A 42-year-old woman presented after two previous rhinoplasties. Despite previous septal scoring, there was a slight persistent septal deviation to the right. The deviation was eliminated using a thinned perpendicular plate splint that had been perforated with multiple drill holes for easier fixation to the septum itself and by using multiple back-and-forth mattress sutures for long-term stabilization. Using this technique, satisfactory straightening of the dorsum was accomplished (Fig. 2.15a–d).
Fig. 2.15
(a) Thinned ethmoid bone for splinting. (b) Front view pre-op/post-op after splinting the scored septum with ethmoid bone graft. (c) Profile view pre-op/post-op after splinting the scored septum with ethmoid bone graft. (d) Base view pre-op/post-op after splinting the scored septum with ethmoid bone graft
2.2.2 Case 2: Technique: Septal Extension Graft
A septal extension graft (SEG) can be used for a variety of indications, including nasal lengthening, lower level cartilages (LLC) contouring, tip support, or augmentation of a weak or overresected anterior septum. A strong and straight piece of septal cartilage is preferred for the creation of an SEG. Suture fixation of the graft can be performed in two different ways, depending upon the anatomy. When the caudal septum is reasonably strong and stable, the SEG can be sutured directly to the caudal septum in a side-to-side configuration for secure immobilization. Alternatively, the SEG can be stabilized using a single (or paired) extended spreader graft or splinting grafts (single or paired from bone or cartilage) when septal support has been compromised or when aggressive nasal lengthening is desired. However, care must be taken to contour the SEG to fit the anterior septal contour precisely.
A 35-year-old female presented after several failed rhinoplasty surgeries. Profile examination revealed a hanging columella, an overresected bony dorsum, and an overprojected lower nose. Frontal examination revealed a deviated nose with an inverted-V deformity, an oblique columella with dislocation from the anterior nasal spine (ANS) into the left nasal vestibule, and asymmetrical nostrils with bilateral alar retraction.
Upon exploration with the open rhinoplasty approach, copious fibrous scar tissue was found covering a weak and unstable caudal septum. Consequently, a large piece of cartilage was harvested from the posterior quadrangular septum and sutured to the caudal septum as a septal extension graft (Fig. 2.16a). Using transverse drill holes created in the ANS, the base of the caudal septum was then sutured in the midline to the ANS (Fig. 2.16b). To straighten the dorsal L-strut, 8 cm of the ninth rib was harvested and cut diagonally into 1.5 mm wide strips, which were used as extended spreader grafts. In addition to straightening the middle vault, extended spreader graft placement stabilized the septal extension graft and eliminated the inverted-V deformity. Tip deprojection was performed using a lateral crural overlap technique followed by tongue-in-groove fixation of the medial crura to the septal extension graft for elimination of the hanging columella. Asymmetrical alar rim grafts were placed to correct tip asymmetry and to contour and strengthen the alar rims. The remaining cartilage was finely diced and used as onlay graft material to smooth the nasal dorsum (Fig. 2.16c–e).




Fig. 2.16
(a) Endonasal stabilizing of a weak caudal septum with a septal extension graft. (b) Straightening the weak anterior septum with septal extension graft and fixing it in the midline. (c–e) Front view, profile view, base view pre-op/post-op
2.2.3 Case 3: Technique: Suture Fixation of the Neoseptum to the ANS Using Osseous Drill Holes
Secure fixation of the septal construct after extracorporeal septal reconstruction is essential. In addition to secure cranial fixation of the construct to the ULC and nasal bones, stable caudal fixation to the ANS is equally important. In order to facilitate stable fixation of the septal construct directly to the ANS, a small transverse drill hole is placed to permit passage of the fixation sutures. Whenever possible, this is also combined with the creation of a sagittally oriented groove created within the ANS to further stabilize the neoseptal construct. The neoseptum is also sutured with at least three passes of 4-0 permanent suture placed at different points within the construct to increase stability.
A 53-year-old male patient presented for revision surgery. Examination revealed a bulky tip and a deviated nose secondary to a severe residual deformity of the nasal septum, including dislocation of the caudal septum into the left nasal vestibule with an oblique columella. An overprojected dorsum and an overly narrow cartilaginous dorsum with collapse of the internal nasal valve were also observed.
Using the open rhinoplasty approach, we observed an “accordion-like collapse of the medial crura.” Owing to the severity of the septal deformity, an extracorporeal septal reconstruction was required, including doubling of the anterior septum to create a straight caudal L-strut. Spreader grafts were then used to widen the pinched middle vault, and the neoseptum was sutured to the ULC, nasal bones, and ANS after a transverse drill hole and osseous sagittal groove were created in the ANS.
In order to compensate for septal shortening after folding the anterior septum, a double-layered conchal “sandwich” graft was used to lengthen the caudal septum and to provide a strut for the LLC. Tip refinement was accomplished using lateral crural underlay technique (cephalic fold-under flaps), spanning sutures, and a non-integrated shield graft. Rim grafts were used to enhance alar rim contour, and a single layer of allogenic fascia lata was used to smooth the nasal dorsum (Fig. 2.17a–d).
Fig. 2.17
(a) Extracorporeal septal reconstruction with fixation to the ANS via a drill hole, sandwich graft from the concha and shield graft for contouring the tip. (b–d) Front view, profile view, base view pre-op/post-op
2.2.4 Case 4: Technique: Creation of a Neoseptum with PDS Foil, Restoration of Strong Tip Support Using a Sandwich Graft from the Concha
The conchal cartilage was cut through to the perichondrium of the opposite side, and then the straight pieces were fixed to PDS foil. Using this technique, a stable anterior septum was created.
For additional tip support, a sandwich graft from the concha was used. By suturing reciprocal curves of the conchal cartilage to balance opposing forces and create a strong, straight graft, long-term stability is ensured. We use the modified Aiach clamp and suture the cartilage with a 4-0 nonresorbable suture on a sharp Keith needle.
A 37-year-old man presented with severe deformity of the external and internal nose after four previous rhinoseptoplasties.
The nose was significantly deviated to the right with asymmetrical nasal bones, asymmetrical nostrils, and an asymmetrical tip. The anterior septum was overresected, with drooping of the tip and a slightly retracted columella. Concavity of both alae was also observed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree