19 Secondary facial reconstruction
Synopsis
 Secondary revision is an inevitable and indispensable part of facial reconstruction.
Secondary revision is an inevitable and indispensable part of facial reconstruction.
 An accurate diagnosis of the missing parts is as important in secondary reconstructions as during the primary reconstruction.
An accurate diagnosis of the missing parts is as important in secondary reconstructions as during the primary reconstruction.
 A comprehensive reconstructive plan is needed from the start, including bailout strategies.
A comprehensive reconstructive plan is needed from the start, including bailout strategies.
Historical perspective
Much has been written about the principles of reconstruction by the giants and early pioneers of plastic surgery, including Tagliacozzi, Paré, Gillies, and Millard, among others. The aims are always to restore to normal. Over the last century many techniques of increasing sophistication have been described. Our armamentarium continues to expand, so that today the reconstructive surgeon has many options to consider for achieving the best possible result. To maximize the end result in complex reconstruction, it is in fact not uncommon to utilize every rung of the reconstructive ladder, or as Bennett and Choudhary have described, the “reconstructive elevator,” which takes the reconstructive surgeon directly to the best method of reconstruction based on the patient’s needs and within the surgeon’s realm of experiences.1
Diagnosis/patient presentation
An evaluation for secondary facial reconstruction begins with a thorough investigation into the history of the patient, in particular the operations and flaps that were previously utilized, paying close attention to the remaining donor vessels in the head and neck.2 Next, an accurate diagnosis of the missing parts has to be made. While it is generally obvious what the missing parts are for a primary reconstruction that immediately follows extirpation, it is less obvious in secondary reconstructions where tissues have been pulled closed or healed secondarily. It takes an astute plastic surgeon to visualize what constitutes adequate contracture release and the resulting defect. This attention to making the correct comprehensive diagnosis is especially important when evaluating a patient whose primary reconstruction was performed elsewhere. Subsequent revisions are individualized and dictated by the area and underlying cause that required reconstruction. Therefore, a surgeon who specializes in secondary facial reconstructions needs to be well versed in all rungs of the reconstructive ladder, especially when many first-line options have already been utilized.
Patient selection
Facial defects and deformities should be evaluated in a systematic manner, starting from:
1. Overall magnitude and extent of the deformity and its anatomical location.
2. Displacement of major facial subunits; for example, the eyebrows, eyelids, nose, ear, and lips.
3. The extent of contour distortion.
4. Location and quality of the scarring that is present.
5. The color, texture, and quality of the skin.
6. The presence, absence, and distortion of specialized cutaneous features; for example, the hairline, sideburn, and beard area.
7. The quality of the subcutaneous tissues, volume and distribution.
8. The function or lack thereof of the underlying musculature.
9. The integrity or deformity of the underlying bony or cartilaginous support structures.
10. The status and quality of tissues lining the oral and nasal cavity.
11. The loss of other specialized components such as the lacrimal apparatus, teeth, and an adequate and mobile tongue.
Treatment and surgical technique
Meticulous technique and planning should be emphasized at every step of a multistage facial reconstruction, as this makes subsequent operations more predictable. Planning and initial flap tailoring are critical first steps. Radiographs are useful to visualize the missing bony elements. We recommend the liberal use of preoperative and intraoperative models to simulate the missing soft tissues and/or bone in developing the plan.3 This maneuver at the commencement of an operative procedure allows for tailored flaps to be designed at the most ideal donor site.
In general, the principles that are observed in secondary facial reconstructions are:
1. Restore to their normal location uninjured or partially injured anatomical features.
2. Repair scar contracture and if possible place the scars along the natural crease lines.
3. Restore the contour, which may involve debulking or augmenting soft facial parts with dermis fat grafts or autogenous fat grafting.4,5
4. Restoration of contour is more important than the presence of scars.
5. Replace “like with like,” thus soft tissues should be replaced with soft tissues, and bony tissues with bone or bone substitutes.
6. Use local flap options with better color and texture match as advancement or transposition flaps to provide better cutaneous coverage of de-epithelialized, previously placed distant free flaps that may have been used.
7. Local specialized flaps, for example, hair-bearing flaps, to reconstruct specific subunits previously covered by large distant flaps are also used to help break up the scars and create an illusion of a more normal appearance.
8. If local flaps are not available to improve the color mismatch of distant flaps, consider the use of thin split-thickness skin grafts harvested from the scalp as overgrafts to resurface these areas after de-epithelialization of the existing flap.6
9. Carry out functional restoration of absent muscles of facial expression, especially for restitution of a smile and adequate closure of the eyelids and mouth. The options of free muscle transfer, with and without nerve grafts or local or regional muscle transfers of functioning muscle, can all be considered.
10. Restore adequate bony platform to repair bony contour deformities, or allow for dental rehabilitation with osseointegrated implants.
11. Carry out supplemental prosthetic reconstruction of nonreconstructible parts, for example, orbital and ear prostheses.
Intraoral and intranasal lining
Deficiency in intraoral and intranasal lining must be suspected in cases of internal or external perioral contractures, or when the lining is known to have been excised or irradiated. Deficiency in intraoral lining can manifest as dry mouth, lack of facial movement, or lack of oral competence. Therefore, prior to commencement of any perioral reconstruction, intraoral scars must be fully released and the lining reconstructed. Otherwise, any attempts at external skin replacement will be suboptimal. Replacements of intraoral lining include skin grafts, regional flaps, and distant flaps. While skin graft might appear to be most appealing because of its availability and simplicity, we have not found it to be durable, especially in scarred or irradiated beds. Distant flaps such as anterolateral thigh flaps and radial forearm free flaps are certainly reliable methods of replacing lining. However, in cases of multiple prior operations, those flaps may have already been utilized or may be needed elsewhere. Furthermore donor vessels are usually scarce. The facial artery musculomucosal (FAMM) flap, a composite flap with mucosa and muscle taken from the lateral cheek, should be considered as an option. This is best done at the first operation when wide exposure and easy access to supple mucosa are available. When harvested with the overlying buccinator muscle, this is a robust flap that can cover widths of 2–2.5 cm. It can be based either superiorly (retrograde flow) or inferiorly (antegrade flow) to cover a variety of oronasal mucosal defects, including defects of the palate, alveolus, nasal septum, antrum, upper and lower lips, floor of the mouth, and soft palate (Fig. 19.1).7
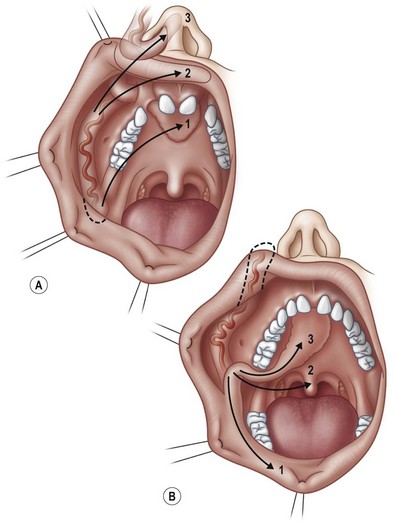
Fig. 19.1 (A) Superiorly based facial artery musculomucosal (FAMM) flap may be used for defects of the anterior palate, alveolus, maxillary antrum, nose, upper lip, and orbit. (B) Inferiorly based FAMM flap may be used for defects of the posterior palate, tonsillar fossa, alveolus, floor of mouth, and lower lip.7
With larger mucosal defects involving the floor of the mouth, the submental flap based on the submental branch of the facial artery is another useful regional option. Our experience indicates that this flap is generally very reliable with minimal donor site morbidity but should be used with caution if there was prior irradiation. Further it can be easily combined with the need for a neck dissection, though it is imperative to raise the flap and preserve its blood supply prior to commencement of the extirpative procedure.8
While vermilion is not strictly speaking intraoral lining, it is a specialized type of tissue that is impossible to reproduce. When vermilion is missing and cannot be borrowed from its neighboring areas, its appearance is much better matched with the use of nonkeratinized mucosa than the use of keratinized skin. In the early days of vermilion reconstruction, jejunal and gastric mucosa were attempted but were fraught with problems. The use of gastric mucosa in particular can be hypersecretory and its acidic contents ulcerogenic. FAMM flap, based superiorly for the upper lip and inferiorly for the lower lip, can give a good match for this specialized tissue.9 Alternatively, the use of lingual mucosa or tattooing of keratinized skin can also be acceptable.
Hair-bearing flaps
Successful facial reconstructions, especially in males, need to recognize the pattern of hair growth particularly in the sideburn and beard areas in order to maintain symmetry. However, few sites are available as hair-bearing donors. The temporal scalp, frontal scalp, and the submental region can all give satisfactory results.10
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree