Seborrheic Dermatitis: Introduction
|
Introduction
Seborrheic dermatitis is a common, chronic papulosquamous disorder affecting infants and adults alike. It is characteristically found in regions of the body with high concentrations of sebaceous follicles and active sebaceous glands including the face, scalp, ears, upper trunk, and flexures (inguinal, inframammary, and axillary).1 Less commonly involved sites include interscapular, umbilical, perineum, and the anogenital crease.2 The dermatitis presents with pink to erythematous, superficial patches and plaques with a yellow, branny and sometimes greasy scale. Excessive flaking on the face and scalp can lead to social embarrassment which can have a negative impact on one’s quality of life, especially in women, younger patients, and those with a higher educational level.3 Mild forms are most commonly encountered, but severe psoriatic and erythrodermic forms can be seen as well.1 Seborrheic dermatitis is one of the most common dermatoses seen in human immunodeficiency virus (HIV) and acquired immunodeficiency syndrome (AIDS) patients along with certain neurological disorders such as Parkinson disease.4,5 These patients tend to have widespread, erythrodermic, and treatment resistant forms. Severe forms are also seen with immunosupression in premature infants and congestive heart failure patients.6,7 African-Americans and other darkly pigmented races are susceptible to the annular or petaloid variant of seborrheic dermatitis, which may be confused for discoid lupus, secondary syphilis, or sarcoidosis.8 A rare pityriasiform variety of seborrheic dermatitis with ovoid scaling patches can be seen on the trunk and the neck, mimicking pityriasis rosea and secondary syphilis. A higher incidence of seborrheic dermatitis is also seen in patients with alcoholism and endocrinologic diseases that lead to obesity.9
Epidemiology
Seborrheic dermatitis is separated into two age groups, an infantile self-limited form primarily during the first 3 months of life and an adult form that is chronic. A male predominance is seen in all ages, without any racial predilection, or horizontal transmission. The prevalence of seborrheic dermatitis is 3%–5% of young adults, and 1%–5% of the general population, although its lifetime incidence is significantly higher.10
History
![]() In 1887, Unna first described seborrheic dermatitis. In 1894, Unna and Sabouraud hypothesized that yeast (Malessezia), bacteria, or both were responsible for causing seborrheic dermatitis, as both were cultured in high quantities from these patients.11 In 1984, Shuster showed that seborrheic dermatitis could be managed with oral ketoconazole, which has been further substantiated by numerous articles.12 The true cause of seborrheic dermatitis has been debated since it was initially described, but Malessezia is accepted as playing a fundamental role. Seborrheic dermatitis, also known as seborrheic eczema has been described in numerous ways over the last two centuries depending on the sites involved. The term seborrhea in its strictest sense implies oily skin and has been called dermatitis seborrhoides, seborrhea oleosa (Von Hebra), steatorrhagia, seborrhagia, and flux sebacea (Rayer). Terms in the past have included morbus Unna, hyperhidrosis oleasa (Unna; increased sweat and oil), crusta lactea in infants (milk crust, cradle cap), napkin dermatitis, and eczema flannelaire (rubbing of clothing, flannel and rough textiles on the skin results in lipid retention and exacerbation). Other terms include pityriasis sicca (dandruff, seborrhea/pityriasis capitis), pityriasis amiantacea (thick scalp involvement), and seborrhea blepharitis (seborrheic blepharitis, marginal blepharitis of the eyelids).13
In 1887, Unna first described seborrheic dermatitis. In 1894, Unna and Sabouraud hypothesized that yeast (Malessezia), bacteria, or both were responsible for causing seborrheic dermatitis, as both were cultured in high quantities from these patients.11 In 1984, Shuster showed that seborrheic dermatitis could be managed with oral ketoconazole, which has been further substantiated by numerous articles.12 The true cause of seborrheic dermatitis has been debated since it was initially described, but Malessezia is accepted as playing a fundamental role. Seborrheic dermatitis, also known as seborrheic eczema has been described in numerous ways over the last two centuries depending on the sites involved. The term seborrhea in its strictest sense implies oily skin and has been called dermatitis seborrhoides, seborrhea oleosa (Von Hebra), steatorrhagia, seborrhagia, and flux sebacea (Rayer). Terms in the past have included morbus Unna, hyperhidrosis oleasa (Unna; increased sweat and oil), crusta lactea in infants (milk crust, cradle cap), napkin dermatitis, and eczema flannelaire (rubbing of clothing, flannel and rough textiles on the skin results in lipid retention and exacerbation). Other terms include pityriasis sicca (dandruff, seborrhea/pityriasis capitis), pityriasis amiantacea (thick scalp involvement), and seborrhea blepharitis (seborrheic blepharitis, marginal blepharitis of the eyelids).13
Etiology and Pathogenesis
The exact pathogenesis of seborrheic dermatitis is yet to be fully elucidated, but this dermatosis is commonly linked with the yeast Malessezia, immunologic abnormalities, sebaceous activity, and patient susceptibility.14,15 The amount of sebum produced is not an essential factor, as not all patients with seborrheic dermatitis will have increased levels of sebum production. On the other hand, some patients with elevated sebum levels may not have seborrheic dermatitis either.16 Patients with seborrheic dermatitis show higher skin surface lipid levels of triglycerides and cholesterol, but lower levels of free fatty acids and squalenes. Both Malassezia species and the resident flora Propionobacterium acnes have lipase activity resulting in transformation of triglycerides into free fatty acids.17 All seven species of Malassezia are lipophilic except the zoophilic species, Malassezia pachydermatis. The free fatty acids and reactive oxygen radicals produced in turn have antibacterial activity that alters the normal skin flora. Some authors believe this disturbance in flora, lipase activity, and free oxygen radicals may be more closely linked to seborrheic dermatitis than an altered immune response.18
Immunology
Many patients have normal levels of Malassezia species on the skin, but have an abnormal immune response to it resulting in a depressed helper T cell response and less production of phytohemagglutinin and concanavalin when compared to control subjects.19,20 Levels of antibodies are the same in both patients with and without seborrheic dermatitis. Malassezia species also play a role in the inflammatory response with stimulation of the alternative complement pathway.21 A disturbed lymphocytic cellular immune response to Malassezia, results in elevated levels of interleukin (IL)-10, with a drop in IL-2 and interferon-γ.22 Both normal and elevated levels of antibodies to Malassezia furfur can be seen in patients with seborrheic dermatitis. Malassezia can lead to inflammation on the skin from metabolic products produced and complement activation via the direct and alternative pathways.
Physical Factors
Seasonal fluctuations in humidity and temperature are noted to flare this disease, particularly with low humidity and cold temperatures in the winter and early spring, with some relief in the summer.23 Facial PUVA (psoralen plus ultraviolet radiation) treatments and facial trauma (i.e., scratching) are also reported to trigger seborrheic dermatitis as well.24
Microbial Effects
The pathogenesis of seborrheic dermatitis has been disputed since it was originally described over a hundred years ago. The presence or imbalance of microbial flora likely plays a role in the disease. Although some patients may have cultures showing Candida albicans, Staphylococcus aureus, Propionobacterium acnes, and other aerobic bacteria, none have been linked to the pathogenesis of seborrheic dermatitis.25 Infants commonly have secondary contamination and infection with Candida species. The pathogenic role of Malassezia furfur (previously known as Pityrosporum ovale) is also controversial. The number of yeasts on the skin does not directly correlate with the severity of seborrheic dermatitis also. Patients with both dandruff and seborrheic dermatitis generally have abundant yeast counts when compared to controls supporting the role of yeast in the disease. A higher rate of seborrheic dermatitis is also seen in patients with Pityrosporum folliculitis and tinea versicolor.26 Clearance of seborrheic dermatitis with antifungals and recurrence following cessation of therapy also supports the premise that Malassezia species is pathogenic.27
Drugs
Several drugs are known to trigger seborrheic dermatitis like eruptions including griseofulvin, cimetidine, lithium, methyldopa, arsenic, gold, auranofin, aurothioglucose, buspirone, chlorpromazine, ethionamide, haloperidol, interferon-α, phenothiazines, stanozolol, thiothixene, psoralen, methoxsalen, and trioxsalen.
Neurotransmitter Abnormalities
Many neurologic disorders have been associated with seborrheic dermatitis, with most of them resulting in some facial immobility and sebum accumulation. These include Parkinson’s, Alzheimer’s, syringomyelia, epilepsy, cerebrovascular infarcts, postencephalitis, mental retardation, poliomyelitis, quadriplegia, trigeminal nerve injury and other facial nerve palsies.28 The fact that administration of l-dopa improves seborrheic dermatitis in some Parkinson patients, and some neuroleptic drugs that induce Parkinsonian symptoms can induce seborrheic dermatitis suggests that neurotransmitters may play a role in this dermatitis.29 Depression and emotional stress have also been reported to trigger seborrheic dermatitis.30 A high rate of this dermatitis is also seen among combat troops.31 In summary, these groups of patients do not have increased rates of sebum, but rather excessive accumulation of sebum on the skin.
Aberrant Epidermal Proliferation
Patients with seborrheic dermatitis may have epidermal hyperproliferation or dyskeratinization related to increased activity of calmodulin, which is also seen in psoriasis.32 This explains why patients with seborrheic dermatitis improve while being treated with a number of different cytostatic medications such as azeleic acid.12
Nutritional Disorders
Seborrheic dermatitis has not been proven to be associated with any vitamin deficiency. Patients with zinc deficiency (acrodermatitis enteropathica, and acrodermatitis enteropathica like conditions) may have an eruption that appears similar to seborrheic dermatitis and improves with zinc supplementation, while seborrheic dermatitis patients do not improve with zinc supplementation.33 Infants with deficiency in biotin, holocarboxylase, biotinidase, and free fatty acids may also have seborrheic-like dermatitis. But again, biotin supplementation has not been substantiated to improve seborrheic dermatitis.34
Genetic Factors
A family history of seborrheic dermatitis is often reported, but only recently has a mutation (ZNF750) encoding a zinc finger protein (C2H2) been described resulting in a seborrhea-like dermatitis. This Israeli Jewish Moroccan family presented with an autosomal dominant seborrhea-like dermatosis.35
Psoriasis and Seborrheic Dermatitis
The controversial term sebopsoriasis is often used in patients when there appears to be an overlap of psoriasis and seborrheic dermatitis. It tends to localize to the scalp, face, and presternal chest as seen with seborrheic dermatitis. However, the margins tend to be better defined, more erythematous and with thicker scales than those seen with seborrheic dermatitis. The biopsy can be indistinguishable from psoriasis, similar to the chronic form of seborrheic dermatitis.36
Clinical Findings
In all patients with seborrheic dermatitis, there is a so-called seborrheic stage, which is often combined with a gray–white or yellow–red skin discoloration, prominent follicular openings, and mild to severe pityriasiform scales. Several forms can be distinguished (Table 22-1).
INFANTILE: Scalp (cradle cap), trunk (flexures and napkin area), Leiner’s disease (nonfamilial and familial C3/C5 dysfunction). |
ADULT: Scalp, face, eyelids (blepharitis), trunk (petaloid, pityriasiform, flexural, eczematous, follicular, generalized, erythrodermic). |
Prognosis and Clinical Course
Self-limited with a good prognosis in infants compared to chronic and relapsing in adults. There is no evidence to suggest infants with seborrheic dermatitis will have disease as adults. Generalized flares and erythroderma can sometimes occur.37
Seborrheic Dermatitis in Infants Compared to Adults
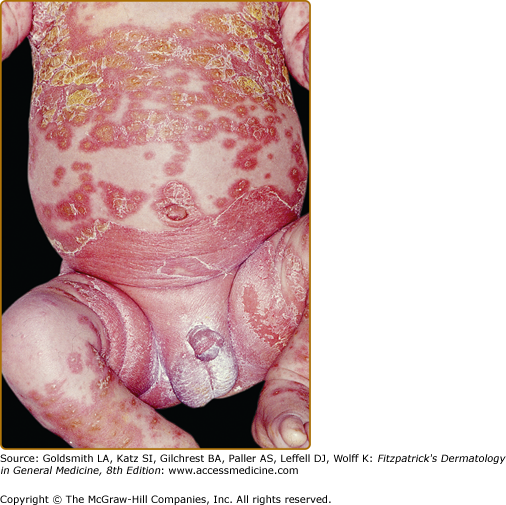
The infantile form occurs during the first few weeks to 3 months of life, is self-limited, and corresponds to the time when the neonate produces sebum, which then regresses until puberty.38 It is commonly concentrated on the vertex of the scalp (i.e., cradle cap) with adherent, yellow–brown, greasy scale, which can sometimes spread to the entire scalp with inflammatory, erythematous, and oozing crusts. Lesions can be seen on the face, neck and can be disseminated to the trunk and extremities with inflammatory glistening plaques in intertriginous sites such as the axillae and groin (Fig. 22-1). A differential diagnosis should be undertaken in any infant with a widespread form of seborrheic dermatitis (Box 22-1). Atopic dermatitis patients tend to have lesions on the forearms and shins, while sparing the axillae. Lesions isolated to the diaper region suggest seborrheic dermatitis. Radioallergosorbent assay test screening to egg whites, milk antibodies, soybean, and total immunoglobulin E levels, may be helpful in discerning infantile seborrheic dermatitis from atopic dermatitis. Some authors believe that infantile seborrheic dermatitis is actually a variant of atopic dermatitis rather than a separate entity. Extensive involvement plus lesions on the palms and soles with severe pruritis suggests scabies. Infantile psoriasis can also be extensive, with erythematous plaques and scale, with less scale in intertriginous sites. Extensive involvement with moist erythematous plaques and petechial lesions of intertriginous sites and the scalp suggests Langerhans cell histiocytosis (Letterer–Siwe) and should be biopsied for confirmation and treated appropriately.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree