58
Scaphoid Nonunion
James W. Vahey and Kevin D. Plancher
History and Clinical Presentation
A 38-year-old police officer presents with the chief complaint of progressively worsening pain and decreased range of motion in his dominant right wrist. He notes a history of a wrist injury from a fall 5 years ago when playing basketball. His evaluation at that time included radiographs that were interpreted as normal. He was diagnosed with a wrist sprain. His pain gradually subsided and became asymptomatic after an unknown amount of time. However, over the last 2 years he has noticed wrist stiffness, mild and occasional pain, and mild decreased wrist motion.
Physical Examination
The right wrist has no swelling. There is mild tenderness on palpation and mild tenderness with Watson shift testing; however, there is no subluxation. The right wrist range of motion is extension/flexion of +40/45, radial/ulnar deviation of 5/15, and pronation/supination of 85/85. The left, asymptomatic wrist range of motion is extension/flexion of +60/65, radial/ulnar deviation of 10/15, and pronation/supination of 85/85.
Diagnostic Studies
Posteroanterior, lateral, and scaphoid radiographs of the right wrist may demonstrate an established nonunion of the proximal pole of the scaphoid (Fig. 58–1). The sclerotic appearance of the proximal pole was consistent with avascular necrosis. There was no evidence of carpal malalignment or instability, including scapholunate and capitolunate angles within normal limits. No significant arthritic changes were present.
Magnetic resonance imaging (MRI) confirmed the diagnosis of avascular necrosis of the proximal pole of the scaphoid (Fig. 58–2). To obtain sagittal views of the scaphoid, MRI images were performed in the oblique plane oriented in line with the longitudinal axis of the scaphoid. These images demonstrated the fracture well and also confirmed that a “humpback” deformity was not present (Fig. 58–3).
Diagnosis
Based on Herbert’s classification of scaphoid nonunion, the patient had a closed, stage D5, scaphoid nonunion with avascular necrosis of the proximal pole.
Scaphoid fractures can be classified into four types. Type A is a stable acute fracture. Type B is an unstable acute fracture. Type C is a delayed union. Type D is an established nonunion. Herbert has described five stages of scaphoid nonunions (Fig. 58–4). If previous surgery has failed, a scaphoid nonunion should be classified one stage worse than suggested by its radiographic appearance.
PEARLS
- A high index of suspicion of a scaphoid fracture is warranted when a patient presents with the history of wrist pain following a fall on an outstretched hand even, if the radiographs initially appear negative. Very commonly, a patient with a scaphoid nonunion experiences an asymptomatic period (sometimes quite a long period) following his initial recovery from the acute trauma. The patient can present later with the history of the insidious onset of wrist symptoms. Alternatively, the patient can present after another traumatic event (often not even associated with high energy) with the onset of wrist symptoms.
- Useful techniques for identifying the nonunion site include identifying the position of the fracture along the longitudinal axis of the scaphoid from the preoperative radiograph, CT scan, or MRI, and scrutinizing the cartilage for the presence of wrinkling, buckling, or fibrous tissue. If the nonunion site cannot be reliably identified by any of these techniques, intraoperative fluoroscopy can be used to identify the location and a 25-gauge needle can be used to mark the location of the nonunion.

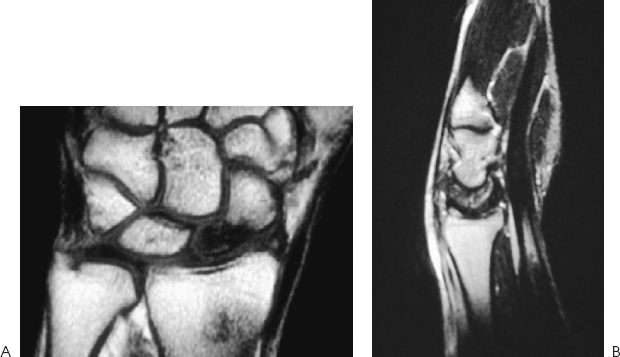
Figure 58-2. Posteroanterior (PA) (A) and lateral (B) magnetic resonance imaging (MRI) of a wrist at stage D5 scaphoid nonunion.
PITFALLS
- A humpback deformity of the scaphoid is a relative contraindication for a vascularized, pedicled bone graft because correction of the deformity is very difficult when performing the graft. Adequate correction of the deformity is more reliably accomplished from a palmar (Russe) approach with conventional trapezoidal corticocancellous bone grafting and Herbert screw fixation.
- The scaphoid nonunion may not be readily identifiable because the cartilage may be partially intact or fibrous tissue may be present.
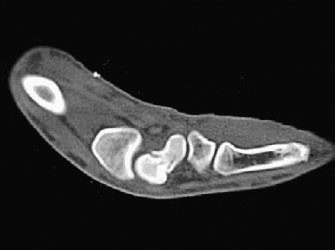
Figure 58-3. Computed tomography (CT) scan of a patient with a nonunion and humpback deformity.
Natural history studies of scaphoid nonunions suggest progression to wrist instability and subsequent wrist arthritis. Surgical treatment is usually indicated for patients with stages Dl and D2 regardless of the presence or degree of symptoms. Stages D3 and D4 have the presence of progressively more severe osteoarthritis, more loss of motion, and lower union rates. For patients with stages D3, D4, and D5 the patient’s age, symptoms, occupation, and needs should be taken into consideration when deciding among conservative treatment, scaphoid reconstruction, and a salvage procedure. For patients with stage D5 who do not have significant osteoarthritis and do not have a humpback deformity, a vascularized, pedicled distal radius bone graft can be considered. Some authors recommend vascularized grafts for patients with stage D5 who have humpback deformities. However, correction of the carpal malalignment pattern is difficult, and the likelihood of success is less than for patients without a humpback deformity.
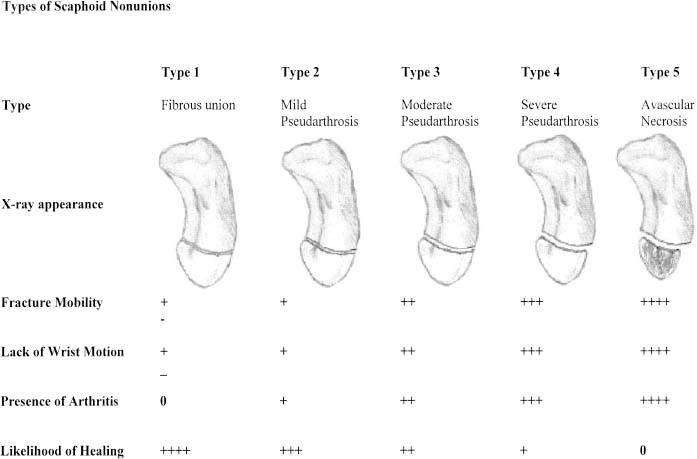
Figure 58-4. Herbert’s five stages of scaphoid nonunions.
Surgical Management
The patient was provided with a “clam-shell” anteroposterior thumb-spica splint that was custom fabricated by an occupational hand therapist. For the interval between the office evaluation and surgery, the patient was instructed to wear the splint at all times except to shower. Unlike a cast, a removable splint is less likely to cause skin problems prior to surgery, and the splint can be reused during the postoperative course.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








