2 Scalp Anatomy
Summary
Keywords: scalp anatomy galea aponeurosis periosteum carotid artery trigeminal nerve occipital nerve
Key Points
•Anatomy of the scalp is essential for the hair restoration surgeon.
•Rich vascularity protects the scalp, allowing for safety in performing flaps procedures or dense packing.
•Knowledge of innervation permits efficient anesthesia of the scalp.
2.1 Introduction
The skin that covers the head is called the scalp. Its primary function is to protect the cranial vault, providing a mechanical barrier to trauma and infection. The scalp also has an important aesthetic function, as it contains the largest collection of hair bulbs in our organism. In humans, hair is the only natural occurring element that may be decorated to display beauty, so hair-bearing scalp must be preserved whenever possible. The surgeon who is presented with a lesion to the scalp should appreciate this. Also, as it is the area where the hair restoration surgeon will primarily perform his/her procedure, knowledge of scalp anatomy is fundamental to his work. Microanatomy and histology of the hair follicle will be discussed in Chapter 3, Hair Anatomy and Histology for the Hair Transplant Surgeon (Video 2.1).
2.2 Surface Anatomy
The scalp extends from the eyebrows anteriorly, to the superior nuchal ridge posteriorly. Lateral limits are the zygomatic arch and the external auditory meatus. It is hair-bearing in all areas except the forehead where it is glabrous (i.e., hairless).1,2,3 In the child, the area of the scalp reaches 20% of total body surface, while in the adult this falls to less than 5%. Due to the loose deep connective tissue, the scalp is not tightly adhered to the skull but allows for a certain mobility. Curiously, some individuals are able to move their scalp by contracting the paired frontalis and occipitalis muscles.
The hair restoration specialist needs to be familiar with the nomenclature of the different areas of the scalp. Standardization permits a terminology that facilitates communication between professionals of different medical and nonmedical specialties.4 These regions are divided in major zones of the balding scalp (frontal region, midscalp, vertex, or crown) and several subregions (Fig. 2.1a, b).
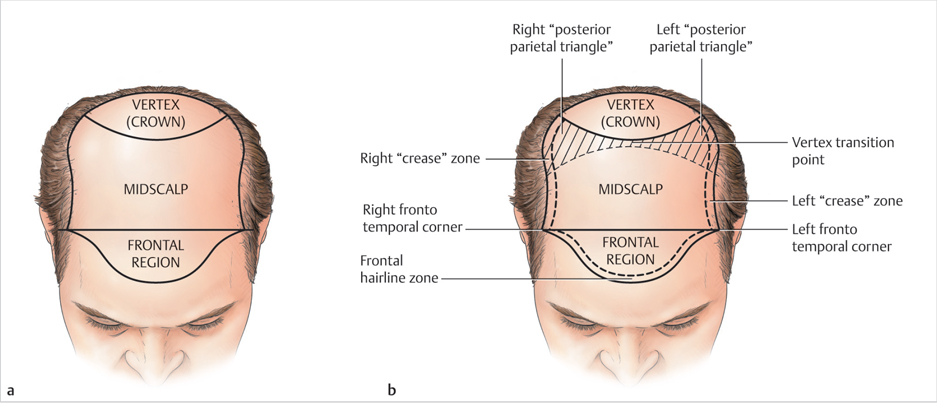
Fig. 2.1 (a) The main regions of the balding scalp. (b) Subregions of the scalp.
2.3 Layers of the Scalp
The scalp consists of five distinct layers of tissue, and they can be recalled by this simple mnemonic S C A L P: Skin, Connective tissue, Aponeurosis, Loose connective tissue, and Periosteum (Fig. 2.2).
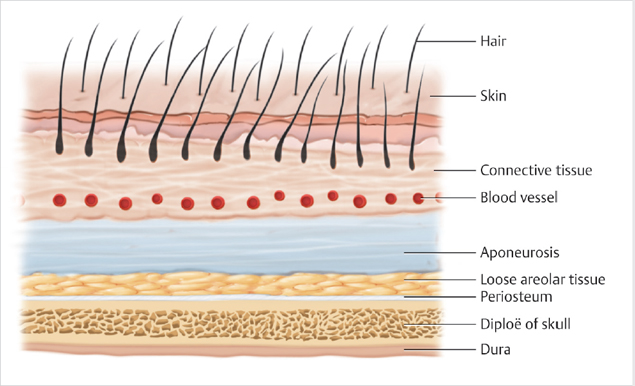
Fig. 2.2 Layers of the scalp.
The Skin is the most superficial layer of the scalp and consists of the epidermis (superficial layer) and the dermis (deep layer). The skin of the scalp is the thickest of the body, ranging from 3 mm (vertex) to 8 mm (occiput).
The Connective tissue (or sub Cutaneous) level consists primarily of fat lobules arranged between a network of fibrous septa that firmly join the skin above to the galea aponeurotica below. As a result, these top three layers of the scalp move together as a unit over the deeper subgalea layer of loose connective tissue.
An extensive network of arteries, veins, lymphatics, and nerves of the scalp are located in this layer. The rich blood supply helps limit infection, improve wound healing, and increase graft survival in hair transplantation surgery. However, blood vessels in this layer are highly adherent to the fibrous septa and therefore do not fully vasoconstrict when cut, thus potentially causing considerable bleeding even with small wounds. Wounds superficial to the galea bleed less than do wounds that cut through it, because the aponeurosis holds the skin tighter with less gapping.
The Aponeurosis or galea aponeurotica (in Gray’s Anatomy, also called epicranius) is a tough fibrous sheet that serves as an extensive ligament, joining the occipitalis muscle posteriorly to the frontalis muscle anteriorly.5 The two paired quadrilateral muscles insert into the dermis at the supraciliary arches (frontalis) and the superior nuchal lines and the mastoid (occipitalis). Laterally, the galea proceeds as the temporoparietal fascia and is continuous with the superficial musculoaponeurotic layer of the face (SMAS).
The galea is inelastic and thick, measuring 1 to 2 mm. The tensile strength of this layer makes it useful when suturing various types of scalp reduction and flap procedures. However, this same tensile strength can sometimes become an obstacle in scalp surgery, making it difficult to close scalp defects without tension. The use of galeotomy, scalp expanders, and scalp extenders can help alleviate this problem.6,7
The Loose connective tissue (subgaleal fascia) is a thin, loosely attached, and relatively avascular layer that allows for ease of undermining and mobilization of flaps with minimal bleeding. The only vessels found here are the emissary veins that connect the scalp with the intracranial venous system. Although rare, infections can arise in this plane and potentially progress via the emissary veins through the parietal foramina to involve the meninges. In certain areas, this layer of loose connective tissue does not exist, and the scalp will present with only three layers (i.e., skin, subcutaneous tissue, and deep fascia). Where five layers exist, wide excisions are feasible; where there are only three layers, scalp resection is limited. In some individuals, because the fibroareolar sheet is less developed there is less gliding of the overlying skin, and these are classified as “tight scalps.”
The Periosteum (or pericranium) is firmly adhered to the bones, especially over the suture lines (i.e., the coronal, temporal, sagittal, and lambdoid sutures).
In clinical practice, these four layers of the scalp may be regrouped into three coverings that appear distinct on modern imaging: the epidermis/dermis sheet; the subcutaneous stratum; the galea/subgalea; and periosteum covering.8
2.4 Blood Supply to the Scalp
The scalp derives its rich and abundant arterial supply via the external carotid and internal carotid artery systems, which supply five main paired arteries to each side of the scalp.
Branches from the external carotid system provide the blood supply to the posterior and lateral scalp via the following three branches:
•The occipital artery (back of the scalp).
•The posterior auricular artery (above and behind the ear).
•The temporal artery (lateral and frontal scalp).
Branches from the internal carotid system provide the blood supply to the anterior and superior scalp via two end branches of the ophthalmic artery:
•The supratrochlear artery (midline forehead).
•The supraorbital artery (lateral forehead as far up as vertex).
There is rich anastomosis between vessels on both sides of the scalp as well as on the ipsilateral side of the scalp, which explain why infection rates are low and flaps survival is often so good. After scalp avulsion, even a single arterial pedicle may be sufficient to revascularize the entirety of the scalp (Fig. 2.3). The use of the Doppler flowmeter to evaluate arterial flow is convenient when performing flap surgery on patients who may have aberrant vascularity (i.e., history of extensive trauma, previous scalp surgeries, or radiation therapy).
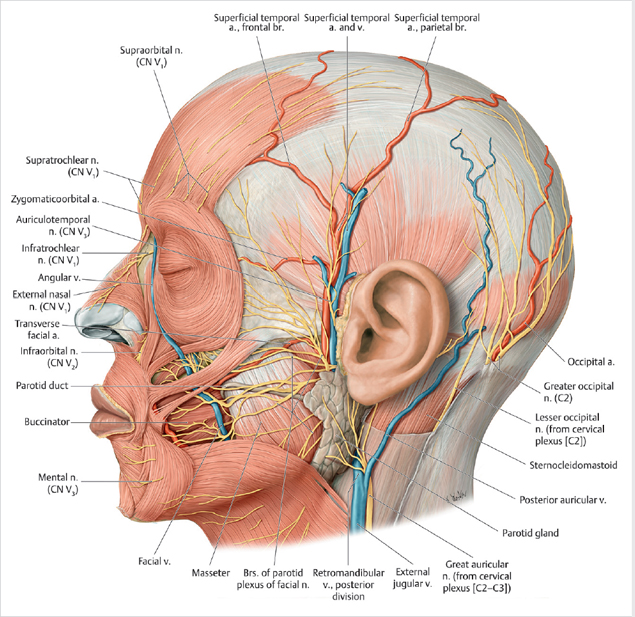
Fig. 2.3 Blood supply to the scalp. (Reproduced with permission from THIEME Atlas of Anatomy, Head and Neuroanatomy, © Thieme 2007, illustration by Karl Wesker.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






