Scalp
BIOANATOMY AND BIOMECHANICS
In a normal individual, the scalp is defined by the extent of dense terminal hair overlying the calvarium. In youth, the scalp is generously covered with hair. With age, thinning or outright hair loss is common. Without adequate photoprotection, the scalp is frequently burned and skin cancer of the scalp is common.
The scalp is supplied by an anastomosing series of moderate-sized arteries, which derive from the supraorbital and supratrochlear systems, the superficial temporal vessels, the postauricular arteries, and the occipital arteries. Most of the larger vessels run just above the galeal fascia and provide smaller extensions that supply the subcutis and dermis.
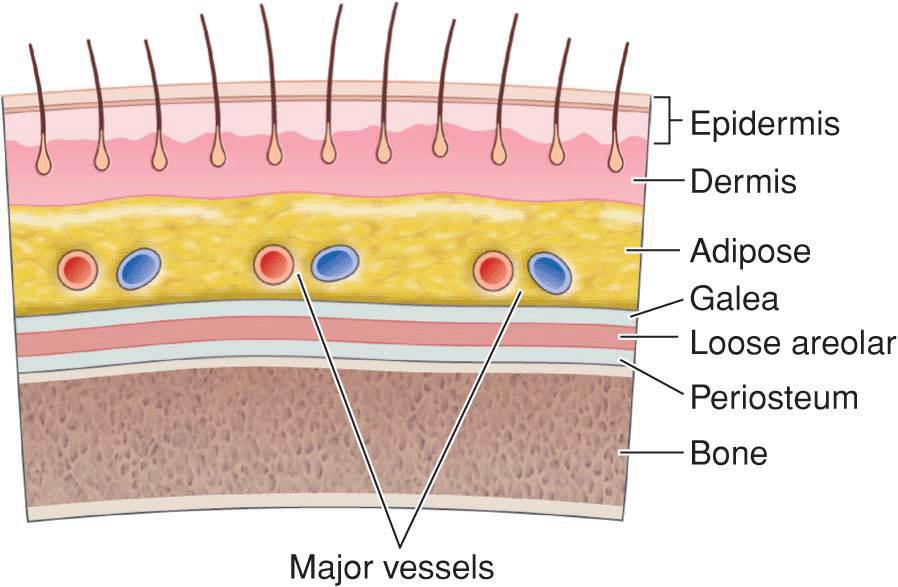
The structure of the scalp is defined by a layered system (Fig. 14.1). The dermis of the scalp is relatively thin and punctuated by numerous terminal hair follicles. The subdermal and subcutaneous plexi are richly supplied by innumerable vessels. The layer of adipose is highly variable from individual to individual and may be either very well developed or almost nonexistent. The first fascial layer is the galea, which envelopes the scalp and extends from the occipital musculature over the head and down to the superior orbital rim. Beneath the galea is a layer of loose areolar tissue, and finally, above the bone is an adherent layer of periosteum.
Figure 14.1 The scalp is characterized by a layered covering of epidermis, dermis punctuated by numerous hair follicles, adipose, fibrous galea, loose areolar tissue, and tightly bound periosteum. The major vessels of the scalp run just above the galea. The plane beneath the galea is easily dissected and contains only rare perforating vessels
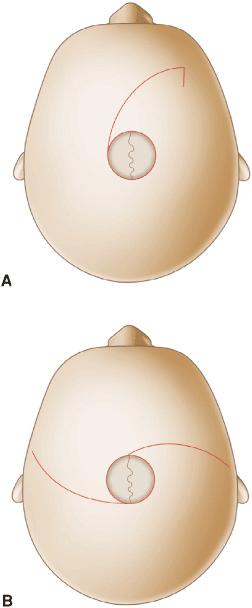
Mobility on the scalp is extremely variable and depends on multiple factors, ultimately being restrained by the rigidity and adherence of the galea. Some individuals have a scalp that is drum-tight and almost impossible to move. Others have a loose scalp that mimics the easily mobile skin of a Shar Pei dog (Fig. 14.2). Mobility can be divided into two zones, one being the ability to move the galea and the other being the mobility of the tissues above the galea. The loose, areolar tissue beneath the galea can be widely undermined in a relatively bloodless plane, and in some individuals, the galea may be closed over a reasonable distance. In many individuals, however, the galea is tight, and little to no additional mobility will be achieved by undermining. Galeotomies can be performed and do lead to some tension release, but they are challenging on direct side-to-side closures and risk transecting large-caliber vessels.1 Mobility above fascia is similarly variable and depends on multiple factors including the thickness of the adipose layer and the fibrous adherence of the overlying tissues to the galea.
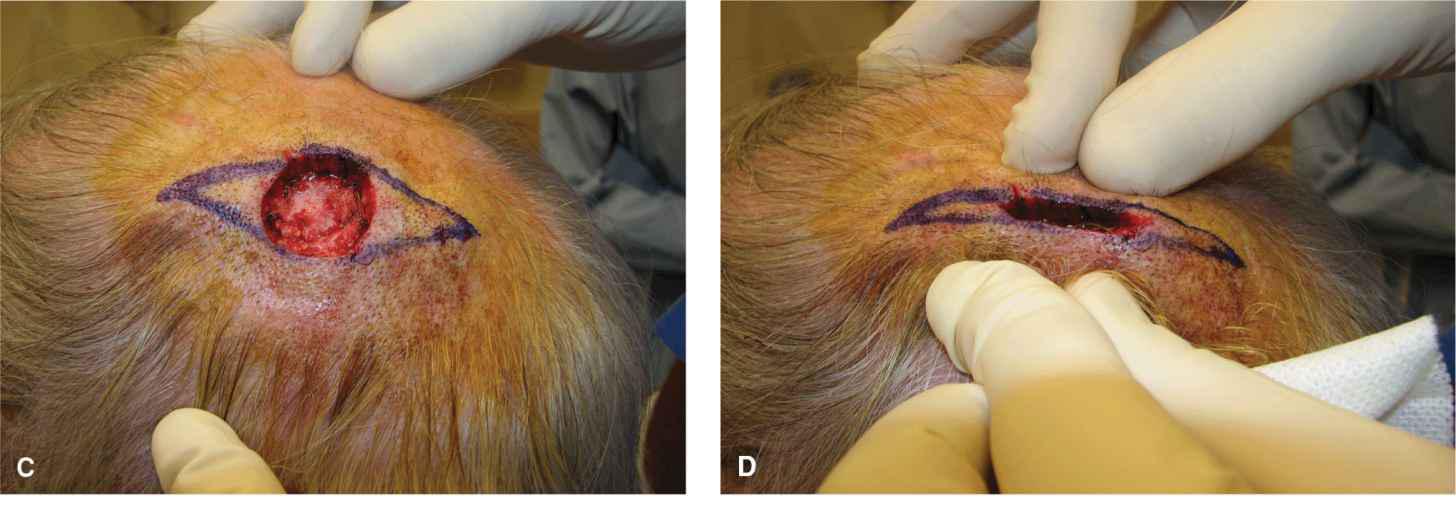
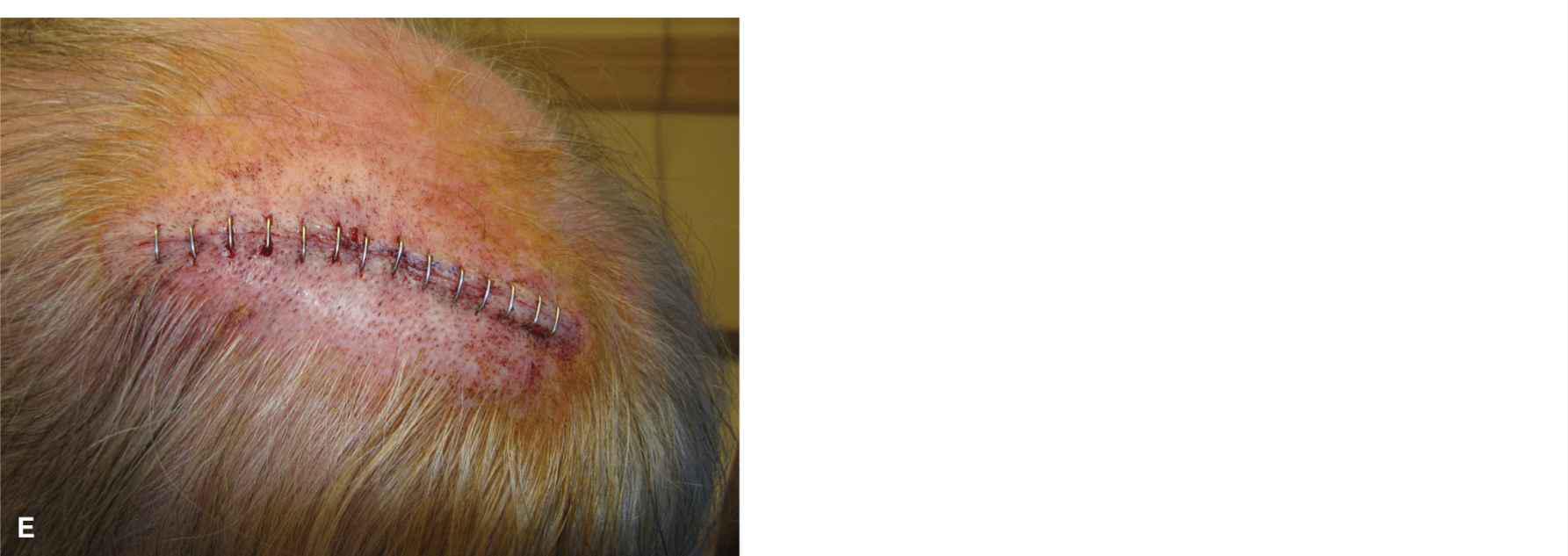
Figure 14.2 Some scalps are very tight and others are loose (Shar Pei scalp). (A) A moderate defect on a tight scalp. (B) An attempt to close this linearly fails due to a lack of laxity. (D) The patient has great laxity of the scalp. (E) The wound in this patient closes easily
The periosteum of the scalp is adequately vascular to nourish a skin graft, and its preservation, where feasible, substantially facilitates the repair of larger operative wounds. If the periosteum must be removed and bone is exposed, reconstruction may be complicated. When deep fascia and periosteum are removed during surgery, care should be taken to have patients in a recumbent position, as air embolism, sometimes fatal, has resulted during scalp surgery under local anesthesia.2 In an upright position, air can be sucked into rigid (open) perforating emissary veins and into the superior sagittal sinus.
APPICLACTION/SCALP REPAIRS
Linear Repairs
Many scalp wounds can be repaired linearly. Because of the convexity of the scalp, a longer fusiform ellipse is needed than might be expected, and a length-to-width ratio of over 4:1 is not uncommon. When considering a linear repair, it is important to evaluate mobility with caution. The scalp will give up to a certain point after which additional motion will be entirely restricted. If the wound does not easily close side to side by pinching the wound edges, it is unlikely to close without substantial tension.
For most wounds, linear repairs should be done in the subgaleal plane. Hemostasis is much more facile when the larger arteries have been severed and have retracted into the wound edges just above the galea. The galea should be closed as far as possible with buried interrupted sutures working from the edges to the center. In closing a scalp wound, it can be helpful to place a row of deep sutures, while access is easier, only tying them off after all have been placed. If a point is reached at which the galea will no longer close, the remaining wound may be closed with dermal sutures and horizontal mattress surface sutures. This may lead to a subtle depression of the center of the repair. For small wounds, it is reasonable to undermine above galea, albeit bleeding is more difficult to control. If a wound will not entirely close, and if no bone has been exposed, the central portion of the wound may be allowed to heal secondarily.
A number of devices have been designed to affect closure of tight scalp wounds. While they may have some use, alternate repairs will usually overcome such motion limitations without the use of machinery.
Rotation Flaps
Rotation flaps are commonly utilized on the scalp to repair wounds that would not be readily closed with direct side-to-side repairs. The dynamics of motion on the scalp, or more realistically the lack of motion in a single direction, make rotation flaps particularly suited to repair larger scalp defects. By creating rotation flaps, motion may be achieved from many directions and will allow for closure of substantial wounds. Rotation flaps on the scalp need to be large and long to achieve adequate tissue motion and tension redistribution (Fig. 14.3).3,4 An advantage of the scalp is that tension can be redistributed all the way along the primary and secondary defects without concern for displacement of free margins.
Figure 14.3 Rotation flap design on the scalp. Scalp rotations should be long and oversized to accommodate for a paucity of innate tissue motion. (A) In some cases, a single long rotation flap may be utilized. (B) Even when using bilateral rotations, the flaps should be of greater length than would be estimated to close similar wounds elsewhere
For small-to-modest wounds, a single rotation flap will be suitable to repair a larger operative wound (Fig. 14.4).5 More frequently, bilaterally opposed rotation flaps (O-Z) are utilized (Fig. 14.5).6 It can be unnerving to create and elevate such large and extensive flaps, but the creation of flaps that are too small will result in the inability to close the wound with the resultant need for second intention healing for a portion of the defect (Fig. 14.6). If the flaps are too small to affect complete closure, it is preferable not to force them closed under tension, as excessive tension on the tip of a scalp flap will quickly lead to ischemia and necrosis (Fig. 14.7).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree