What are the histological features of salivary glands and how are they related to oncogenesis?
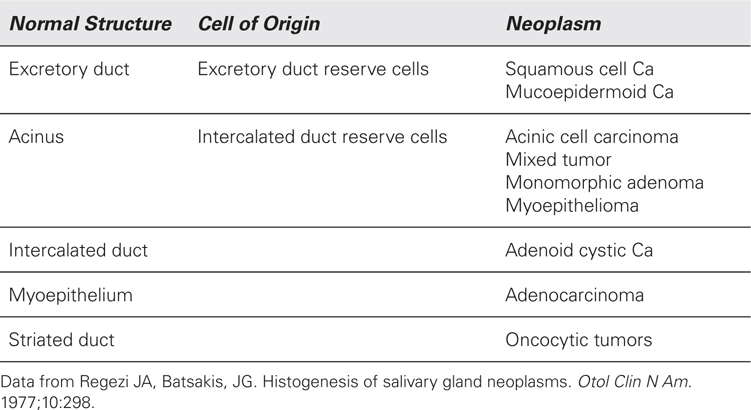
The parenchyma of the salivary glands is formed from the acini that lead to the sequence of ducts. While origin of the salivary tumors is poorly understood, there may be a correlation between the salivary neoplasms and the cells forming salivary units. This unit consists of acinus, intercalated, striated, and excretory ducts. Table 51-1 illustrates the correlation between normal structure and tumor cells.
Table 51-1 Histogenic Scheme of Salivary Gland Neoplasms
 Which salivary gland is the most common site for salivary tumors?
Which salivary gland is the most common site for salivary tumors?
Parotid gland harbors 70% to 85% of all salivary tumors.
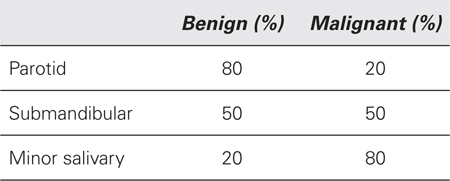
 What is the incidence of malignancy in different salivary glands?
What is the incidence of malignancy in different salivary glands?
 Tumors of which salivary gland are most frequently malignant?
Tumors of which salivary gland are most frequently malignant?
Sublingual gland.
Starting with lowest to the highest chance of malignancy the sequence is as follows:
Parotid < submandibular < minor salivary < sublingual gland
 Overall, what salivary gland harbors the most of the malignant tumors?
Overall, what salivary gland harbors the most of the malignant tumors?
Parotid gland. Although about 80% of parotid tumors are benign, the remaining 20% are malignant, and since tumors in the parotid are much more frequent than in all other salivary glands combined, the majority of malignant salivary glands tumors occur in the parotid gland.
 What is the most common benign salivary neoplasm for all salivary glands?
What is the most common benign salivary neoplasm for all salivary glands?
Pleomorphic adenoma (benign mixed tumor) is both the most common benign parotid neoplasm and the most common benign salivary neoplasm overall, comprising about 60% of all salivary tumors and about 80% of benign tumors. Mixed tumor is derived from dual epithelial (granular cells) and myoepithelial (mesenchymal) origin. The latter connective tissue (stromal) component often exhibits myxofibroid and cartilaginous differentiation. It has histologic appearance of stellate and spindle cells with a myxoid background. Pleomorphic adenoma has a potential for malignant transformation.
 The patient who was diagnosed with pleomorphic adenoma of the parotid (mixed parotid tumor) has another tumor in the same parotid gland. What is histology of the second primary parotid tumor most likely to be?
The patient who was diagnosed with pleomorphic adenoma of the parotid (mixed parotid tumor) has another tumor in the same parotid gland. What is histology of the second primary parotid tumor most likely to be?
Warthin’s tumor (papillary cystadenoma lymphomatosum) has a reputation of the most common second primary parotid tumor. The tumor histologically characterized by papillary cysts with mucoid fluid and the presence of lymphoid tissue (Think of intercalated parotid lymph nodes); Warthin’s is highly unusual outside the parotid gland and periparotid lymph nodes.
 Do any of the parotid tumors have propensity to be bilateral?
Do any of the parotid tumors have propensity to be bilateral?
Warthin’s tumors are bilateral in 10% of patients.
 A patient who has a symptomatic Warthin’s tumor in the parotid gland is found to have an occult contralateral parotid tumor on the CT scan. What would you do about it?
A patient who has a symptomatic Warthin’s tumor in the parotid gland is found to have an occult contralateral parotid tumor on the CT scan. What would you do about it?
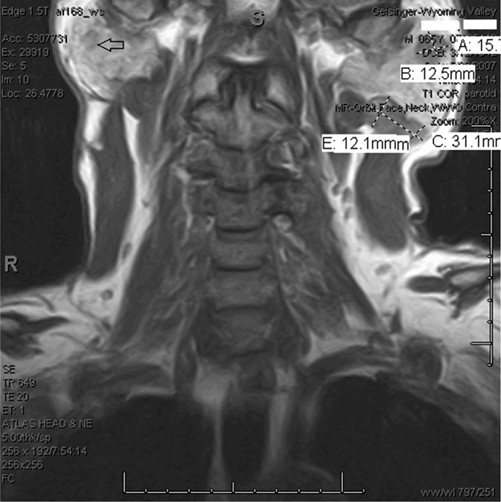
In the patients with bilateral Warthin’s tumors, the symptomatic side should be treated operatively, whereas you may observe an asymptomatic contralateral tumor. When it becomes symptomatic, you would remove it. Warthin’s tumor is known for being bilateral and multicentric (Fig. 51-1).
Figure 51-1 MRI of a bilateral and multicentric recurrence of Warthin’s tumor after incomplete superficial parotidectomy.
 Why are oncocytomas frequently found on the Tc-99 scans and what do you do with them?
Why are oncocytomas frequently found on the Tc-99 scans and what do you do with them?
Their origin is thought to correlate with striated ducts. This striation is related to the presence of large number of mitochondria. Tc-99 is preferentially picked up by tissues rich in mitochondria (gastric mucosa in the Meckel’s diverticulum lights up on Tc-99 Meckel’s scan). When oncocytoma is found on the scan and is not symptomatic, it may be observed initially.
 What is the most common malignant tumor of the parotid gland?
What is the most common malignant tumor of the parotid gland?
Mucoepidermoid carcinoma is the most common malignancy of the parotid. Histologically, it contains two major components of mucin-producing cells and epidermoid epithelial cells hence its name. Low-grade tumor is more common and greater mucin-secreting component. High-grade, poorly differentiated variant is largely solid with paucity of mucin-producing elements with the loss of differentiation.
 What is the most common malignant tumor of the salivary gland outside the parotid?
What is the most common malignant tumor of the salivary gland outside the parotid?
Adenoid cystic carcinoma (cylindroma) is the most common submandibular, sublingual, and minor salivary gland malignancy. There are three histologic types: the cribriform (“Swiss cheese” appearance), the tubular (resembles glandular architecture), and solid or basaloid pattern (solid sheets of cells without luminal or glandular appearance).
 What is the most common malignant tumor of the salivary glands overall?
What is the most common malignant tumor of the salivary glands overall?
Mucoepidermoid carcinoma. Low-grade variant is more common and is predominantly cystic, whereas high-grade tumors are solid with small amount of mucin.
 How do salivary malignancies spread?
How do salivary malignancies spread?
Lymphatic, hematogenous, direct invasion of the surrounding structures, as well as perineurally.
 Which head and neck malignancies are notorious for perineural spread?
Which head and neck malignancies are notorious for perineural spread?
Adenoid cystic carcinoma is a classic example. Malignant mixed tumor, melanoma, and squamous cell carcinoma also demonstrate perineural invasion.
 What are peculiar features of adenoid cystic carcinomas?
What are peculiar features of adenoid cystic carcinomas?
Lack a tumor capsule, direct invasion of the surrounding tissues, and very high propensity for perineural invasion. These three features make it very challenging to achieve negative resection margins. This tumor has hematogenous route of spread, which leads to the lung, liver, and bone metastases. It has excellent 5-year survival (75%), but poor 10-year survival, and even worse 20-year survival (13%); it tends to recur late.
 What are the important clinical features of acinic carcinoma?
What are the important clinical features of acinic carcinoma?
While the majority of the acinic carcinomas are curable, about 10% can manifest very aggressively and be tenacious with a tendency to recur.
 What is an important consideration in planning the removal of malignant mixed tumors?
What is an important consideration in planning the removal of malignant mixed tumors?
Malignant mixed tumors (or carcinoma-ex-pleomorphic adenoma) are locally destructive and require wide resection and frequently, microvascular flap reconstruction.
 What is the most common parotid tumor of young children?
What is the most common parotid tumor of young children?
Hemangioma.
 What are other common pediatric parotid tumors?
What are other common pediatric parotid tumors?
Most common benign epithelial tumor is pleomorphic adenoma. Most common malignant tumor is mucoepidermoid carcinoma, similarly for adults.
 Does the ratio 80:20 between benign and malignant parotid tumors apply to children?
Does the ratio 80:20 between benign and malignant parotid tumors apply to children?
No. Pediatric parotid tumors are much more likely to be malignant. In fact, an older child with a parotid mass has 50% chance of harboring malignancy.
 What is the most common presentation of parotid tumors?
What is the most common presentation of parotid tumors?
It is a mass below the angle of the mandible and not in front of the ear. The clinician needs to be aware that most parotid tumor present as upper cervical masses.
 Do you always feel parotid tumor on palpation?
Do you always feel parotid tumor on palpation?
No. Sometimes the presentation is subtle. If the tumor is in the deep lobe, only diffuse enlargement of the gland can be appreciated, and you have to rely on imaging to demonstrate the tumor.
 What about the size of the tumor? If the tumor is large, is it more likely to be malignant?
What about the size of the tumor? If the tumor is large, is it more likely to be malignant?
Not necessarily. You can have a large pleomorphic adenoma that has grown over past 20 years to be very large, yet still benign.
 A patient presents to you with a parotid mass, when should you think about malignancy?
A patient presents to you with a parotid mass, when should you think about malignancy?
Start with history and physical examination. Patient’s age, history of head and neck radiation, and history of previous malignancies and symptoms are important. Tumors in children and older individuals are more likely to be malignant. Pain and rapid growth are very suspicious for malignancy as are tumors that are adherent to surrounding structures on physical examination and have regional adenopathy. Facial nerve paralysis and eruption through the skin are rare even in advanced malignancy and are grave prognostic signs.
 A mass with facial nerve paralysis is a bad prognostic sign. What would be a benign condition that could have a similar presentation?
A mass with facial nerve paralysis is a bad prognostic sign. What would be a benign condition that could have a similar presentation?
Sarcoidosis is the most common cause for nonneoplastic parotid mass with facial nerve paralysis.
 What is importance of cystic parotid mass in an HIV patient?
What is importance of cystic parotid mass in an HIV patient?
A benign lymphoepithelial cyst is a cystic degeneration of salivary gland inclusions within intercalated lymph nodes. The cyst is lined with lymphocytes. It is manifestation of progression to AIDS. Treatment is repeat aspiration and careful use of a sclerosing agent.
 The patient presents with xerostomia dry eyes and history of long-standing periodic cheek swelling. On physical examination the patient has a unilateral ill-defined parotid mass. What clinical entity should be considered?
The patient presents with xerostomia dry eyes and history of long-standing periodic cheek swelling. On physical examination the patient has a unilateral ill-defined parotid mass. What clinical entity should be considered?
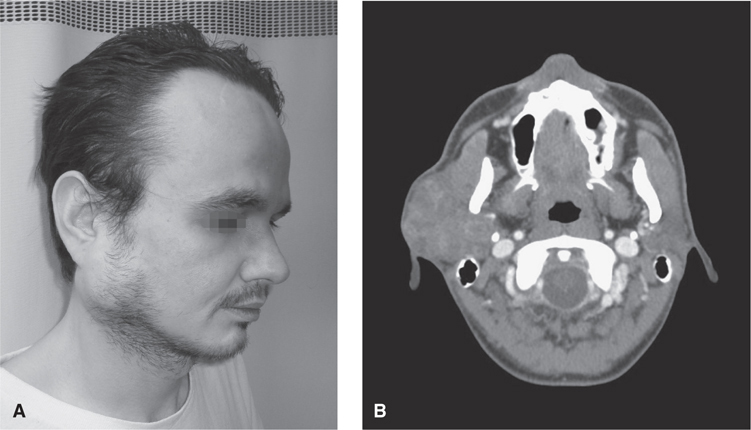
Clinical presentation of keratoconjunctivitis sicca and xerostomia is typical for Sjögren’s syndrome, a chronic progressive autoimmune disorder resulting from lymphocyte-mediated destruction of lacrimal and salivary glands. As the disease progresses, a sizable parotid mass may develop (Fig. 51-2). It may manifest as an isolated (primary) or associated with other autoimmune disorders (secondary) forms. A biopsy of a minor salivary gland, usually form the lower lip under local anesthetic in the office is a valuable diagnostic tool. Representative serologies, such as rheumatoid factor, ANA, SS-A, and SS-B are also frequently obtained. The risk of primary non-Hodgkin’s lymphoma of the parotid is increased.
Figure 51-2 Left parotid mass in a patient with a long-standing Sjögren’s syndrome. See Color insert.
The treatment is medical. Parotidectomy plays a very limited role in the case of Sjögren’s syndrome patients and is reserved for parotitis refractory to medical management, gross disfigurement, and diagnostic concerns of parotid lymphoma.
 How do you workup a parotid mass?
How do you workup a parotid mass?
After thorough history and physical examination (Fig. 51-3A), MRI is the best study; however, a good quality head and neck CT is acceptable (Fig. 51-3B). These will evaluate local and regional extent of the disease. CT imaging of the tumors of deep lobes and parapharyngeal space is undermined by scattering from petrous pyramids and MRI is the study of choice for those locations.
Figure 51-3 Large pleomorphic adenoma involving deep and superficial lobes of the right parotid. See Color insert.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree