CHAPTER 22 Saline Implants
Getting a Good Result
Summary/Key Points
Patient Selection
Given that nothing needs or should be done to the breast parenchyma and there is no change in the risk of breast cancer from the procedure1 a routine mammogram should not be required of patients preoperatively if there is otherwise no reason for one. If the patient needs a mammogram based on their age, physical findings, or some other reason, then they should have one done before the procedure.1
Physical findings of the breast that would preclude the patient from primary cosmetic breast augmentation as a sole procedure include active breast disease or undiagnosed palpable abnormality of the breast. Previous treatment for breast cancer or radiation treatment would put the patient in the category of breast reconstruction. Ptosis of the breast beyond about 2 cm into Grade II2 is a cosmetic contraindication to primary breast augmentation in my experience. Two centimeters or less can be compensated for using a properly placed breast implant and is usually of more benefit than any type of mastopexy procedure as long as the patient is willing to accept the increase in volume and understands that an implant will not truly lift the breast but only fills it out.
One of the listed complications of cosmetic surgery that is perhaps too common but can be avoided is the aesthetic risk of dissatisfaction with the result. This is best avoided by telling the patient what a breast augmentation can do and can’t do and what the patient can choose for her own reasons and what is being done based on experience of the surgeon on how to get the best result (Table 22.1).
Table 22.1 Key to getting a good result
| The key to consistent natural results with saline-filled implants requires thinking dimensionally as in fitting a woman for clothes or fitting an orthopedic implant and giving up thinking in terms of volume alone. This can all be done preoperatively and should not require choices made during surgery. |
| Avoiding visible rippling requires: |
• Matching the width of the implant to the width of the breast (excluding the skin and some of the subcutaneous tissue); |
| If the saline-filled breast implant is sized correctly, positioned correctly, filled correctly, and healed in the proper position, the result should look just like a result with a gel-filled implant in the majority of patients. Gel-filled implants are much more forgiving regarding sizing and positioning and there are no filling issues. |
| Palpable feel of the saline-filled implant, ‘rippling’ that is felt and not seen in the upright position, cannot be avoided with a saline-filled device but can be graded and understood by the patient at least for the immediate postoperative period. |
The other area that is often missed in the evaluation of patient selection is whether the patient has adequately prepared for the recovery. Contrary to efforts by some to convince the patient that they can return to normal activity the next day,3 I recommend treating breast augmentation as an orthopedic procedure and require that the patient has a week off from any and all required activities other than taking care of herself. This helps to magnify the consequences of the procedure and the importance of the recovery in the overall result as well as help to avoid precipitous surgery and poorly thought out choices. It also allows for the enormous variation in perceived pain and recovery difficulty among patients after what is ostensibly the same procedure.
Indications
Their major disadvantage is their inherent watery or ripply feel.
Silicone gel-filled breast implants have several disadvantages:
Their major advantage is their inherent natural or tissue-like feel.
Preoperative Planning
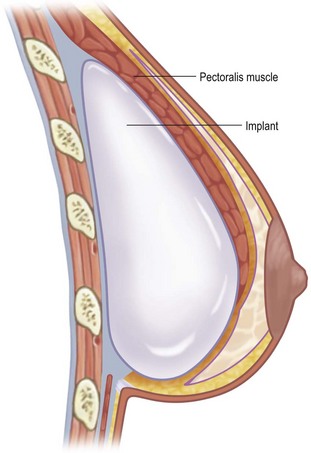
Degree of coverage starts from a rating of near zero and completely inadequate in a woman with thin or very soft skin, virtually no subcutaneous fat, and essentially no breast tissue. This is a situation comparable to someone whose ribs are sticking out or a woman who has had an aggressive subcutaneous mastectomy or full mastectomy. Perfect coverage would be rated a 3 with thick elastic skin, normal or more subcutaneous fat, and average breast tissue. In that situation, the woman is not going to be able to feel the implant to any significant degree and it won’t matter whether it’s saline-filled or gel-filled. In between the extremes are where most patients fall and there are those who have adequate coverage laterally but inadequate in the inferior pole, particularly in the somewhat ptotic or pseudo-ptotic (Fig. 22.1).
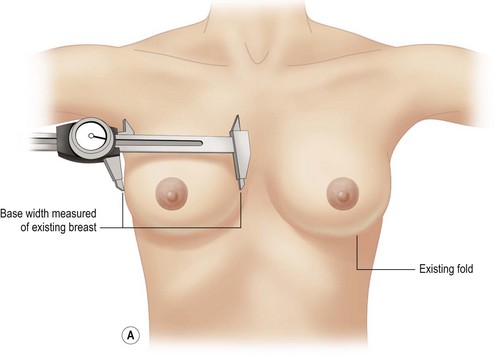
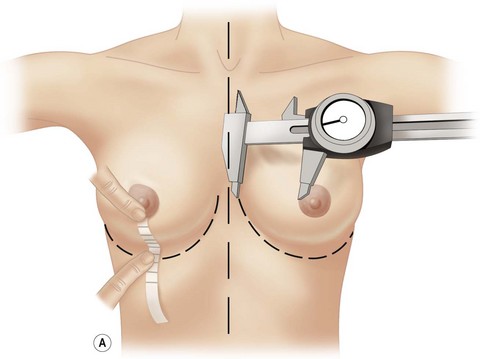
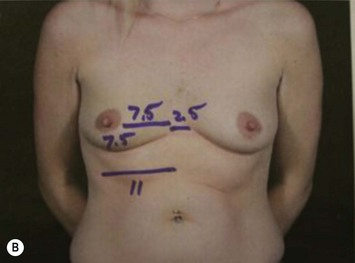
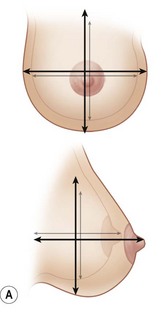
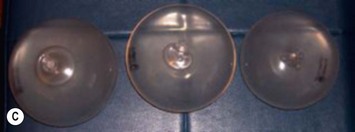
The patient has chosen saline implants and the profile of the implant. The width of the implant is determined by the width of the breast (Figs 22.2 and 22.3). Therefore, the correct implant is known before the procedure and can be confidently placed without using sizers, sitting the patient up during the procedure, or making choices for the patient on the operating table (Fig. 22.4A–C).
The only other marking required preoperatively is the position of the inframammary crease in the upright position. On the operating table, the distance from the medial border of the breast to the nipple (or medial edge of the areola) can be measured under no tension and compared to the distance from the nipple (or inferior edge of the areola) under tension. With few exceptions related to extreme lateral positioning of the nipple–areola, comparing these two measurements determines whether a round implant of the width of the inner diameter of the breast will fit and seat properly behind the nipple–areola. If the distance to the inframammary crease is too short, the crease must be lowered to the appropriate level and re-established and healed in the new position (Fig. 22.2A, B).
During the preoperative consultation, the physical characteristics of the breast should be noted and pointed out to the patient (see Box 22.1).
Box 22.1 Physical characteristics of the breast
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree