5
Rosacea
Victor Gabriel Clatici and Cristiana Voicu
DermaLife – Medlife Group, Bucharest, Romania
Introduction and Epidemiology
Rosacea has always been a topic of interest throughout history, its semiology being well known from the Middle Ages. Red faces were frequently associated with alcohol consumption, violent temperament, shameful sexual conduct, unhealthy lifestyle, or lower socio‐economic background [1].
Rosacea is a chronic and common skin condition characterized by specific signs and symptoms located mainly on the convex areas of the face (cheeks, nose, forehead, chin), such as facial erythema, dilated vessels, inflammatory lesions (papules and pustules), hypertrophic lesions named phyma, and sometimes accompanied by ocular irritation, with a potential important impact on the individual’s emotional well‐being [2].
The pathophysiology of rosacea continues to remain unclear, but it is believed that genetic factors, immune system dysregulation, abnormal neurovascular signaling, and dysbiosis of commensal skin organisms may be the key promoters of rosacea [3].
The prevalence of rosacea seems to be higher in fair‐skinned individuals with I or II Fitzpatrick skin types and Northern and Eastern European descent [2], but the disease has also been identified in other ethnicities [4], and the onset of rosacea usually ranges between 30 and 50 years of age [2]. Classically, rosacea has been believed to predominate in women, but recent studies suggest that this female predominance might not be as important as previously thought.
Risk Factors and Triggers
Based on the epidemiological data available and the surveys conducted by the National Rosacea Society, some important risk factors for the development of rosacea such as genetic predisposition, age, skin phototype, female gender, and history of flushing, have been identified [5].
There are many external factors believed to trigger or to exacerbate rosacea, including ultraviolet exposure, hot or cold temperatures, spicy food, stress, hot drinks, or alcohol [6, 7], but internal contributors, such as pharmacological, infectious, immunological, and endocrinological disturbances have also been proposed as promoters or aggravating factors for rosacea [8, 9].
Current data suggest that some trigger factors, like UV radiation, extreme temperatures, spicy food, and skin colonization with Demodex folliculorum modulate Toll‐receptor like (TLR) signaling, while also inducing reactive oxygen species (ROS), stimulating neuropeptide production [10–15].
Internal contributors might be pilosebaceous unit abnormalities, abnormal vascular reactivity, dysregulation of the innate immune system, high ROS levels, increased serine protease or matrix metalloproteinase (MMP) activity, Demodex, or small intestinal bacterial overgrowth (SIBO) [15–18].
Quality of Life
Since its first description hundreds of years ago, rosacea has also been named “the curse of the Celts,” emphasizing its high prevalence among individuals with Northern‐European heritage [19] and its association with alcohol consumption, lack of refinement, unhealthy lifestyle, psychiatric illness, and inappropriate behavior. Historically, these misconceptions made facial erythema an important handicap on social relationships and a major cause for stigmatization [20, 21].
It as a well‐known fact that this common, yet often underdiagnosed condition has the ability to influence personal, social, and professional aspects of patients’ lives [22] and, if left untreated, can have serious psychosocial consequences, inducing emotional distress and social anxiety avoidance behavior [6].
In addition, psychodermatological literature links rosacea to depression, body dysmorphic disorders, low self‐esteem, sexual dysfunction, and reduced quality of life (QoL) in general.
Studies have shown that 70% of rosacea patients experience feelings of embarrassment, 75% low self‐esteem, and most of them are frustrated about their disease; all of these feelings potentially lead to social and professional isolation [22].
Associated Diseases
In the past few years it has become more and more obvious that rosacea might be associated with systemic diseases in a direct relation with the severity of the skin symptoms [23].
Three HLA alleles (major histocompatibility complex –MHC– class II), HLA‐DRB1, HLA‐DQB1, and HLA‐DQA1, known to be associated with type I diabetes, retinopathy (vascular proliferation), and celiac disease have also been linked with rosacea [24].
Cardiovascular Diseases
Rosacea patients have been shown to have a higher prevalence of cardiovascular risk factors, such as dyslipidemia, hypertension, and coronary artery disease, compared to healthy controls [23, 25, 26], in a disease severity‐dependent manner [23]. This association could be explained by the over‐expression of cathelicidins and lower levels of high‐density lipoprotein paraoxonase‐1, found in rosacea, atherosclerosis, and dyslipidemia respectively [26].
Metabolic Diseases
Recent studies revealed that rosacea and type I diabetes mellitus share a genetic locus [24, 27] and that rosacea patients might suffer from insulin resistance and higher fasting blood glucose levels [3, 28].
Digestive Diseases
Another interesting connection has been established between rosacea and the digestive system via the HLA‐DRA locus which has been associated with rosacea and inflammatory bowel diseases (IBD) including ulcerative colitis, Crohn’s disease, and celiac disease [3, 24].
A Danish population‐based cohort study revealed that this population group presents higher prevalence rates of celiac disease, Crohn’s disease, ulcerative colitis, Helicobacter pylori infection (HPI), SIBO, and irritable bowel syndrome compared to healthy subjects [29].
Neurological Diseases
Patients with rosacea have also been found to have significantly increased risk of neurological disorders such as migraine, depression, complex regional pain syndrome, Alzheimer’s disease and Parkinson’s disease, and glioma [330–33]. The common link between rosacea and neurological disorders seems to be enhanced expression of matrix metalloproteinase (MMP) [31].
Depression and Anxiety
Psychological factors are considered potential triggers for rosacea, and studies have also shown that rosacea is associated with higher rates of depression and anxiety in a disease severity‐dependent manner [34].
Autoimmunity
The relationship between rosacea and autoimmune disorders is sustained by the higher prevalence of celiac disease, multiple sclerosis, and rheumatoid arthritis in rosacea patients [27].
Pathogenesis
The pathogenesis of rosacea is still not completely understood. Two main mechanisms are considered to be implicated in this disease: immune system and neurovascular abnormalities [35]. But other factors, such as dermal matrix degeneration, pilosebaceous unit abnormalities, and infectious agents might also be implicated [3].
Inflammation is believed to be one of the most important factors of rosacea pathogeny. Both the innate and the adaptive immunity seem to be implicated in the development of the lesions [3]. The main factors involved in the promotion of inflammation are the toll‐like receptors, the antimicrobial peptides, and different enzymes [35].
The inflammatory lesions of rosacea have been shown to present elevated serine protease activity and cathelicidin‐derived peptides [36], but also higher levels of neuropeptides, which may be involved in the induction and maintenance of inflammation [35]. One of the main sources of cathelicidin‐derived peptides are the mast cells, which also act as key mediators of inflammation in rosacea [37].
Rosacea could be considered a vascular disorder because of its association with erythema and telangiectasia, which are also promoted by mast cells through a complex process finally leading to vasodilatation, angiogenesis, and fibrosis [35]. The correlation between facial erythema and emotional stress has led researchers to think that the nervous system is another pathogenic factor for rosacea [38].
Other possible contributors to rosacea pathology are microbial agents and amongst them, D. folliculorum mites play a central role. Different bacteria acting as residences for Demodex mites might also be implicated in rosacea’s pathogeny. Amongst them, Bacillus oleronius and its products could be related to rosacea by stimulating the production of proinflammatory mediators and chemotaxy. Other Bacillus species, such as Bacillus cereus have been identified in association with D. folliculorum in rosacea‐affected skin and they seem to be associated with reactive enzyme production and tissue destruction [39].
Another proposed contributing factor in rosacea pathogeny is the epidermal barrier disruption which sustains the association between rosacea and sensitive skin. Demodex mites feed themselves with sebum and keratinocytes, and they can additionally disrupt the skin barrier, leading to hypersensitivity [3].
Clinical Variants
Rosacea comprises multiple signs and symptoms [40]. The National Rosacea Society Expert Committee (NRSEC) has defined the clinical diagnostic criteria for rosacea, classifying them into primary and secondary features. Flushing, telangiectasia, permanent erythema, papules, and pustules are considered primary rosacea features, while the presence of plaques, edema, dry appearance, ocular manifestations, burning or stinging sensations, and phymatous lesions are classified as secondary manifestations. A clinical diagnosis of rosacea is sustained by the presence of one or more primary features located in central areas of the face.
Based on the characteristic signs and symptoms, rosacea has been classified into four subtypes: erythematotelangiectatic, papulopustular, phymatous, and ocular.
The first subtype, erythematotelangiectatic, is characterized by flushing, permanent erythema, and telagiectasia located on the convex areas of the face, accompanied by sensations of burning or stinging [41, 42].
Papulopustular rosacea comprises features such as facial papules and pustules on an erythematotelagiectatic background [41], predominantly found in middle‐aged women (Figure 5.1).

Figure 5.1 Clinical Aspect of Rosacea.
The phymatous subtype is more common in men and affects predominantly the nose (rhynophyma). Other locations affected by such fibrous, hypertrophic changes are the chin (gnatophyma), forehead (metophyma), eyelids (blerapharophyma), or ears (otophyma) [41].
Ocular rosacea is characterized by a wide spectrum of symptoms ranging from sensations of dryness, foreign body, irritation to inflammatory keratitis, chalazion, hordeolum, corneal ulcers or scars and, in extremely rare instances, blindness [41].
Most patients experience characteristic lesions of more than just one subtype at a time with different severity levels, while others progress from one subtype to another in succession.
Imagistic Approach
Several bioengineering techniques, such as scanning laser doppler, video microscopy, measurement techniques for skin surface temperature, pH, colorimetry, and digital photography can be utilized to assess rosacea’s signs and symptoms (Figure 5.2) and also to monitor treatment results (Figures 5.4 and 5.5).
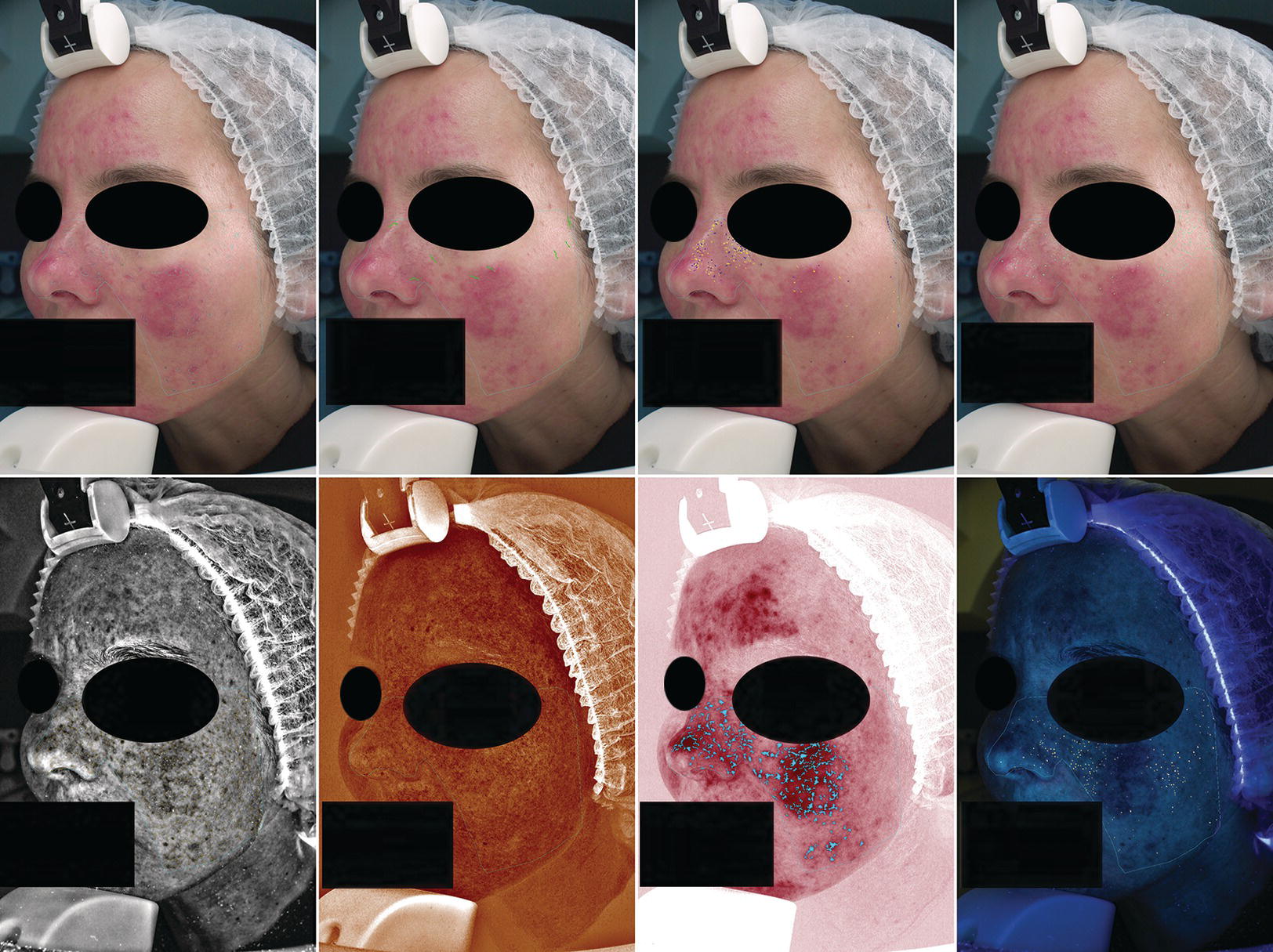
Figure 5.2 Noninvasive evaluation.
The amount of hemoglobin in the blood vessels of the papillary dermis determines the degree of cutaneous erythema. A useful tool to quantify erythema is skin reflectance spectrophotometry, an efficient way to measure changes in cutaneous vasculature [43] (Figure 5.3).
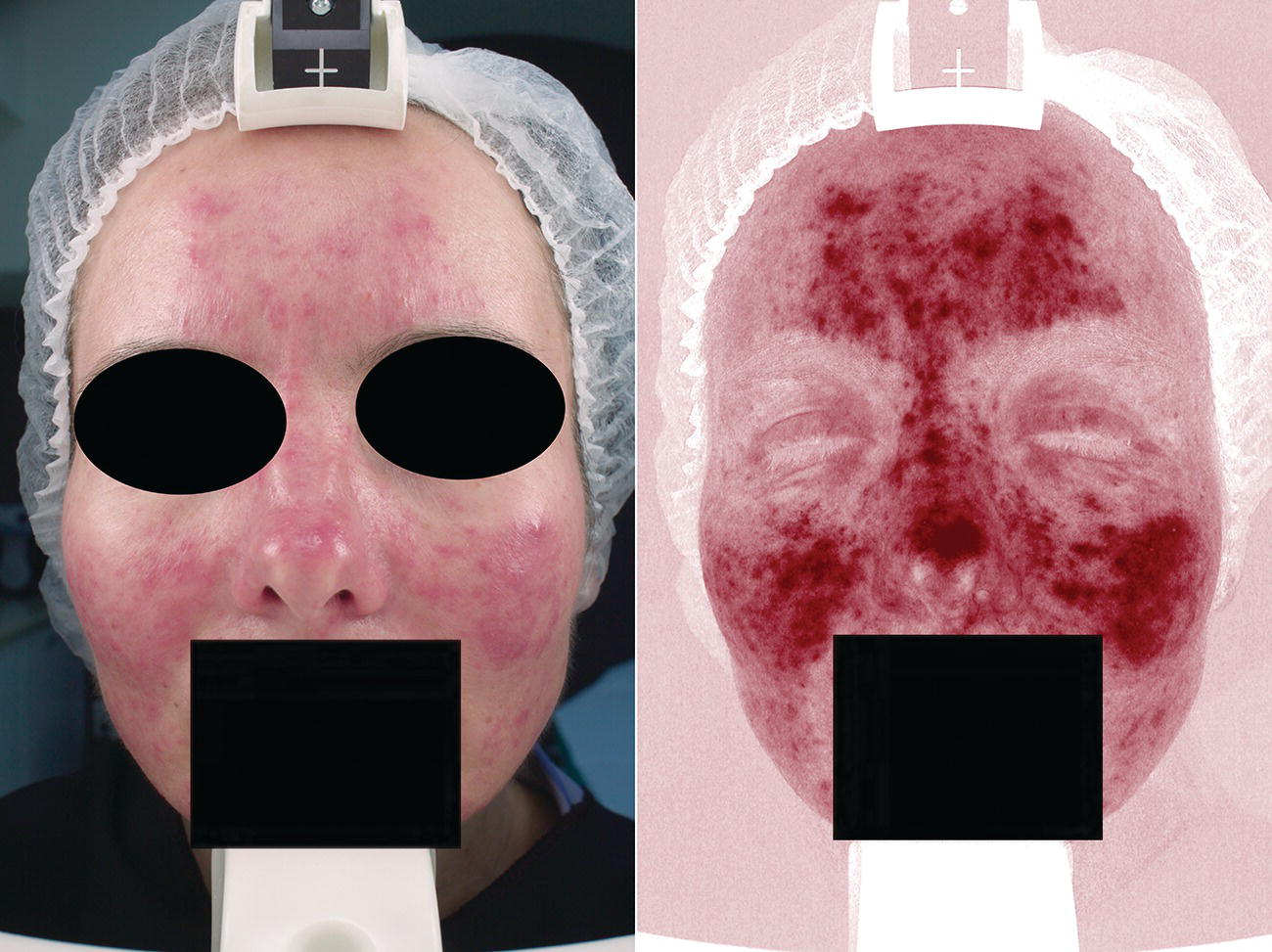
Figure 5.3 Correlation clinical lesions with vascular modifications.
The initial non‐invasive evaluation of patients with rosacea facilitates the possibility to administer an individualized treatment and delivers better treatment results. [44]
Approach
Rosacea is a chronic condition characterized by exacerbation and remission periods and a sensitive skin type [40]. Currently, there is no curable treatment for this condition and most management strategies rely on lifelong symptomatic therapies that must be effective, safe, and well tolerated. Basic rosacea care could be defined as the triad of patient education, appropriate skin care, and effective treatment [40].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree