Chapter 3 Risk and Gender Factors for Noncontact Anterior Cruciate Ligament Injury
Environmental Risk Factors
Certain studies have examined surface conditions relating to ACL injuries. Olsen et al1 and Torg et al2 both studied team handball and found an increased risk of ACL injury while playing on synthetic floors versus traditional parquet floors. Both believed that the increased friction of synthetic flooring was the cause. Orchard et al,3 Heidt et al,4 and Scranton et al5 all reported higher rainfall and cooler temperatures were related to decreased ACL injuries and theorized that dry, hot weather conditions promote increased frictional forces on the playing field, thus in turn resulting in increased injury rates.
Lambson et al6 in a 3-year prospective study looked at footwear to evaluate torsional resistance of modern football cleats. They compared four styles of football shoes and found that the edge design, a design having longer irregular cleats at the periphery and many smaller cleats interiorly, was associated with higher ACL injury rates.
Bracing Pros and Cons
Prophylactic and functional (postreconstructive) knee bracing has long been a controversial subject. Over the past 20 years, attitudes have fluctuated regarding the effectiveness of braces in preventing knee injury in the uninjured athlete, the ACL deficient athlete, and the ACL reconstructed athlete. A study by Decoster and Vailas7 on brace prescriptions patterns noted that there has been a decreasing tendency for orthopaedic surgeons to prescribe ACL braces. The authors also noted that a primary factor influencing brace prescription by orthopaedists was the activity level of the patient.7
Early studies on prophylactic brace wear by Teitz et al8 and Rovere et al9 indicated no benefit to brace wear. These authors cited increased rates of knee injury in some athletes using prophylactic knee braces. In contrast, two other studies—the West Point study by Sitler et al10 involving 1396 cadets at the U.S. Military Academy who played intramural tackle football and the Big Ten Conference study by Albright et al11 involving 987 NCAA football players—concluded that prophylactic knee braces were effective in reducing injury. Since these studies, there has been a paucity of data to support prophylactic bracing for ACL injury protection, but it is believed that braces may provide some advantage to reducing medial collateral ligament (MCL) injury.12,13
Braces are commonly prescribed following ACL injury or reconstruction; however, little evidence supports their physiological or biomechanical efficacy. In a prospective randomized clinical trial of functional bracing for ACL deficient athletes, Swirtun et al14 found that subjectively, patients had initial sense of increased stability, but these investigators were unable to find objective benefits. In contrast, Kocher et al studied the use of braces to prevent reinjury in 180 ACL deficient alpine skiers and found reinjury occurred in 2% of the braced skiers compared with 13% of the unbraced “control” skiers.15
Risberg et al investigated the effect of knee bracing after ACL reconstruction in a prospective clinical trial of 60 patients randomized postoperatively (30 braced and 30 without brace) with 2 years of follow-up.16 They found no evidence that bracing affected knee joint laxity, range of motion, muscle strength, functional knee tests, patient satisfaction, or pain in braced athletes compared with athletes who did not use a brace following ACL reconstruction. Furthermore, they found prolonged bracing, which they defined as brace wear 1 to 2 years postoperatively, produced decreases in quadriceps muscle strength. McDevitt et al in a prospective, randomized multicenter study of 100 subjects likewise found no significant differences between braced and nonbraced subjects following ACL reconstruction.17
It has been theorized that damage to the ACL can disrupt mechanoreceptors in the knee leading to decreased proprioception.18 Birmingham et al19 has suggested that brace wear may help to correct this deficit somewhat, but benefits do not carry over to more demanding tasks. To examine knee proprioception, researchers have studied the threshold for detection of passive knee motion and found that brace application to the ACL deficient limb does not improve the threshold to detect passive range of motion.20,21
Anatomical Risk Factors
Association Between Q Angle and Injury Risk
The Q angle, which typically ranges from 12 to 15 degrees, is formed by the intersection of two lines, one from the anterior superior iliac spine to the midpoint of the patella and another from the tibial tubercle to the same reference point on the patella. It has been proposed that an increased Q angle may be associated with an increased risk for knee injury because excessive lateral forces could negatively influence the knee’s mechanical alignment.22,23
Females have been reported to have larger Q angles than their male counterparts24,25; however, in a trigonometric evaluation, Grelsamer et al reported a mean difference of only 2.3 degrees between the Q angles of men and women and furthermore found that men and women of equal height demonstrated similar Q angles.26 Shambaugh et al25 studied the relationship between lower extremity alignment and injury rates in recreational basketball players and found larger Q angles in athletes who sustained knee injures. In contrast, other authors have not been able to relate injury to Q angle.22,27,28 Guerra et al29 reported that quadriceps contraction alters Q angle measurements, thus making it difficult to establish a direct link between static Q angle measurements and injury.
Notch Width as a Risk Factor
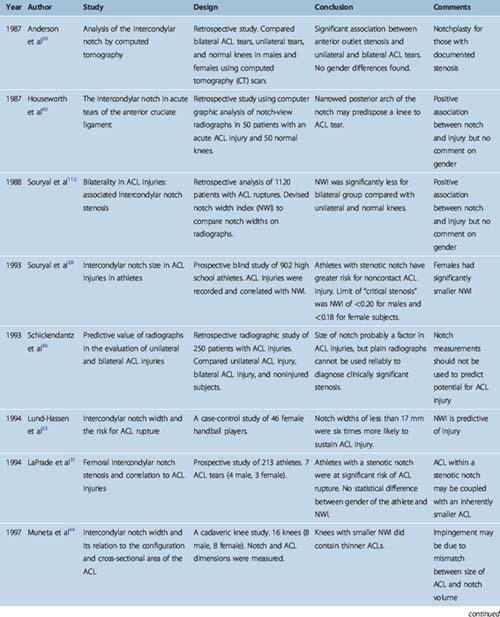
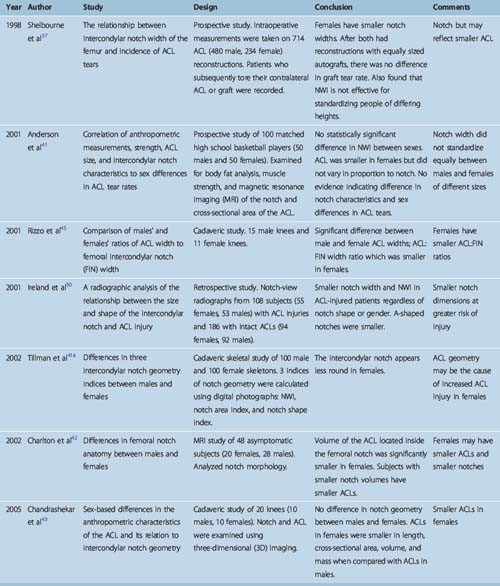
Structural characteristics of the distal femur and femoral intercondylar notch as well as ACL geometry and the ACL relationship to the intercondylar notch have been implicated as anthropometric factors associated with ACL injury rate disparity between males and females. It has been postulated that a smaller notch, termed notch stenosis, may cause impingement to the ACL and put it at increased risk of injury, or possibly a smaller notch may imply a smaller ACL leading to decreased load to failure. Although these factors have been heavily studied using plain radiography,30–38 computed tomography (CT),39,40 magnetic resonance imaging (MRI),41,42 and cadaveric43–45 and in vitro37 analysis, a lack of consistent measurement techniques and findings has made it difficult to interpret results. Therefore there is still no consensus relating morphology of the intercondylar notch to ACL injury rates. A chronological summary of the data is listed in Table 3-1.
Hormonal Risk Factors
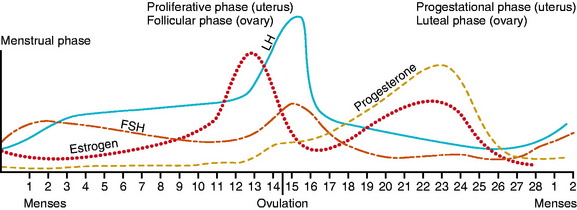
The increased incidence of ACL injury in women compared with men has raised interest regarding the influence of sex hormones on injury occurrence. Fig. 3-1 describes the menstrual cycle. A normal cycle is typically 28 to 30 days. The follicular phase (i.e., the stage of the follicle development) begins with menstruation and ends with ovulation. The latter lasts approximately 3 to 5 days and, if pregnancy does not occur, is followed by the luteal phase, which begins with the involution of the follicle and formation of the corpus luteum. Estradiol secretion is biphasic, peaking in both the follicular and luteal stages. Progesterone is produced by the corpus luteum and therefore occurs in the luteal phase only.
Monthly Distribution of Anterior Cruciate Ligament Injuries
Initial surveys of injury occurrence throughout the monthly menstrual cycle revealed that injuries were not equally distributed throughout the cycle but instead were clustered either around menstruation or the ovulation period of the cycle.46–48
However, the reliability of these early data was questioned because subjects were not frequently controlled for the use of birth control pills and hormonal assays were not done to verify cycle times; instead, athletes recalled or reported their menstrual history. Repeated studies using radioimmunoassays on serum, urine, or saliva verified the non–chance distribution of ACL injuries throughout the menstrual cycle.48–51
Sex Hormones and Laxity
If sex hormone levels do influence injury rates, how this occurs is not clear. Multiple studies in the past decade have focused on the influence of sex hormones on knee laxity, and some investigators have even correlated female sex hormone levels and laxity measures with menstrual cycle phase. In 1999, Wojtys and Huston52 reported on a series-controlled study of 12 females and 12 males, in which they found a decrease in knee laxity on day 12 of the monthly menstrual cycle in women versus no monthly variation in knee laxity in men.
In the following year, however, Belanger et al53reported no significant difference in anterior knee laxity throughout the monthly cycle in 18 Brown University athletes studied over 10 weeks. Similarly, Karageanes et al54 reported no significant changes in ACL laxity from the follicular to luteal phases. This research group measured laxity before workouts in 26 athletes, comparing these data to self-charted menstrual cycles. Van Lunen et al,55 using a within-subjects linear model, reported on 12 females tested for knee laxity at the onset of menses, near ovulation, and on day 23 with hormonal assays performed on blood drawn on those same days. They found no association between follicular, ovulatory, or luteal phase hormone concentrations and ACL laxity measures.
This is in contrast to an earlier study by Heitz et al,56 who not only compared laxity measures taken on days 1, 10, 11, 12, 13, 20, 21, 22, and 23 of a self-reported menstrual cycle but also compared these data with serum estradiol and progesterone levels as measured by immunoassays in seven active females who reported normal 28- to 30-day menstrual cycles. These investigators found a significant difference in anterior knee laxity when comparing laxity measures at baseline estrogen levels with peak levels of estrogen and when comparing laxity at baseline progesterone levels with that of peak progesterone levels. These results are similar to a series-controlled Japanese study57 involving 16 women and 8 men, which found no statistical difference in anterior displacement over time in men but did find variation in anterior knee laxity in women between the follicular and ovulatory phases and between the follicular and luteal phases at 89N displacement. Furthermore, Shultz et al58 obtained daily knee laxity measures as well as assayed daily serum samples for estradiol, progesterone, and testosterone in 25 females throughout one complete menstrual cycle and concluded that changes in sex hormones mediated changes in knee laxity across the menstrual cycle. Moreover, these investigators found a variable knee laxity response among females, with some females experiencing significant variation in knee laxity across the monthly cycle and others experiencing very little.
Even if an association can be demonstrated among sex hormones, menstrual phase, and increased laxity, an increase in knee laxity has not been reliably associated with an increased risk of ACL injury.59–62
Sex Hormones and Ligament Biology
Female sex hormones have been found in animal and human studies to have a direct effect on growth and development of bone, muscle, and connective tissue. In 1996, Liu et al63 reported receptor sites for estrogen and progesterone in the human ACL, and in 2005, Lovering and Romani reported androgen receptors in the female ACL as well, suggesting that these sex hormones could have a direct effect on the structure and composition of the ACL.64
In fact, in 1997, Liu et al reported a significant reduction in procollagen synthesis by ACL fibroblasts and in fibroblast proliferation with increasing estradiol concentrations.65 Similarly, Slauterbeck et al66 found that high-dose 17β-estradiol significantly decreased the tensile strength of the ACL in ovariectomized rabbits compared with the tensile strength of the ACL in ovariectomized rabbits not supplemented with estrogen. Seneviratne et al67 reported that despite the presence of estrogen receptors on ovine ACL fibroblasts, there was no significant difference in ACL fibroblast proliferation or collagen synthesis when cells in culture were exposed to 17β-estradiol at physiological concentrations. In 2003, Strickland et al,68
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree