Chapter 15 The Central Quadriceps Free Tendon for Anterior Cruciate Ligament Reconstruction
Introduction
The central quadriceps has been used for anterior cruciate ligament reconstruction (ACLR) for more than 25 years.1,2 Stability results are similar to those with other autograft alternatives, but patients experience less pain and reach rehabilitation landmarks sooner.3 Staubli et al4,5 have studied the anatomy and biomechanical properties of the quadriceps tendon. We became interested in this ACL graft in the early 1990s, first using it with bone6 but later discovering that it is a desirable free tendon graft option7 for ACLR. We wanted to avoid the risk of postoperative problems noted with bone–tendon–bone–patella tendon graft harvest,8,9 were concerned about subtle weakness after taking out the medial hamstring tendons for ACLR in young athletes,10 and continue to worry about the possibility of prions in allograft tissue. We wanted to avoid these risks by using the central quadriceps free tendon (CQFT) for our ACLR. We confirmed and later reported the strength of the quadriceps tendon after harvesting the graft.11 Our experience has remained very positive as we begin our 10th year with the CQFT graft. Also, patients frequently come into our office impressed with how little postoperative pain and difficulty they have compared with bone–tendon–bone and hamstring ACLR patients they encounter in physical therapy, as noted by Joseph et al3 in their short-term recovery study of ACLR patients.
Technique
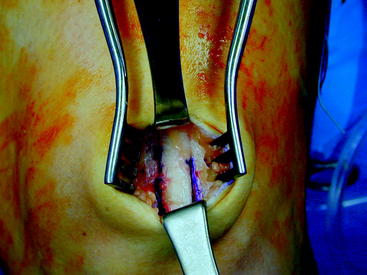
To harvest the CQFT, make a short 1.5- to 2-inch incision from the mid proximal patella upward (Fig. 15-1), and retract to view the quadriceps tendon. Retract slightly medially and note the vastus medialis obliquus (VMO). The graft should be taken preferentially from the thicker medial part of the quadriceps tendon but started proximally by retracting upward to the proximal VMO where the first incision is placed. Use a #10 scalpel blade and draw it distally at a 6- to 7-mm depth (just slightly less than the breadth of a #10 blade). The medial border of the graft then will usually be about 5 to 8 mm from the VMO at the level of the proximal patella.
Grasp the released end of the quadriceps tendon with a uterine T clamp, and further dissect it proximally using a combination of blunt stripping and careful sharp dissection. We usually place two whipstitches12 with at least one Fiberwire (Arthrex, Naples, FL) in the released end and use this for traction during the dissection.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree