What are the three primary goals in treating the rheumatoid hand?
PRC:
1. Pain relief.
2. Restoration of function.
3. Cosmetic improvement of the hand.
 What are the three basic principles in rheumatoid hand surgery?
What are the three basic principles in rheumatoid hand surgery?
1. Synovectomy/soft-tissue reconstruction done early in disease.
2. Highly erosive disease (arthritis mutilans) treated early with fusion before bone loss.
3. Correction of deformity that causes loss of motion and may severely compromise hand function.
 What surgical sequence should be followed in a rheumatoid patient?
What surgical sequence should be followed in a rheumatoid patient?
1. Lower extremity addressed first.
2. Proximal joints before distal joints (e.g., elbow before wrist, wrist before metacarpophalangeal joint [MCPJ] and proximal interphalangeal joint [PIPJ]).
 What is an essential part of the preoperative evaluation in a rheumatoid patient?
What is an essential part of the preoperative evaluation in a rheumatoid patient?
Cervical spine evaluation. 25% to 50% of patients can have atlantoaxial instability (plain cervical radiographs including flexion and extension views are standard).
 What is the pathogenesis in rheumatoid arthritis (RA) of the hand?
What is the pathogenesis in rheumatoid arthritis (RA) of the hand?
Autoimmune disorder resulting in erosive synovitis of the hand and wrist secondary to injury to synovial microvascular endothelial cells triggering an inflammatory reaction causing influx of polymorphonuclear leukocytes (PMNs), monocytes, and macrophages.
 Inflammatory cells/mediators produced by macrophages, monocytes, PMNs stimulate which cell type in the rheumatoid hand?
Inflammatory cells/mediators produced by macrophages, monocytes, PMNs stimulate which cell type in the rheumatoid hand?
Osteoclast. These are responsible for subchondral osteopenia.
 What three classes of drugs are used to treat RA medically?
What three classes of drugs are used to treat RA medically?
Nonsteroidal anti-inflammatory agents (NSAIDs), corticosteroids, and disease-modifying anti-rheumatic drugs (DMARDs).
 Which of these medications can help to change the disease course?
Which of these medications can help to change the disease course?
Only DMARDs are found to alter the course of RA and improve associated radiographic outcomes. They have both anti-inflammatory effects as well as structural-modifying properties.1,2
 What are the two classes of biologic agents that exist to treat RA?
What are the two classes of biologic agents that exist to treat RA?
Tumor necrosis factor (TNF) inhibitors and interleukin-1 (IL-1) receptor antagonists. These agents act to neutralize cytokines that mediate the inflammatory pathogenesis in RA.1
 What are the extra-articular manifestations seen in RA? Which one is most common?
What are the extra-articular manifestations seen in RA? Which one is most common?
Vasculitis, pericarditis, pulmonary nodules, episcleritis, and subcutaneous nodules. Subcutaneous nodules (25% of patients with RA).
 Manifestation of accumulated inflammatory cells around capillaries of the synovium and tenosynovium is known as:
Manifestation of accumulated inflammatory cells around capillaries of the synovium and tenosynovium is known as:
Synovitis and tenosynovitis.
 What cellular processes are responsible for cartilage damage in RA?
What cellular processes are responsible for cartilage damage in RA?
Cytokine-activated neutrophils release lysosomal enzymes and free oxygen radicals, which destroy cartilage in the affected joint.3
 Is pattern of joint involvement in RA different from osteoarthritis (OA) of the hand?
Is pattern of joint involvement in RA different from osteoarthritis (OA) of the hand?
Yes. In RA, MCPJ and PIPJ are commonly involved. In OA, distal interphalangeal joint and basilar joint of thumb are involved.
 What are Bouchard’s nodes?
What are Bouchard’s nodes?
Enlargement of PIPJ seen mainly in RA. **Heberden’s nodes are seen in OA and refer to DIP enlargement.
 What is the most commonly affected joint in RA?
What is the most commonly affected joint in RA?
The wrist.4
 What is the most frequently affected area about the wrist in RA patients?
What is the most frequently affected area about the wrist in RA patients?
Distal radioulnar joint (DRUJ).
 Why is the DRUJ affected early in the disease course?
Why is the DRUJ affected early in the disease course?
There is a greater degree of vascularity at the prestyloid recess of the distal ulna, which allows for early synovial infiltration.3
 What are other commonly affected areas of the wrist in RA?
What are other commonly affected areas of the wrist in RA?
Palmar side of distal radius, waist of scaphoid, triquetrum.3
 What is the typical presentation of RA early in the disease?
What is the typical presentation of RA early in the disease?
Insidious onset of morning stiffness and polyarthropathy involving most commonly the hands and feet.
 Decreased active digital flexion in a patient with RA is usually caused by what?
Decreased active digital flexion in a patient with RA is usually caused by what?
Synovial nodules within flexor tendons. These nodules within retinacular system reduce active flexion of finger.
 What is the natural course of rheumatoid disease with articular involvement at the MCPJ?
What is the natural course of rheumatoid disease with articular involvement at the MCPJ?
Progressive joint erosion and collapse with palmar displacement.
 How do tendon ruptures of the hand and wrist occur in patient with RA?
How do tendon ruptures of the hand and wrist occur in patient with RA?
By attrition (abrasion over bony prominences), infiltration (synovitis), and ischemia (external pressure by compressive synovium).
 What is the more common direction of sagittal band rupture in RA?
What is the more common direction of sagittal band rupture in RA?
Radial sagittal band, results in ulnar displacement of the extensor tendons.
 How is the wrist affected in patients with RA?
How is the wrist affected in patients with RA?
Synovitis begins in ulnar aspect of the wrist with the DRUJ and radiocarpal joint first affected, usually sparing the midcarpal joint. Erosive changes seen at the prestyloid recess of the ulnar styloid, sigmoid notch of radius, insertion of radioscapholunate ligament, and the scaphoid waist. The carpus subluxes ulnarly and volarly with supination relative to radius. This carpal alignment leads to radial deviation of the metacarpals.
 What is the natural course of wrist deformities with rheumatoid disease?
What is the natural course of wrist deformities with rheumatoid disease?
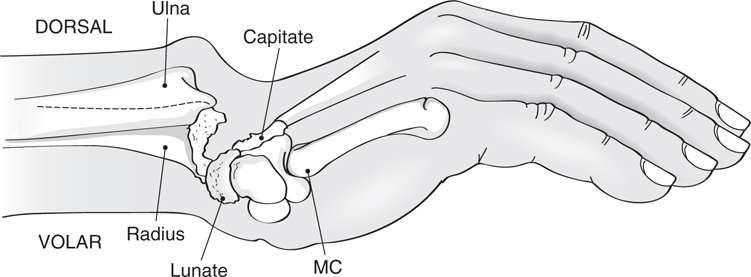
Supination, palmar dislocation, radial deviation, and volar–ulnar dislocation of the carpus on the radius (see Fig. 38-1).
Figure 38-1 Natural course of wrist deformities with rheumatoid disease.
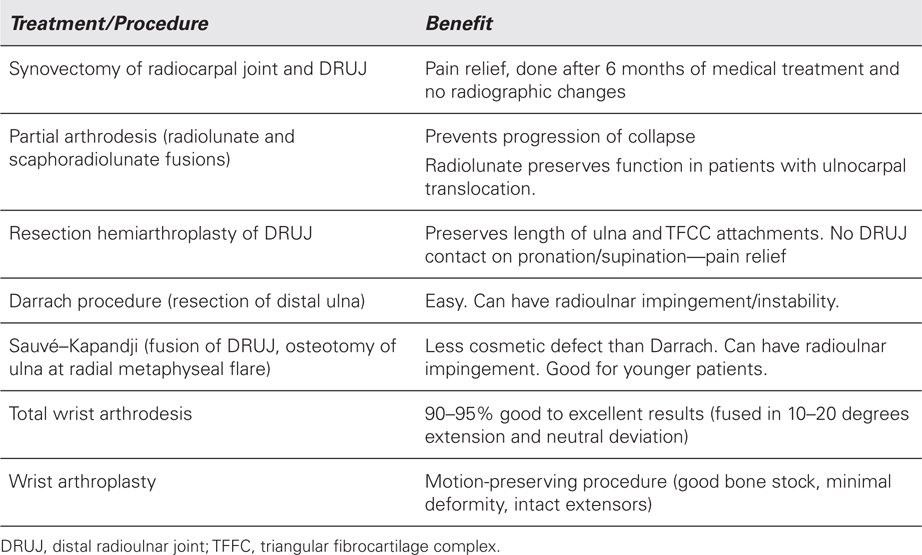
 What are the treatment options available for the rheumatoid DRUJ/wrist?
What are the treatment options available for the rheumatoid DRUJ/wrist?
 What is the total wrist arthroplasty experience in the United States?
What is the total wrist arthroplasty experience in the United States?
1. 1967: Swanson. Silicone hinge.
2. 1972: Meuli. Ball and trunnion.
3. 1973: Volz. Dorsopalmar tracking.
4. 1977: Figgie and Ranawat. Trispherical (hinge).
5. 1982: Beckenbaugh. Biaxial (ellipsoidal).
6. 1990: Mennon. Universal (anatomic).
7. 2002: Adams. Universal 2 (uncemented).
 What are current accepted indications for total wrist arthroplasty?
What are current accepted indications for total wrist arthroplasty?
1. Painful pancarpal (diffuse) and advance arthritis.
2. Progressive deformity with advanced arthritis.
3. Patients who do not use walking aids with affected hand.
4. Other joints of same extremity have significant limitations.
5. Personal factors (low-demand activities that require wrist motion).
6. Contralateral wrist fused.
 What are current accepted contraindications for total wrist arthroplasty?
What are current accepted contraindications for total wrist arthroplasty?
1. Previous sepsis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree