RHEUMATOID ARTHRITIS
I. GENERAL CONSIDERATIONS
A. Definition: Inflammatory arthritis characterized by morning stiffness, subcutaneous nodules, and laboratory abnormalities (+ rheumatoid factor in 70%).
B. Affects 6% of women and 2% of men of European ancestry
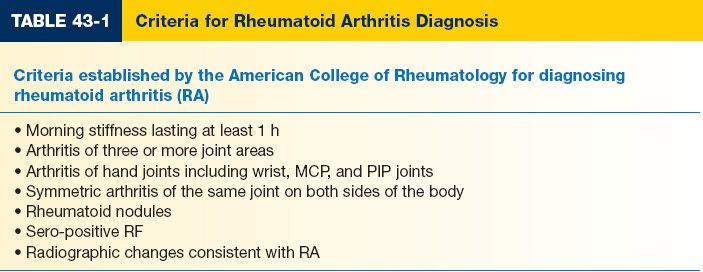
C. Diagnosis (Table 43-1)
D. Typically involves: C-spine, shoulders, elbows, hands, hips, knees, and feet
E. Pathophysiology
1. Inflamed synovium (pannus) invades and destroys articular cartilage as well as tendons.
2. Bone and cartilage destruction from synovial enzymes and inflammatory cells.
3. Tissue ischemia from direct invasion into terminal vessels or mass effect of hypertrophic synovium.
4. Tendon destruction from direct invasion as well as from ischemia (tendon central necrosis).
5. Rheumatoid nodule: Necrotic material (ischemia or trauma) surrounded by inflammatory cells in granulomatous reaction.
F. Stages of rheumatoid joint involvement
1. Stage I: Synovitis without deformity
2. Stage II: Synovitis with passively correctable deformity
3. Stage III: Fixed deformity without joint changes
4. Stage IV: Articular destruction
G. Female to male ratio is 3:1
H. Treatment goals: Control synovitis, maintain joint function, and prevent deformity
I. Priorities for hand surgery in rheumatoid patients are
1. Alleviation of pain: Alleviation of medically refractory pain is primary indication for surgery.
2. Improvement of function
a. Loss of function is not synonymous with deformity
b. Surgery cannot restore full function and may further weaken hand.
c. Reconstruction before inset of severe deformity may offer better results.
3. Retardation of progression
a. Earlier reconstruction/procedure with more predictable outcome is preferable
b. Tenosynovectomy may prevent tendon rupture
c. Wrist stabilization and distal ulna excision to prevent wrist collapse
4. Improvement of appearance: Surgery to correct deformity should be avoided in patients with minimal functional loss or pain, as patient may adapt to function with such deformity.
J. Treatment overview
1. Maximize medical management: The patient should usually be under the care of a rheumatologist for at least 6 months before considering an operation.
2. PT and OT: Critical to help with preoperative preparation and postoperative recovery.
______________
*Denotes common in-service examination topics
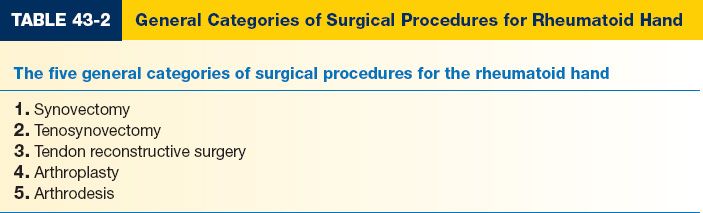
3. Surgery (Table 43-2)
a. Can be prophylactic, not just for late complications.
b. Need to coordinate timing with the rheumatologist; maximize medical control.
c. Preoperative cervical spine evaluation is essential.
d. Generally, address joints from proximal to distal.
II. HAND FINDINGS
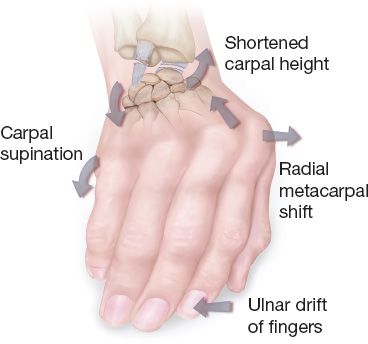
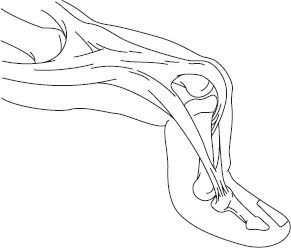
A. Physical examination (Fig. 43-1)
1. Ulnar drift at metacarpophalangeal (MP) joint
2. Caput ulna
Figure 43-1. Rheumatoid arthritis changes at the wrist. Volar and ulnar translation of the wrist with progressive supination occurs as the restraining ligaments are successively disrupted.
3. Swan-neck and boutonniere deformities
4. Tendon ruptures
5. Thumb deformities
6. Radiocarpal collapse
B. X-ray changes: Periarticular erosions and osteopenia
III. TENOSYNOVITIS
A. Background
1. Tenosynovitis is common with 50% to 70% of RA patients developing tendon sheath inflammation.
2. May occur before joint involvement
3. Common sites of involvement are dorsal wrist, volar wrist, and volar aspect of digits.
4. May lead to pain, tendon dysfunction, compressive neuropathy, and tendon rupture.
B. Dorsal wrist tenosynovitis
1. Often obvious as painless swelling due to the thin dorsal wrist skin
2. May involve one, some or all tendons in all compartments
3. Tendon ruptures frequent from invasion by hypertrophic synovium and attrition.
4. Although remission may occur from conservative therapy (rest, steroid injection, and anti-rheumatoid agents), early dorsal tenosynovectomy is suggested
a. Remission unlikely if proliferative synovitis progresses
b. Lack of improvement after 4 to 6 months of medical management
5. Dorsal tenosynovectomy treatment of choice
C. Volar wrist tenosynovitis
1. Hypertrophic tenosynovitis often less obvious than dorsal disease.
2. Usually leads to restriction of flexor tendons leading to restricted active and passive motion.
3. Compression of median nerve may occur
4. Again, early surgical treatment is indicated to prevent permanent damage.
5. Volar tenosynovectomy with carpal tunnel decompression is treatment of choice.
D. Digital tenosynovitis
1. Mild synovial hypertrophy can affect function as tendons travel in a tight fibro-osseous canal.
2. Rheumatoid nodule in digital tendons can cause trigger finger
3. Prolonged tenosynovitis may lead to tendon rupture
4. Flexor tenosynovectomy and excision of flexor tendon nodules are indicated
IV. ULNAR DRIFT AT MP JOINT
A. Mechanism of deformity
1. Condylar joints (allow biplanar movements) inherently less stable. Further destabilization by rheumatoid destruction allows normal and abnormal forces in hand to deform joints.
2. Synovitis at the MP joint causes capsule, ligament, and volar plate laxity
3. Radial sagittal band laxity causes ulnar deviation of the extensor tendons
4. Contraction of the ulnar intrinsics
5. Radial deviation of the wrist and metacarpals alters the direction of pull of the extensor tendons.
B. Treatment depends on degree of joint destruction
1. Address the wrist first
2. If no joint destruction: Synovectomy, soft tissue realignment, and ulnar intrinsic release
a. Infrequently indicated due to recurrence and effectiveness of MP arthroplasty
b. Indicated for persistent synovitis with early volar subluxation and ulnar drift or young patients with slowly progressing disease.
c. Extensor relocation indicated in patient with dislocated tendons but otherwise functional extensor and joint.
3. If joint destruction: Good results with MP implant arthroplasty (i.e., Swanson silicone implants) or fusion
a. Indicated for severe disease with MP dislocation, ulna drift, and articular involvement.
b. Soft tissue destruction and abnormalities make an ideal arthroplasty result difficult to obtain.
c. Deformities in PIP, DIP, and wrist may need to be corrected to enhance MP joint function.
d. Concurrent soft tissue (ligamentous, intrinsic, and tendon) reconstruction optimized outcome.
V. CAPUT ULNA
A. Mechanism of deformity
1. Dorsal subluxation of the ulna due to distal radioulnar joint (DRUJ) synovitis and capsule stretch (piano key sign).
2. Wrist supination, ulnar, and volar translation result from extensor carpi ulnaris subluxation ulnar and volar.
3. *Dorsal ulna can cause ischemic or attritional rupture of finger extensor tendons, starting with fifth dorsal compartment (Vaughn–Jackson syndrome)
B. Nonoperative treatment
1. Optimize medical management
2. Splinting
3. Local steroid injections
C. Operative treatment is indicated for pain relief with motion. These approaches require that the hand be under minimal load-bearing demands.
1. Synovectomy of the DRUJ
2. Distal ulnar resection for unstable ulna (Darrach procedure).
3. Distal ulnar pseudarthrosis (Sauve–Kapandji procedure) preserves ulnocarpal joint if it is in good condition.
4. Hemiresection arthroplasty of DRUJ preserves triangular fibrocartilaginous complex and ulnar length.
VI. SWAN-NECK DEFORMITY
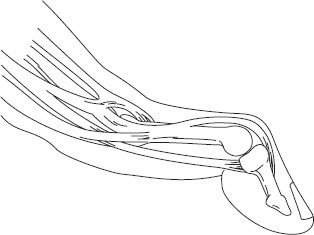
A. Hyperextension of proximal interphalangeal joint (PIPJ) with Distal interphalangeal joint (DIPJ) flexion (Fig. 43-2)
B. *Mechanism of deformity (three distinct mechanisms are possible)
1. Synovitis at DIPJ  leads to rupture of distal extensor tendon
leads to rupture of distal extensor tendon  mallet deformity
mallet deformity  extensor imbalance and volar plate laxity
extensor imbalance and volar plate laxity  PIPJ hyperextension
PIPJ hyperextension
2. Synovitis at PIPJ  volar plate laxity
volar plate laxity  PIPJ hyperextension
PIPJ hyperextension  extensor imbalance
extensor imbalance  DIPJ flexion
DIPJ flexion
3. Intrinsic tightness  MP joint subluxations
MP joint subluxations  extensor imbalance
extensor imbalance  PIPJ hyperextension and DIPJ flexion
PIPJ hyperextension and DIPJ flexion
C. Correction of deformity depends on PIPJ mobility and destruction
1. If passively correctable in all metacarpophalangeal joint (MPJ) positions, then use PIPJ splint, DIPJ fusion, or retinacular ligament reconstruction.
Figure 43-2. Illustration of the characteristic configuration of the swan-neck deformity with synovitis of the flexor tendon sheath, flexion at the metacarpophalangeal joint, hyperextension at the proximal interphalangeal joint, and flexion at the distal interphalangeal joint.
2. If flexion is limited by MPJ position: Fix MPJ subluxation or release tight intrinsics.
3. If there is a fixed flexion deformity without joint destruction: Manipulation, lateral band mobilization, fix underlying deforming force.
4. If there is a fixed flexion deformity with joint destruction: Arthrodesis verus silicone arthroplasty of PIPJ
a. Fuse joints where stability is most important
i. Index (to maintain pinch): Fuse at 30 degrees
ii. When necessary, can fuse middle finger at 35 degrees, ring at 40 degrees, and small at 45 degrees.
b. Replace joint where motion is important: Typically middle, ring, and small fingers (to maintain power grip).
VII. BOUTONNIERE DEFORMITY
A. Flexion at PIPJ with hyperextension at DIPJ and MPJ (Fig. 43-3).
B. Mechanism of deformity
1. Synovitis at PIPJ  attenuation of central slip
attenuation of central slip  flexion at PIPJ
flexion at PIPJ  volar subluxation of lateral bands
volar subluxation of lateral bands
2. Shortened oblique retinacular ligaments  DIPJ hyperextension
DIPJ hyperextension
3. Compensatory MPJ hyperextension
C. Correction of deformity
1. If passively correctable with mild deformity: Synovectomy and splinting ± tenotomy of terminal tendon.
2. If passively correctable with moderate deformity: Synovectomy with central slip/lateral band reconstruction ± tenotomy of terminal tendon.
3. If there is a fixed flexion deformity: Arthrodesis vs. arthroplasty of PIPJ as above (see Section “Swan-Neck Deformity”)
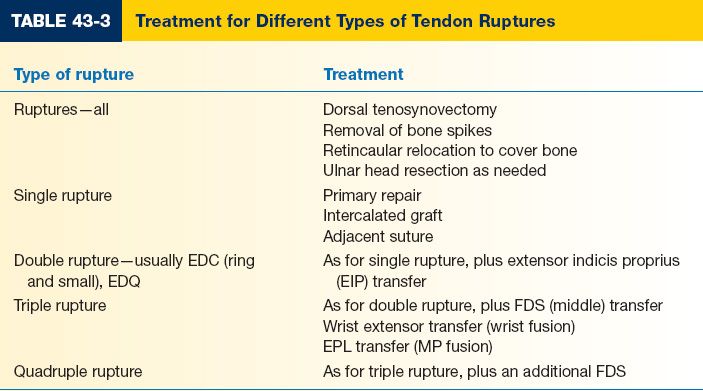
VIII. TENDON RUPTURES (TABLE 43-3)
A. It is important to differentiate the cause of a sudden inability to extend a finger
1. Extensor tendon rupture from attrition: (−) active extension, (−) maintenance of extension, (−) tenodesis effect (passive finger extension with wrist flexion)
2. Ulnar subluxation of extensor tendon at MPJ: (−) active extension, (+) maintenance of extension, (+) tenodesis effect
3. Posterior interosseous nerve palsy at elbow from synovitis: (−) active extension, (−) maintenance of extension, (+) tenodesis effect
4. Palmar subluxation of MPJ: Evident on X-ray and physical examination
B. Extensor tendon rupture
1. *Extensor digitorum communis (EDM) is the most common extensor tendon to rupture.
2. *Vaughan–Jackson syndrome: EDM, extensor digitorum communis (EDC)-small, EDC-ring usually rupture in sequence; may proceed to rupture more radial tendons.
Figure 43-3. Characteristic configuration of rheumatoid boutonnière deformity with metacarpophalangeal joint hyperextension, proximal interphalangeal joint flexion, and distal interphalangeal joint hyperextension, with florid synovitis depicted over the proximal interphalangeal joint.
3. Treatment is tenosynovectomy, address caput ulna (with Darrach procedure), tendon grafts or transfers
a. EPL rupture: Transfer EIP, EDM, or extensor pollicis brevis
b. EDM rupture: Transfer EIP if necessary
c. Single EDC rupture (usually SF): Cross-link to adjacent EDC (usually RF)
d. 2 EDC ruptures: Transfer EIP
C. *Flexor pollicis longus (FPL) rupture (Mannerfelt syndrome): Most common flexor tendon ruptured.
1. Inability to flex the thumb IPJ
2. Caused by osteophytes of the scaphoid irritating the FPL
3. Causes: Synovitis, carpal osteophyte
4. Treatment is synovectomy, osteophyte resection, and tendon graft or transfer
OSTEOARTHRITIS
I. GENERAL
A. Most common form of arthritis: Clinically affects 3% to 7% of adults
B. Osteoarthritis (OA) is a noninflammatory primary cartilage disease that is characterized by progressive articular cartilage deterioration and reactive new bone formation.
C. Cartilage changes are manifested by joint enlargement, pain, stiffness, contracture, and angular deformity.
D. Females > males, usually over 40 years of age, possible genetic predisposition
E. The carpometacarpal (CMC) joint of the thumb and the IP joints of the digits are most frequently affected.
F. In contrast to RA, OA has less inflammatory reaction in the joints
G. Nonoperative therapy is the mainstay of treatment, though there are surgical options for recalcitrant cases.
II. HISTORY AND EVALUATION
A. Most common complaint is an insidious onset of joint pain and stiffness that interferes with function of the hand.
B. Pain is usually activity related
C. CMC arthritis usually presents with pain and weakness with pinch and grasp
D. Examination
1. Joint swelling and occasional tenderness
2. Periarticular enlargement (Heberden nodes at distal interphalangeal [DIP] and Bouchard nodes at proximal interphalangeal [PIP]).
3. Mucous cysts can be present at the DIP and cause nail deformities
4. Crepitus with joint passive range of motion and positive “grind test”
1. Dedicated three-view radiographs are generally all that is needed to confirm the diagnosis of an osteoarthritic joint.
2. Findings include osteophytes, narrowed joint space, eburnation (bony sclerosis), and subchondral cysts.
III. NONOPERATIVE TREATMENT
A. No medical treatment available for the underlying disease process in OA
B. Treatment is for symptomatic control
1. Activity modification
2. Splints
3. NSAIDs
4. Injection (steroids, hyaluronic acid)
IV. SURGICAL TREATMENT
A. DIPJ
1. Mucous cyst excision
a. Usually done without skin excision with an H-shaped incision over the dorsal DIPJ.
b. If skin is severely thinned, a rotation/advancement flap is designed for closure.
c. Important to take down the osteophytes to reduce the recurrence rate
2. Arthrodesis
a. Can be done with longitudinal K-wires or Acutrak or Herbert screw
b. Usually done with 5 to 10 degrees of flexion.
B. PIPJ
1. Arthodesis
a. Indicated for pain relief but loss of range of motion is less than ideal, particularly in the ulnar digits for power grip.
b. Can be done with K-wires, tension band, or internal fixation
c. When considering fusion, the PIPJ of the index finger is fused at 25 degrees of flexion, advancing by 5 degrees for each finger ulnarly.
2. Silicone arthroplasty: Frequent fracture rate, but easily revised
3. Pyrocarbon arthroplasty: High complication rate has made this option fall out of favor at the PIPJ.
C. MCP Joint: Pyrocarbon arthroplasty is a good option at this joint
V. THUMB CMC JOINT
A. Findings
1. Early symptoms: Pain, swelling, crepitus, and weak pinch
2. Late symptoms: Metacarpal adduction and web contracture
3. Signs: Positive grind test (pain with axial loading of thumb CMC)
B. Mechanism of deformity: Volar carpal (beak) ligament from volar-ulnar base of the first metacarpal to the trapezium degenerates  destabilizes the thumb CMC
destabilizes the thumb CMC  joint wear
joint wear
C. Surgical options
1. Arthrodesis
a. Fuse at 30 to 40 degrees palmar abduction, 30 degrees radial abduction, and 15 degrees pronation.
b. Nonunion is a frequent complication.
2. Trapeziectomy with/without ligament reconstruction
a. Studies show that trapeziectomy alone is just as efficacious as other techniques.
b. Subsidence occurs with all surgical options, to differing degrees
c. Trading pain relief for some residual weakness
d. Trapezium excision with tendon interposition plus reconstruction of volar beak ligament using FCR, APL: good pain relief and restoration of pinch
DUPUYTREN’S CONTRACTURE
I. GENERAL
A. Well-known entity, but poorly understood disease process, where fascial layers of digits and palm are progressively involved in an abnormal, benign fibroproliferative disorder.
B. Major clinical features
1. Discrete nodules and contracted longitudinal cords which can result in finger contractures.
2. Progression is neither linear nor homogeneous
C. Histologically, there is uncontrolled tissue proliferation, myofibroblast, and increased extracellular matrix synthesis.
D. Pathogenesis remains controversial
II. EPIDEMIOLOGY
A. Demographics
1. Almost exclusively a disease of Caucasians—most commonly, people of Northern European ancestry (Scandinavia or British isles).
2. More common in males, 7 to 15 times greater incidence
3. Incidence peaks between ages 40 and 60
4. *Autosomal dominant inheritance with variable penetrance
5. Underlying cause is unknown; not occupational or traumatic
B. Location
1. Dupuytren disease affects the palm and most commonly the ring and small fingers.
2. Radial side involvement is more common in diabetics
C. Pathophysiology
1. Occurs in fibrofatty subcutaneous layer of volar hand (palmar fascia)
2. Normal BANDS contract to form pathologic CORDS
3. Similarity to wound healing and fibrosis biochemically
4. TFG-β and PDGF-B upregulated
5. Also GAG differences in Dupuytren tissue
D. Associated diseases
1. Alcoholism
2. Diabetes mellitus
3. Epilepsy
4. HIV infection
5. Chronic obstructive pulmonary disease (COPD)
E. *Dupuytren’s diathesis: Presents aggressively, with early onset and early recurrence; may require more extensive treatment. Characterized by three classic findings.
1. Knuckle pads (Garrod pads)
2. Foot involvement (Ledderhose disease)
3. Penis involvement (Peyronie’s disease)
III. ANATOMY
A. Bands are normal digital and palmar subcutaneous fibrous connective tissue
1. Spiral band
2. Lateral digital sheet
3. Natatory ligament
4. Pretendinous band
5. Grayson’s ligament: Palmar to neurovascular (NV) bundle
6. *Cleland’s ligament: Dorsal to NV bundle and does not become diseased
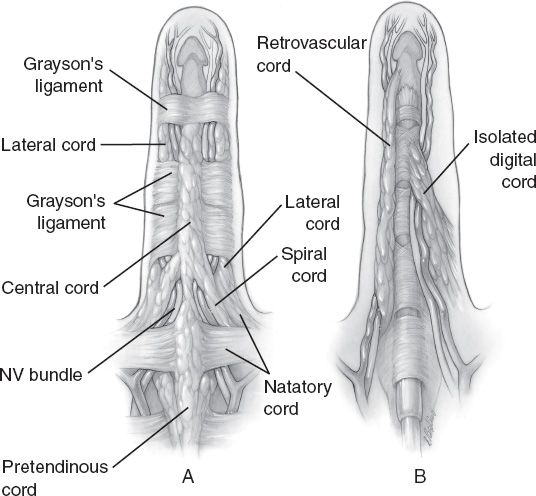
B. *Cords are diseased tissue (Fig. 43-4)
1. Spiral cord: From diseased pretendinous band, spiral band, lateral digital sheet, and Grayson’s ligament and central cord; wraps around the NV bundle. (Mnemonic: Plastic Surgeons Look Good).
Figure 43-4. Pathological anatomy of the distal palmar and digital anatomy. A: The more superficial diseased elements. B: The deeper diseased elements.
a. Grayson’s ligament
i. This is the most dangerous surgically because it drags the NV bundle: (1) Midline, (2) Proximal, and (3) Superficial
ii. Danger zone is between mid-palm and base of middle phalanx
2. Lateral cord: Contributes to PIP contracture
3. Natatory cord: From diseased natatory ligament; causes webspace contracture
4. Pretendinous cord: Cord in palm from diseased pretendinous band causes metacarpophalangeal joint contracture.
5. Central cord: Contributes to PIPJ contracture
6. Retrovascular cord: Causes DIPJ contracture
IV. INDICATIONS FOR TREATMENT
A. MCP joint contracture is usually correctible; operative release is indicated when
1. Contractures interfere significantly with daily activities (ask the patient)
2. Arbitrary contracture angles are less important, but usually an operation is done if MCP contracture is >30 to 45 degrees.
B. Any PIPJ contracture is difficult to fully correct, so early intervention is warranted
C. Contracture causing maceration or hygiene difficulties
D. “Table top test”: Patient unable to have digit and palm simultaneously on the surface of a table top is a sign of significant contracture.
V. NONOPERATIVE TREATMENT
A. Steroid injections may help painful palm nodules but do not prevent progression. Can be helpful to treat knuckle pads.
B. Collagenase injections (Xiaflex)
1. It is gaining popularity and data show promise with good long-term efficacy and reasonable side effect profile.
2. Indications for its use are still evolving, but often patient preference
3. FDA approved to be used in Dupuytren’s disease with a palpable cord
VI. OPERATIVE TREATMENT
A. Primary operations
1. Percutaneous needle aponeurotomy: Cords transected in clinic with sweep of a needle
2. Open fasciotomy: Done in older patients with significant medical comorbidities
3. Limited fasciectomy: Resection of only diseased tissue (most common procedure)
4. Regional fasciectomy: Resection of diseased tissue and a margin of non-diseased fascia
5. Extensive fasciectomy: Resection of diseased tissue and all potentially involved fascia
6. Radical fasciectomy (dermatofasciectomy): Consider in recurrent disease
B. Incision design
1. Many skin incisions have been advocated
a. Palmar: Transverse incision in proximal palmar crease is preferred
b. Finger: Longitudinal incision, broken up by Z-plasties over crease is preferred
2. Open palm technique (of McCash) heals well and prevents hematoma
C. Postoperative considerations
1. Splinting
2. Full extension for 2 to 3 days
3. Alternative: Intrinsic plus
4. Early active mobilization and nighttime splinting
5. May need dynamic splinting
6. Skin graft causes delay in early mobilization.
D. Recurrent disease
1. Repeat fasciectomy or dermatofasciectomy with full thickness skin grafting.
2. Joint arthrodesis
3. Amputation in severely affected or if NV compromise
E. Complications
1. Hematoma formation
2. Recurrence
3. Nerve injury: Remember that spiral cord pulls NV bundle proximally and abnormally centrally on the digit.
4. Vascular injury
5. Stiffness (i.e., failure to correct contracture, especially PIPJ)
6. Complex regional pain syndrome (CRPS)
F. Postoperative care
1. Dressing changes if open palm technique was used
2. Early aggressive active and passive range of motion therapy should begin as soon as tolerated.
3. Splinting: Some variability
a. Some advocate nighttime extension splinting.
b. Some advocate splinting in position of function.
PEARLS
1. DMARDs (“disease-modifying agents”) have made surgery in rheumatoid disease much less necessary, though the hand surgeon continues to play a crucial role in maintaining function.
2. Failure of medical therapy to improve tenosynovitis in an RA patient after 6 months is an indication for surgery.
3. The surgeon should differentiate reducible joint deformities from fixed ones, as the treatment options are very different.
4. Nonoperative treatment should be maximized prior to offering surgical treatment in OA
5. Pyrocarbon arthroplasty requires precise placement of the implants and stability of the soft tissues. High dislocation rate in the PIPJ position.
6. Spiral cord pushes the NV bundle volar, proximal, and midline. The NV bundle is often in a nonanatomic position, so be careful.
7. Do not combine fasciectomy with carpal tunnel release as there is an increased chance of CRPS.
QUESTIONS YOU WILL BE ASKED
1. What is the mechanism of a swan-neck deformity?
a. Synovitis at DIPJ  leads to rupture of distal extensor tendon
leads to rupture of distal extensor tendon  mallet deformity
mallet deformity  extensor imbalance and volar plate laxity
extensor imbalance and volar plate laxity  PIPJ hyperextension.
PIPJ hyperextension.
b. Synovitis at PIPJ  volar plate laxity
volar plate laxity  PIPJ hyperextension
PIPJ hyperextension  extensor imbalance
extensor imbalance  DIPJ flexion.
DIPJ flexion.
c. Intrinisic tightness  MP joint subluxations
MP joint subluxations  extensor imbalance
extensor imbalance  PIPJ hyperextension and DIPJ flexion.
PIPJ hyperextension and DIPJ flexion.
2. What is the mechanism of a boutonniere deformity?
a. Synovitis at PIP joint  attenuation of central slip
attenuation of central slip  flexion at PIPJ
flexion at PIPJ  volar subluxation of lateral bands.
volar subluxation of lateral bands.
b. Shortened oblique retinacular ligaments  DIPJ hyperextension.
DIPJ hyperextension.
c. Compensatory MPJ hyperextension.
3. What digital fascial structure is NOT involved in Dupuytren’s disease?
Cleland’s ligament.
< div class='tao-gold-member'>