CHAPTER 45 Revision Total Hip Arthroplasty
Megaprosthesis Proximal Femoral Replacement and Total Femur Replacement
KEY POINTS
 Examine patients thoroughly. Note scars fro previous surgeries, status of abductors, and the limb length.
Examine patients thoroughly. Note scars fro previous surgeries, status of abductors, and the limb length. Perform detailed preoperative templating. Have the company representative available to review your templating and to ensure that correct components, and neighboring sizes, are available on the day of surgery.
Perform detailed preoperative templating. Have the company representative available to review your templating and to ensure that correct components, and neighboring sizes, are available on the day of surgery. Minimize soft-tissue dissection off the native bone, and retain as much of the host bone as possible.
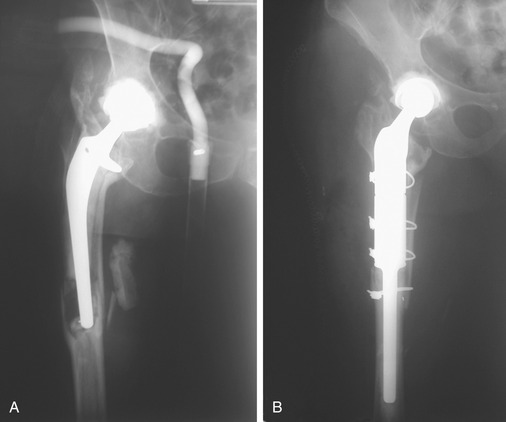
Minimize soft-tissue dissection off the native bone, and retain as much of the host bone as possible.During the past decade, remarkable advances in the field of revision hip reconstruction have been made. One such improvement was the introduction of second-generation modular prosthetic components (Fig. 45-1) that allow better ability to restore limb length and to achieve optimal soft-tissue tension, which may reduce the incidence of instability that frequently occurred after insertion of a monolithic megaprosthesis. The new generation of megaprostheses also provides a better environment for soft-tissue reattachment and the ability to reapproximate the retained host bone to the prosthesis. However, with current improvements in alternative reconstruction methods and increased use of cortical strut grafts to augment host bone, the indications for the use of the megaprostheses have narrowed.

FIGURE 45-1 Photograph shows new generation of modular proximal femoral and total femoral replacement prosthesis.
INDICATIONS
We currently reserve the use of the megaprosthesis (proximal femoral replacement and total femoral replacement) to expedite recovery for elderly or sedentary patients with massive bone loss that may have occurred after failed total hip arthroplasty (THA) deep infection (Fig. 45-2), periprosthetic fracture (Fig. 45-3), fracture nonunion with failed multiple attempts at osteosynthesis, and hip salvage after a failed resection arthroplasty. In younger patients in whom bone loss of high magnitude is encountered and the bone cannot be reconstructed by conventional means, an allograft prosthetic composite would be preferred over femoral prosthetic replacement. An important prerequisite for the use of prosthetic femoral replacement and allograft prosthetic composite is the availability of sufficient distal femoral length (>10 cm) for secure fixation of the cemented or uncemented femoral stem. When distal bone is severely deficient, total femoral replacement may be considered.
SURGICAL TECHNIQUE
Anesthesia and Patient Positioning
Regional anesthesia is preferred in these patients. Intraoperative blood salvage (cell-saver equipment) should be used in these patients. The anesthesia team should be warned about possible large volume loss and encouraged to monitor this closely. Invasive monitoring with the use of arterial lines or pulmonary catheters may be necessary in some patients. We place the patient in the lateral decubitus position and use hip rests to secure the patient (Fig. 45-4). Impermeable U-drapes are used to isolate the groin. The distal third of the extremity is also isolated from the field using impermeable drapes. It is very important to include the knee in the operative field in all of these patients—even in those undergoing proximal femoral replacement. Extension of the incision and arthrotomy of the knee to address intraoperative problems such as fractures extending distally are not uncommon. The skin is scrubbed with Betadine solution for at least 10 minutes and DuraPrep is applied before the application of Ioband to the skin.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree