What is the single most difficult challenge in revision rhinoplasty and how do you address it? During revision rhinoplasty, when dorsal augmentation is necessary and septal and ear cartilage is not available, what is the best substance for correcting the problem? If rib cartilage is used for dorsal augmentation during revision rhinoplasty, what is the technique to prevent warping of the graft? Alloplast in the nose – when, where, and for what purpose? Does the release and reduction of the upper lateral cartilages from the nasal dorsal septum always require spreader graft placement to prevent mid-one-third nasal pinching in reductive rhinoplasty?’ Analysis: Over the past 5 years, how has your technique evolved or what have you observed and learned in performing revision rhinoplasty?
Peter Adamson, Jeremy Warner, Daniel Becker, Thomas Romo, and Dean Toriumi address questions for discussion and debate:
- 1.
What is the single most difficult challenge in revision rhinoplasty and how do you address it?
- 2.
- 3.
- 4.
Alloplast in the nose – when, where, and for what purpose?
- 5.
- 6.
What is the single most difficult challenge in revision rhinoplasty, and how do you address it?
Adamson and Warner
The single most difficult challenge in revision rhinoplasty is the psychology of the revision rhinoplasty patient. With respect to the psychology of the revision rhinoplasty patient, there is no doubt that the consultative process and partnership with the patient in a revision setting is vastly different from that of the primary rhinoplasty patient. While primary rhinoplasty patients are often hopeful and optimistic, the revision rhinoplasty patient is often hesitant, upset, and leery regarding what can be achieved after a failed attempt to achieve their goals. While it is important to carefully listen to patients’ concerns in any consultation, it is especially important to understand the revision rhinoplasty patient’s original concerns in addition to their current concerns. In cases where the original concerns can truly no longer be addressed adequately, it is important to be honest with the patient and tell them so. An attempt to lead the patient down a pathway likely to fail is a recipe for disaster for both the patient and the surgeon. We often would like to think we can “save the day,” but we must realize what our limits are, especially in the patient who has had 3 or more surgeries. Fortunately, in many cases, the original concerns can be addressed surgically, and it is incumbent upon the surgeon to listen to these concerns and determine what can, and what cannot, be achieved.
Iatrogenic rhinoplasty deformities can come in a variety of shapes and forms. Patient concerns may be focused on the aesthetics of the nose, function of the nose, or both. Any deformity may have an impact on the patient. The challenges for the surgeon are to determine:
- 1.
If the deformity is real or imagined
- 2.
If the surgeon has the ability to correct the deformities
- 3.
If the surgeon has the ability to achieve the patient’s original goals
- 4.
Whether or not the patient has realistic expectations coupled with the likelihood of satisfaction after surgery.
The latter is the most difficult component of the decision making process because it can be unpredictable. But we can make reasonable assumptions during the consultation process based on the patient’s personality and demeanor. The patient who understands that surgical outcomes can be partly based on nature and the healing process, and who gives the previous doctor credit for doing their best, can typically be assumed to move forward in an optimistic manner. Conversely, the patient who is very negative regarding their previous doctor, and expresses this in a revision consultation, should be considered cautiously for surgery, as they may be likely to shift their negative feelings toward the new surgeon should there be a suboptimal revision outcome.
Becker
The nationally reported revision rate for primary rhinoplasty ranges from 8% to 15%. Experienced surgeons consistently achieve a high level of satisfaction among their patients. Still, complications can and do occur despite technically well-performed surgery. All surgeons have complications.
The single most important challenge in revision rhinoplasty is to reduce the occurrence of the most commonly seen complications. On a national and international level, the most common complications that I see relate to the midnasal pyramid and lateral alar sidewalls. These complications can be reduced by recognizing this and taking steps to mitigate the risk. In both situations, the key is to ensure strong structural support. For the lateral alar sidewalls, this relates to preserving appropriate support and adding additional support as needed. In the case of the midnasal pyramid, this relates to preserving support after hump reduction. This is discussed further in the final question.
Revision rhinoplasty is a term that encompasses a wide spectrum of technical problems, from straightforward to complex. For the more complicated revision rhinoplasties, in my practice the single most difficult challenge is the psychological aspect. The revision rhinoplasty patient is someone who sought aesthetic improvement and had the opposite result. They are acutely aware of the risks of surgery, they have a strong desire for repair coupled with fear of further worsening. The challenge is to help the patient understand the realistic expectations for surgery, and to empower them to be happy after a successful surgery.
In an established revision practice, patients seeking consultation include many who have all but lost hope. Commonly, the experienced revision surgeon will find that significant improvement is possible. However, to achieve success, it is important that the patient and surgeon come to a realistic understanding of what can and cannot be accomplished. Verbal communication supplemented by computer imaging helps surgeon and patient arrive at a shared surgical goal.
The revision rhinoplasty patient needs an environment in which they will be able to develop and maintain trust. This environment is best created by dedicating oneself to revision surgery, by placing a strong emphasis on patient education, by taking the time necessary to answer the patient’s questions and concerns, and by being honest and plain-spoken. The patient must feel that the surgeon has a passion for the operation, and that the surgeon has dedicated him or herself to the pursuit of excellence in nasal surgery, and specifically revision surgery.
I have addressed this challenge by dedicating my practice to nasal surgery. I have created an atmosphere where the patient understands that they are “in the right place.” I take the extra time with these patients that they need. I include them in the process so that they are empowered.
For the most part, the surgical techniques required for a difficult rhinoplasty are available and accessible to the dedicated, experienced and skillful surgeon. This does not ensure success. The current condition of the patient’s nose may be the primary limiting factor, and it is important to educate the patient about this. Unexpected problems can be encountered during surgery as well. Ultimately, if the possibility of satisfactory improvement cannot be offered, and/or if the patient is unwilling to accept the risks that are inherent to their surgery, the patient may not be a suitable surgical candidate.
Romo
The single most difficult challenge in revision rhinoplasty is lengthening the scarred cephalically rotated, shortened nose with absence of vestibular mucosa under the upper lateral cartilages. These problems are often associated with a myriad of other nasal deformities, including internal valve collapse, external valve collapse, overresected dorsum, tip asymmetries, bossa, columella show or retraction, and alar deformities. Each of these conditions needs to be diagnosed and treated appropriately.
When patients present for an initial revision rhinoplasty consultation, a considerable amount of time – 45 minutes to 1 hour – is allowed. A thorough history of prior nasal surgery is documented. Prior treatment records are obtained if necessary. A complete physical examination of the internal and external nasal structures is completed. The deformities and problems are then documented on a template. Subsequently, a discussion with the patient commences on the philosophy, complications, benefits and possible treatment plan for the revision rhinoplasty.
Once the extent of the stenosis is determined, the treatment plan proceeds to surgical management. It is well known that lysis of stenosis with stenting using either silastic sheeting or tubing will result in restenosis once the stenting is removed. Therefore relining of the structures is required.
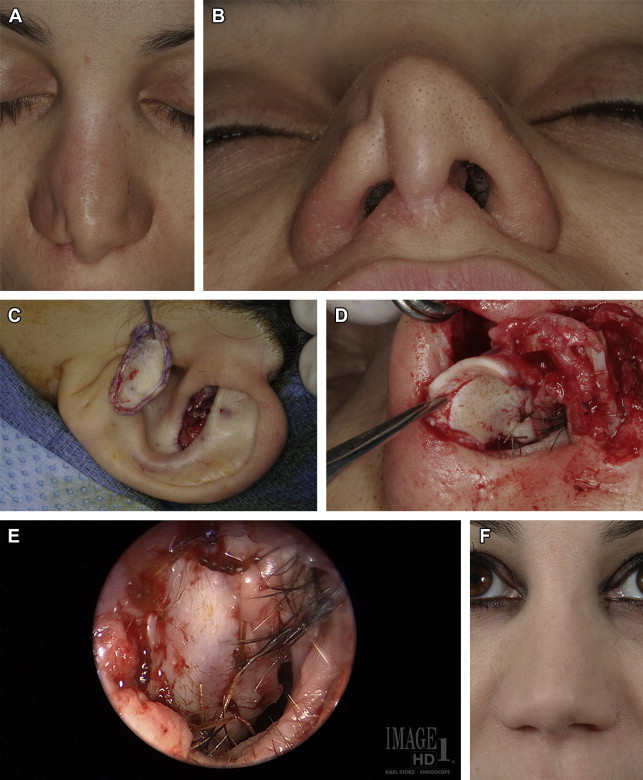
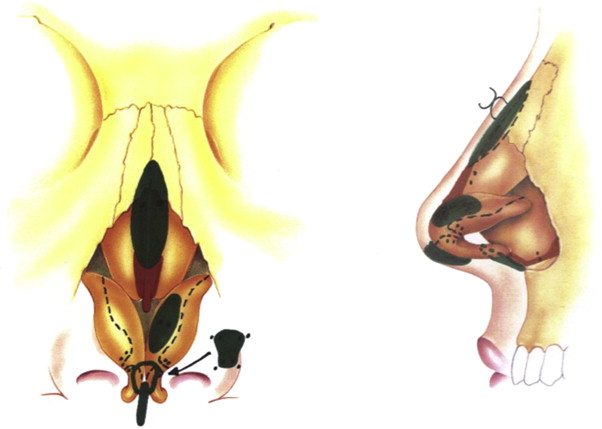
I perform this procedure using a full-thickness skin graft taken from the trichophytic hairline at the mastoid region. An open rhinoplasty technique is employed. The residual upper lateral cartilages are detached from the nasal dorsal septum. Scar tissue lateral to the cartilage is resected. The skin graft is inset at the dorsal septum-nasal bone interface. The skin graft is positioned so the epithelium is facing into the nasal vault. One side of the graft is sutured to the superior nasal septal mucosal line and the alternate edge of the skin graft is sutured to the mucosal lining of the released upper lateral cartilage. This continues inferiorly in a widening manner allowing for expansion of the mid- and lower one-third of the nose. This relining is carried down medially to the septal angle inferiorly and to the superior rim of the planned position of the lower lateral limb cartilage. Structural grafting of the upper lateral cartilages, dorsal augmentation, and lower lateral cartilage reconstruction can then commence. This may entail spreader grafts with caudal extension, caudal septal extension grafts, lower lateral battens, alar rim grafts and columellar augmentation ( Fig. 1 ). This structural grafting is doomed to failure unless nasal vestibular lining is replaced, thereby releasing the tethered scarred down nose.

Toriumi
In my experience the most challenging problem in revision rhinoplasty is correction of soft tissue deformities of the nose. These include cases of skin compromise after necrosis or infection ( Fig. 2 ), severe columellar scarring ( Fig. 3 ), severe alar notching ( Fig. 4 ), and over-resection of the alar base ( Fig. 5 ). Some of these deformities are associated with the use of alloplastic implants. In such cases of soft tissue deformity it is very difficult to recreate normalcy to the nose. When addressing soft tissue deformities, damaged soft tissues may need to be replaced. Reconstruction is complicated when these soft tissue deformities are in three-dimensionally complex areas of the nose such as the soft tissue triangle or facets ( Fig. 6 A, B). These areas are very difficult to reconstruction and unfortunately are damaged or deformed from previous surgery more often than I would like to see. To correct these deformities I typically place composite skin cartilage grafts into the site of scar contracture to replace missing vestibular mucosa. This requires creative use of composite grafts taking special care to design grafts to fit the defect and also placement to maximize camouflage of the grafts (see Fig. 6 C–G). Despite placement of structural grafts and composite grafts complete correction is rarely possible. These deformities do not fall into the category of typical deformities seen in revision rhinoplasty such as the pinched nasal tip, inverted-V deformity, saddle nose deformity, polly-beak deformity, alar retraction, over-rotated nasal tip, short nose, hanging columella, and supra-alar pinching. With a normal skin envelope most of these more typical secondary deformities are readily correctable using structural grafting. However, with severe soft tissue defects it is very difficult to completely correct the deformities.





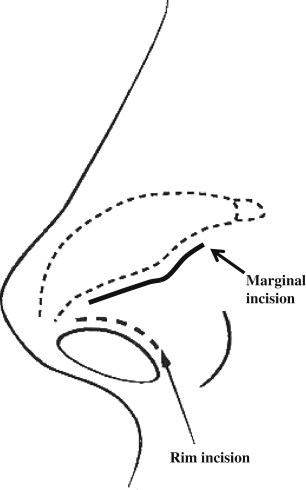
Prevention of soft tissue deformities requires careful positioning of incisions, avoiding closure of the columellar and marginal incision under tension, precise closure of all external and intranasal incisions and conservative alar base reduction. There is rarely a need to make a “rim” incision which is made along the alar margin and introduces a high likelihood for alar notching ( Fig. 7 ). Some surgeons confuse this incision with a marginal incision which is made along the caudal margin of the lateral crura. When performing a delivery approach or external approach one should use a “marginal” incision along the caudal margin of the lateral crura which is at least 3 mm to 5 mm away from the alar rim and moving further away as you move laterally. Surgeons should also avoid making transcolumellar incisions to high on the columella as this can lead to deformity of the soft tissue facets. Ideally the transcolumellar incision should be made at the level of midcolumella or just below midcolumella ( Fig. 8 ).

During revision rhinoplasty, when dorsal augmentation is necessary and septal and ear cartilage are not available, what is the best substance for correcting this problem?
Adamson and Warner
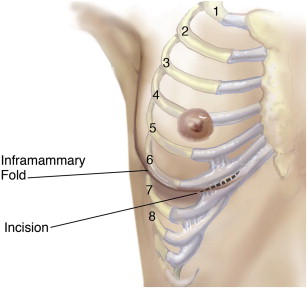
When ear or septal cartilages are not available for rhinoplasty in revision cases, I prefer to use autologous rib cartilage to reshape the nose and maintain its structure ( Figs. 9–12 ). Autologous rib cartilage graft harvest is easy, quick, safe, and abundant. I can now harvest rib cartilage through a 2 to 3 cm incision in the inframammary crease and it typically only adds about 15 to 20 minutes to the case, making it an equally good donor site compared with other cartilage harvesting options. The perichondrium can also be used as an overlay soft graft to soften any harsh contours. Of course, septal cartilage is an ideal donor site given the fact that it can be completely hidden and blends into the recovery from the nasal surgery. There is no doubt that rib cartilage grafting does add additional donor site healing pain and scarring. However, pain can be minimized by taking only a portion of the rib, and the scar tends to heal well and is quite well hidden. Some patients presenting for revision rhinoplasty may find the thought of using rib cartilage a foreign and anxiety-provoking concept during my initial consultation with them. After discussing the harvesting process, recovery, and benefits of using this powerful grafting material, patients are uniformly comfortable with the idea and have no problem with this as part of the operative plan.


One of the biggest issues in using rib cartilage is creating the ideal shape. A boat shaped graft, tapering both cephalically and caudally is ideal. I also believe that, in addition to warping being a cause of postoperative aesthetic disappointment, malplacement rather than postoperative displacement is a significant issue. I prefer autologous rib graft over synthetic materials, as I have seen a suboptimal number of patients with synthetic graft-related complications, including infections and extrusions – complications that I have not seen with autologous grafting.
Becker
There is not a single best substance. The literature describes calvarial bone, autogenous rib, autogenous bone-cartilage rib graft, and irradiated rib as options. Alloplasts are also an option. Each option offers risks and benefits. These must be conveyed to the patient, and the surgeon and patient can together make the best choice.
For example, in an older patient with other health issues, in need of significant dorsal augmentation, the additional surgical time and recovery may make an autogenous graft less desirable. In these patients, another issue is that the cartilage of the rib may be calcified and less than ideal. An irradiated rib graft may be the best choice in this situation. Donor site morbidity, re-absorption risk, infection risk, warping, and other risks are all factors that must be weighed and considered with the patient.
On May 4th, 2011 this subject was elegantly discussed and highlighted at the American Academy of Facial and Reconstructive Surgery (AAFPRS) Advances in Rhinoplasty Course in Chicago, Illinois. In a panel entitled, “My Op Note,” distinguished surgeons described 5 different preferred methods for augmenting the dorsum. Each surgeon indicated a preference for their choice of material.
Dr Rollin Daniel described augmentation of the dorsum with diced cartilage. His assistant dices the cartilage so that it can fit through a tuberculin syringe. He creates a tube of deep temporal fascia and injects the diced cartilage into this tube. He then molds it with his sterilely gloved finger and guides it into place with a percutaneous suture. He reported 350 cases in 9 years and stated that he had not seen any resorption of cartilage in these cases.
Dr Dean Toriumi described augmentation of the dorsum with autogenous rib cartilage. He reported that critical points to minimize warping including careful carving, anticipating the bending and carving accordingly, creating a tight pocket for insertion, and fixation to the bony dorsum. He suture secured rib perichondrium to the undersurface of the rib graft, and feels that this is a critical step. At times, a percutaneous K-wire is necessary to facilitate fixation. He reports that there is a significant learning curve to successful autogenous rib grafting.
Dr Peter Hilger described the use of autogenous rib cartilage and bone, harvested from the 11th rib. He similarly feels that stability with bony fusion is key. He favors this graft because it “replaces like with like” and because the risk of warping or bending is mitigated, as bone generally does not warp. He also reports the need for a K-wire at times.
Dr Eduardo Yap reported an extensive experience with alloplasts, specifically with Gore-Tex. He reported over 1000 cases from 2006 to 2009 with only 4 infections, 1 in a primary case and 3 in revisions. He reports that minimizing operating time, and avoiding medial osteotomies/exposure of the intranasal space to the dissection plane, may be a factor in minimizing infection.
Dr Russ Kridel described his extensive use of irradiated rib. He reported long-term follow-up with no difference in absorption compared to autologous rib. He stated that the preparation of the rib was important, that the Tissue Bank must not chemically treat the rib graft.
To summarize, there is no single best choice. Each option offers risks and benefits. These risks and benefits must be conveyed to the patient, and the surgeon and patient can together make the best choice.
Romo
The plan for dorsal augmentation during revision rhinoplasty is determined during the preoperative evaluation. The loss of dorsal height and width may involve only the middle third of the nose, dorsal bridge cartilage and upper lateral cartilages or may also involve the upper one-third of the nose; ie, nasal bones. Rarely are the nasal bones solely overresected.
If nasal dorsal augmentation is necessary, then autologous tissue is the best grafting material ( Table 1 ). The nasal septum is the ideal graft because of its characteristics of providing long-term architectural support. Even if a portion of the septal cartilage is curved, these sections can be incised and carved so that the graft will lay down flat. The obvious drawback is that adequate septal cartilage may not be available because of prior resection.
| Type | Pros | Cons | Recommended Uses | Comments |
|---|---|---|---|---|
| Autogenous grafts | ||||
| Cartilage | ||||
| Septum | Well proven Low extrusion rates Low infection rates Use for structural support and soft tissue augmentation | Limited availability in revision cases | Dorsal onlay, tip grafts, columellar strut, alar batten, soft tissue filler | Gold-standard grafting material |
| Auricular | Pros similar to septum Concha cymba similar shape to lower lateral cartilage | Limited supply Separate donor site harvest Associated warping | Alar battens, dorsal onlay, tip grafts | — |
| Costal | Ample supply Similar to septum | Warping Donor site morbidity | Dorsal onlay, tip, columellar grafts, batten grafts, soft tissue filler | Cannot harvest in elderly owing to ossification |
| Bone | ||||
| Split calvarium | Ample supply | Donor site morbidity Resorption Potential of fracture Palpability | Dorsal onlay, columellar strut, alar batten | Not recommended in children |
| Temporalis fascia | Ample supply | Separate donor site | Soft tissue filler Camouflage grafts | — |
| Homologous grafts | ||||
| Irradiated rib | Ample supply Biocompatibility | Resorption Patient stigma Warping | Dorsal onlay, tip grafts, collumellar strut, alar batten, soft tissue filler | — |
| Alloderm | Ample supply Biocompatibility | Resorption | Soft tissue filler Camouflage grafts | — |
The next alternative would be auricular cartilage. This includes the concha cymba and concha cavum cartilage. Because of the intrinsic curve in these cartilages, they are difficult to use solely as dorsal onlay grafts. Even if the spring is broken in these cartilages, by cross-hatching and morsalization, they tend to be deficient in length. However, they can be utilized for internal valve spreader grafts.
Without a doubt, during revision rhinoplasty, if dorsal augmentation is required, the ideal grafting material is autologous costo-chondrial cartilage. This can be harvested with minimal complications once the technique is mastered. The major difficulty is the actual carving of the graft into its desired shape and having the graft maintain that shape without warping. This problem is so common, that one of the masters of the technique, Dr Jack Gunter, dealt with it by placing a K-wire down the length of the graft in order to prevent warping. Over time, the wire became exposed and had to be removed along with the subsequent warped graft. One of our own contributing authors, Dr Dean Toriumi, designed a technique that lessens this warping process, which will be reviewed during his portion of this discussion.
Toriumi
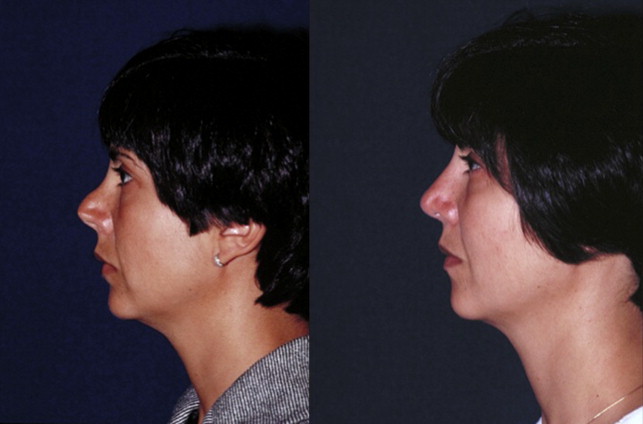
I prefer to use autologous costal cartilage as it is abundant, relatively easy to access, very strong, and predictable to use with good long-term outcomes. By minimizing dissection costal cartilage can be harvested with low morbidity and less pain than with ear cartilage harvest. I prefer to use the sixth rib as it usually lies just under the inframammary crease allowing the incision to be hidden under the breast. Additionally, the sixth rib is surrounded by the fifth and seventh ribs allowing its removal without destabilizing the chest wall and causing pain ( Fig. 13 ). The sixth rib is favorable in that one can harvest a relatively long and straight segment for dorsal augmentation. Some patients have a significant genu in the sixth rib which may necessitate using the seventh rib if a long straight segment is needed. I harvest rib cartilage via a 1 cm incision in the right chest ( Fig. 14 ). Typically the 1 cm incision gets stretched to 1.3 cm ( Fig. 15 ). In most cases the incisions heal to the point where they are relatively inconspicuous ( Fig. 16 ). I have a very low complication rate, patients have minimal pain, with no instances of pneumothorax.



I prefer not to use any alloplastic implants in the nose as they always have the potential to extrude or become infected. It is true that most implants do fine over the lifetime of the patient. However, when infection or extrusion occurs it can be devastating to the patient frequently creating soft tissue deformities. I also choose not to use irradiated homograft costal cartilage as it does not become vascularized and therefore acts as a non-viable implant. In older patients the costal cartilage can become calcified however it is rare that I am unable to find usable cartilage in most patients. I have also found that rib cartilage in patients who are age 40 to 55 years is less likely to bend or warp. This older cartilage has a brown tint and may be more brittle but is definitely less likely to warp. If a patient has a calcified chest wall I will go to the ear for cartilage. In most patients that do not have adequate septal cartilage I will go directly to the chest to harvest costal cartilage as I feel it is a better option for dorsal augmentation.
I have not used the technique of wrapping diced cartilage in fascia for dorsal augmentation. I prefer to use a solid segment of costal cartilage that is precisely carved to create symmetric and well defined dorsal aesthetic lines (brow-tip aesthetic lines). The diced cartilage in fascia does not have the same structural integrity as a solid piece of rib cartilage and therefore is not able to create the same definition to the dorsal lines. I also believe that the diced cartilage can deform or change shape over time potentially leading to an unfavorable contour. We do not have enough data on the long-term efficacy of this technique and if there is any resorption over time. Additionally, there is chance that thinner skin will contract leading to a “cobble stoning” effect.
Using costal cartilage for dorsal augmentation is associated with a significant learning curve. Harvesting the costal cartilage is not complicated. It is the planning, carving of the graft, placement into a tight midline pocket and rigid fixation that require precise execution. Using this technique one can create a natural appearing nasal dorsum that also feels natural as they are not moveable.
During revision rhinoplasty, when dorsal augmentation is necessary and septal and ear cartilage are not available, what is the best substance for correcting this problem?
Adamson and Warner
When ear or septal cartilages are not available for rhinoplasty in revision cases, I prefer to use autologous rib cartilage to reshape the nose and maintain its structure ( Figs. 9–12 ). Autologous rib cartilage graft harvest is easy, quick, safe, and abundant. I can now harvest rib cartilage through a 2 to 3 cm incision in the inframammary crease and it typically only adds about 15 to 20 minutes to the case, making it an equally good donor site compared with other cartilage harvesting options. The perichondrium can also be used as an overlay soft graft to soften any harsh contours. Of course, septal cartilage is an ideal donor site given the fact that it can be completely hidden and blends into the recovery from the nasal surgery. There is no doubt that rib cartilage grafting does add additional donor site healing pain and scarring. However, pain can be minimized by taking only a portion of the rib, and the scar tends to heal well and is quite well hidden. Some patients presenting for revision rhinoplasty may find the thought of using rib cartilage a foreign and anxiety-provoking concept during my initial consultation with them. After discussing the harvesting process, recovery, and benefits of using this powerful grafting material, patients are uniformly comfortable with the idea and have no problem with this as part of the operative plan.
One of the biggest issues in using rib cartilage is creating the ideal shape. A boat shaped graft, tapering both cephalically and caudally is ideal. I also believe that, in addition to warping being a cause of postoperative aesthetic disappointment, malplacement rather than postoperative displacement is a significant issue. I prefer autologous rib graft over synthetic materials, as I have seen a suboptimal number of patients with synthetic graft-related complications, including infections and extrusions – complications that I have not seen with autologous grafting.
Becker
There is not a single best substance. The literature describes calvarial bone, autogenous rib, autogenous bone-cartilage rib graft, and irradiated rib as options. Alloplasts are also an option. Each option offers risks and benefits. These must be conveyed to the patient, and the surgeon and patient can together make the best choice.
For example, in an older patient with other health issues, in need of significant dorsal augmentation, the additional surgical time and recovery may make an autogenous graft less desirable. In these patients, another issue is that the cartilage of the rib may be calcified and less than ideal. An irradiated rib graft may be the best choice in this situation. Donor site morbidity, re-absorption risk, infection risk, warping, and other risks are all factors that must be weighed and considered with the patient.
On May 4th, 2011 this subject was elegantly discussed and highlighted at the American Academy of Facial and Reconstructive Surgery (AAFPRS) Advances in Rhinoplasty Course in Chicago, Illinois. In a panel entitled, “My Op Note,” distinguished surgeons described 5 different preferred methods for augmenting the dorsum. Each surgeon indicated a preference for their choice of material.
Dr Rollin Daniel described augmentation of the dorsum with diced cartilage. His assistant dices the cartilage so that it can fit through a tuberculin syringe. He creates a tube of deep temporal fascia and injects the diced cartilage into this tube. He then molds it with his sterilely gloved finger and guides it into place with a percutaneous suture. He reported 350 cases in 9 years and stated that he had not seen any resorption of cartilage in these cases.
Dr Dean Toriumi described augmentation of the dorsum with autogenous rib cartilage. He reported that critical points to minimize warping including careful carving, anticipating the bending and carving accordingly, creating a tight pocket for insertion, and fixation to the bony dorsum. He suture secured rib perichondrium to the undersurface of the rib graft, and feels that this is a critical step. At times, a percutaneous K-wire is necessary to facilitate fixation. He reports that there is a significant learning curve to successful autogenous rib grafting.
Dr Peter Hilger described the use of autogenous rib cartilage and bone, harvested from the 11th rib. He similarly feels that stability with bony fusion is key. He favors this graft because it “replaces like with like” and because the risk of warping or bending is mitigated, as bone generally does not warp. He also reports the need for a K-wire at times.
Dr Eduardo Yap reported an extensive experience with alloplasts, specifically with Gore-Tex. He reported over 1000 cases from 2006 to 2009 with only 4 infections, 1 in a primary case and 3 in revisions. He reports that minimizing operating time, and avoiding medial osteotomies/exposure of the intranasal space to the dissection plane, may be a factor in minimizing infection.
Dr Russ Kridel described his extensive use of irradiated rib. He reported long-term follow-up with no difference in absorption compared to autologous rib. He stated that the preparation of the rib was important, that the Tissue Bank must not chemically treat the rib graft.
To summarize, there is no single best choice. Each option offers risks and benefits. These risks and benefits must be conveyed to the patient, and the surgeon and patient can together make the best choice.
Romo
The plan for dorsal augmentation during revision rhinoplasty is determined during the preoperative evaluation. The loss of dorsal height and width may involve only the middle third of the nose, dorsal bridge cartilage and upper lateral cartilages or may also involve the upper one-third of the nose; ie, nasal bones. Rarely are the nasal bones solely overresected.
If nasal dorsal augmentation is necessary, then autologous tissue is the best grafting material ( Table 1 ). The nasal septum is the ideal graft because of its characteristics of providing long-term architectural support. Even if a portion of the septal cartilage is curved, these sections can be incised and carved so that the graft will lay down flat. The obvious drawback is that adequate septal cartilage may not be available because of prior resection.






