Injuries in overhead throwers are common, and there are limited data on return to throw programs in the literature. This article outlines the criteria that baseball players should meet before initiating throwing and further describes an evidence-based throwing program that can be utilized to aid in the rehabilitation of overhead athletes and optimize chances of returning to same level of throwing. These guidelines may be used for rehabilitation after injury is treated operatively or nonoperatively.
Key points
- •
Before beginning a throwing program, an athlete should be pain-free, have no motion arc deficits in abduction, minimal scapular dyskinesis, have completed strength training, and completed plyometric training.
- •
Baseball players, specifically pitchers, have differing range of motion profiles when comparing nondominant and dominant arms, which should be considered during rehabilitation.
- •
We outline a throwing program for fielders and pitchers that should be completed with the inclusion of a radar gun.
Introduction and background
Upper extremity injuries are common in baseball, accounting for approximately 51% of major league baseball (MLB) injuries, with an average annual cost of US$423,267,634 when players are designated to the injured list. , In recent years, we have seen a considerable rise in upper extremity injuries at all levels, from adolescents to the professional level, which has led to a subsequent increase in surgical management. Return to play/throw rates vary significantly based on the pathology treated. Ulnar collateral ligament (UCL) reconstruction return to play rates range from 75% to 85% overall with a 63% return to same level in MLB players. Superior labrum anterior to posterior repair has an overall return rate of 63% to 80%, with a 52.3% return to same level of play for pitchers. , Rotator cuff repair has a return rate of 38% to 49.9% for same level of play in all levels of baseball players and further to 33.3% for MLB players. Shoulder instability has the lowest return rate, ranging from 10% to 19%.
To improve return to play rates, rehabilitation protocols have been an important subject of research at all levels of competition. However, this has been complicated, first, by a lack of consensus on the definition of return to play and, second, by differing rehabilitation protocols. Although a formal standardized definition has not been adopted, return to play most commonly refers to an athlete returning to competition in a game or competitive play with some studies investigating elite athletes further specifying this as a return to same level of sport. Additionally, a systematic review of rehabilitation protocols for UCL reconstruction revealed a wide variability of protocols, milestones, and timing of milestones considered vital during rehabilitation. Standardized evidence-based protocols are vital to prevent reinjury given that return to play rates decrease substantially to as low as 0% to 33% for revision surgery depending on pathology. In this review, we outline the criteria for engagement in a return to throw program and emphasize key milestones while presenting a structured throwing program based on data-driven rehabilitation programs to optimize player outcomes and return to play.
Preparing to throw
Prior to beginning a return to throw program after shoulder or elbow surgery, it is crucial to achieve specific milestones to prevent reinjury or exacerbation of pain that can lead to revision surgery. The criteria that we suggest should be met before initiation of a throwing program are lack of baseline pain, no rotational motion arc deficits in abduction, no scapular dyskinesis, completion of strength training, and completed plyometric training. One recent systematic review of return to throw in UCL reconstruction revealed similar criteria, also focusing on full range of motion (ROM), no pain, and completion of Advanced Throwers Ten and plyometric exercises. Our outlined criteria can serve as guidelines that should be met before initiating a return to throw program to minimize the risk of reinjury.
Pain Free
The athlete should be pain-free before initiating a return to throw program. Specifically, the athlete should have no swelling or inflammation of the joint and have no or very minimal pain at baseline. Mild pain may be acceptable (1–3/10 on a visual analog scale) when throwing and is commonly reported in the general population of uninjured pitches throwing less than the maximum pitches per day. Pain after UCL reconstruction has been linked to higher rates of revision surgery. , Pain and fatigue lead to changes in pitching mechanics, particularly changes in knee flexion and increased hip to shoulder separation, leading to increased shoulder and elbow torques that increase the risk for reinjury. , Pain at baseline and pain greater than 3 out of 10 during throwing should prompt a pause of a throwing program. These players should be re-evaluated with further examination prior to initiation of a return to play program.
Range of Motion and No Motion Arc Deficits in Abduction
Restoration of ROM to preoperative values and focus on total arc of motion are critical to prevent high torque on the shoulder and elbow during throwing. It is important to note that overhead athletes, and particularly pitchers, have different ROM profiles when comparing the dominant to the nondominant arm. Pitchers have decreases in dominant elbow extension (7.9°), elbow flexion (5.5°), and total flexion-extension arc (13.3°) when compared to the nondominant arm. , When looking at pitchers’ passive dominant shoulder ROM, they demonstrate on average 132° of external rotation (ER) at 90°, 52° of internal rotation (IR), and 102° of mean ER at 45° of abduction. These values can be used as a baseline when examining either ROM deficits or excesses. A shoulder flexion deficit greater than 5° is a significant risk factor for elbow injury, and the risk of elbow injury increases by 7% for each degree of ER deficit and 9% for each degree of decreased shoulder flexion. The loss of shoulder rotational ROM and increased elbow flexion can increase shoulder and elbow torque and risk for reinjury. However, too much shoulder ER can also predispose players to injuries, and therefore, a balance must be struck. Prioritizing postoperative matching of preoperative ROM rather than emphasizing end range stretching should be the focus during rehabilitation, which has been shown to improve outcomes during rehabilitation.
Previously, much of the focus on ROM was on glenohumeral internal rotation deficits (GIRDs); however, recent literature suggests that the focus should instead be shifted to rotational motion (total arc of motion). Certainly baseball pitching prior to skeletal maturity does contribute to an increased humeral retrotorsion, which is then reflected in an increased external and decreased internal rotation, without a change in total rotational arc. It has been shown that a decreased total arc of motion is significantly associated with IR deficits and, therefore, represents the underlying cause of GIRDs. Additionally, decreased total arc of motion is associated with decreased shoulder strength. Furthermore, a decrease in rotator cuff stiffness is associated with acute ROM gains as opposed to glenohumeral joint mobility or humeral torsion. Baseball players with shoulder pain show a significant decrease in total arc of shoulder motion, along with IR compared to pain-free players. ROM exercises should, therefore, focus on restoring total arc of motion rather than solely IR deficits, which will ultimately lead to improved strength and decreased rotator cuff stiffness that lead to decreased pain and risk of reinjury.
Scapular Evaluation
Another important aspect of a rehabilitation program is assessing the scapular mechanics of the overhead athlete, paying particular attention to scapular dyskinesis. The scapula plays an integral part in throwing mechanics. Scapular protraction and anterior tilt can increase loads and alter throwing motions leading to decreased performance and increased injury risk. Similarly to ROM profiles, healthy throwing athletes have significantly increased upward rotation, IR, and retraction of the scapula during humeral elevation compared to the general population. Rehabilitation protocols with regards to scapular mechanics have recommended a focus on serratus anterior muscle function to prevent impingement, while others focus mainly on assessing dyskinesis as this has long been associated with throwing-related injuries. Assessing for scapular dyskinesis entails examining for winging in the medial or inferior border, which may indicate abnormal protraction, anterior tilt, and/or internal rotation. Recent literature has shown that scapular dyskinesis may not be an isolated risk factor for shoulder injuries; however, patients with dyskinesis still had a 43% increased risk of shoulder pain. , We, therefore, choose to focus on rehabilitation of dyskinesis in the process of return to play to avoid exacerbating the injury or inciting shoulder pain, which could then, in turn, lead to further kinetic chain alterations and abnormal throwing mechanics.
Strength: Hip/Core and Upper Extremity
Hip and core strength are essential to a successful rehabilitation program due to their large contribution to the kinetic chain that generates the energy necessary for throwing. Furthermore, as pitch counts increase, core and leg muscles fatigue leading to breakdowns in the kinetic chain, altering throwing mechanics, and potentially resulting in injury. Hip abduction strength deficits and lumbopelvic control of the drive leg are also related to increased movement of the lower extremity that can lead to altered kinematics increasing the shoulder and elbow valgus torque. , Hip and core strength can be assessed with a single leg squat and forward lunge or a crossed toe-touch. Signs of imbalance or hip deviations during these exercises indicate that further strengthening is necessary before moving to a throwing program.
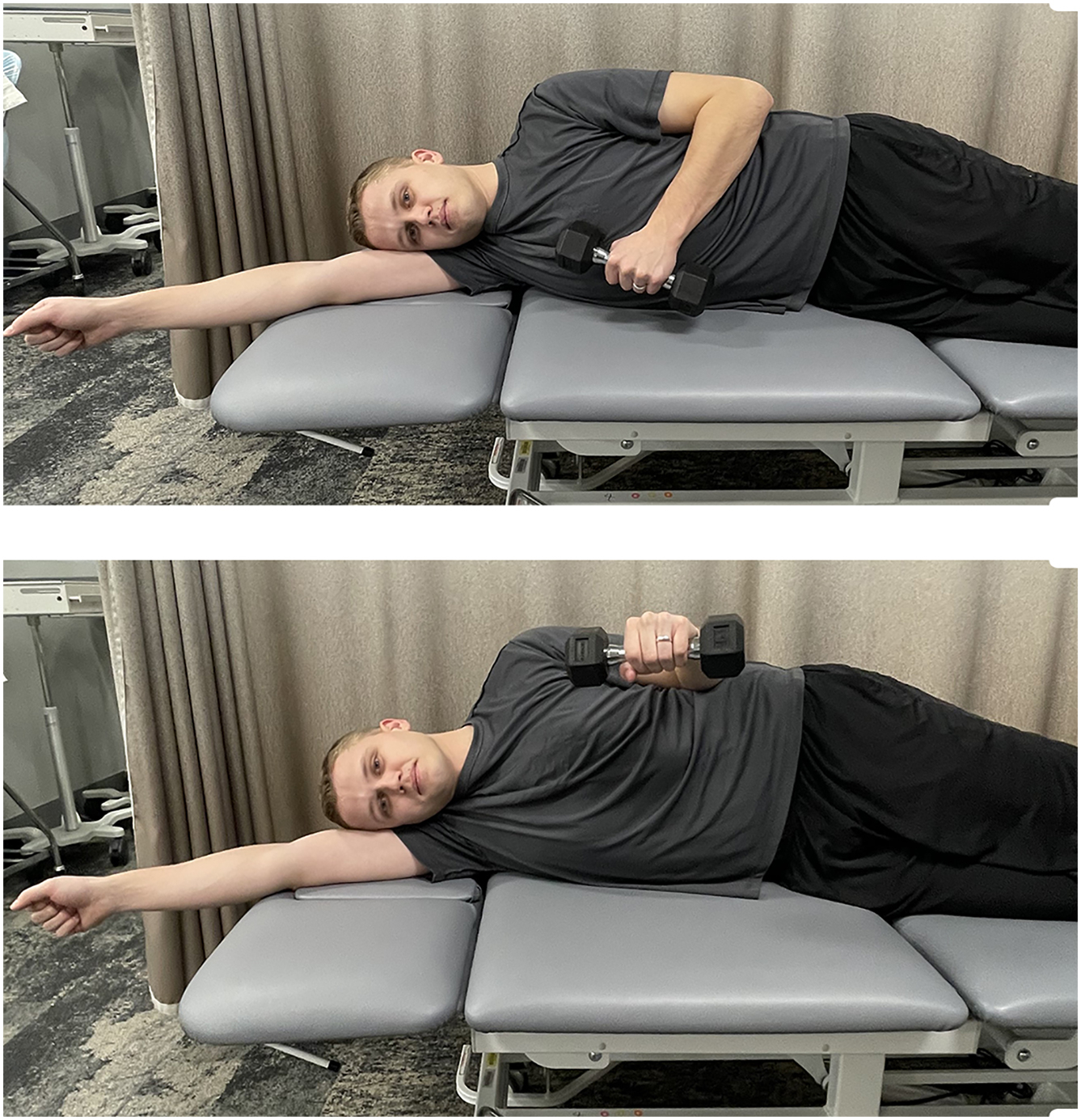
Upper extremity strength is also an important element to rehabilitation, particularly shoulder ER. ER deficits have previously been shown to be a risk factor for throwing-related injuries. , The dominant arm and nondominant arm have different strength profiles, and ER can be improved particularly with prone rowing into ER. ,
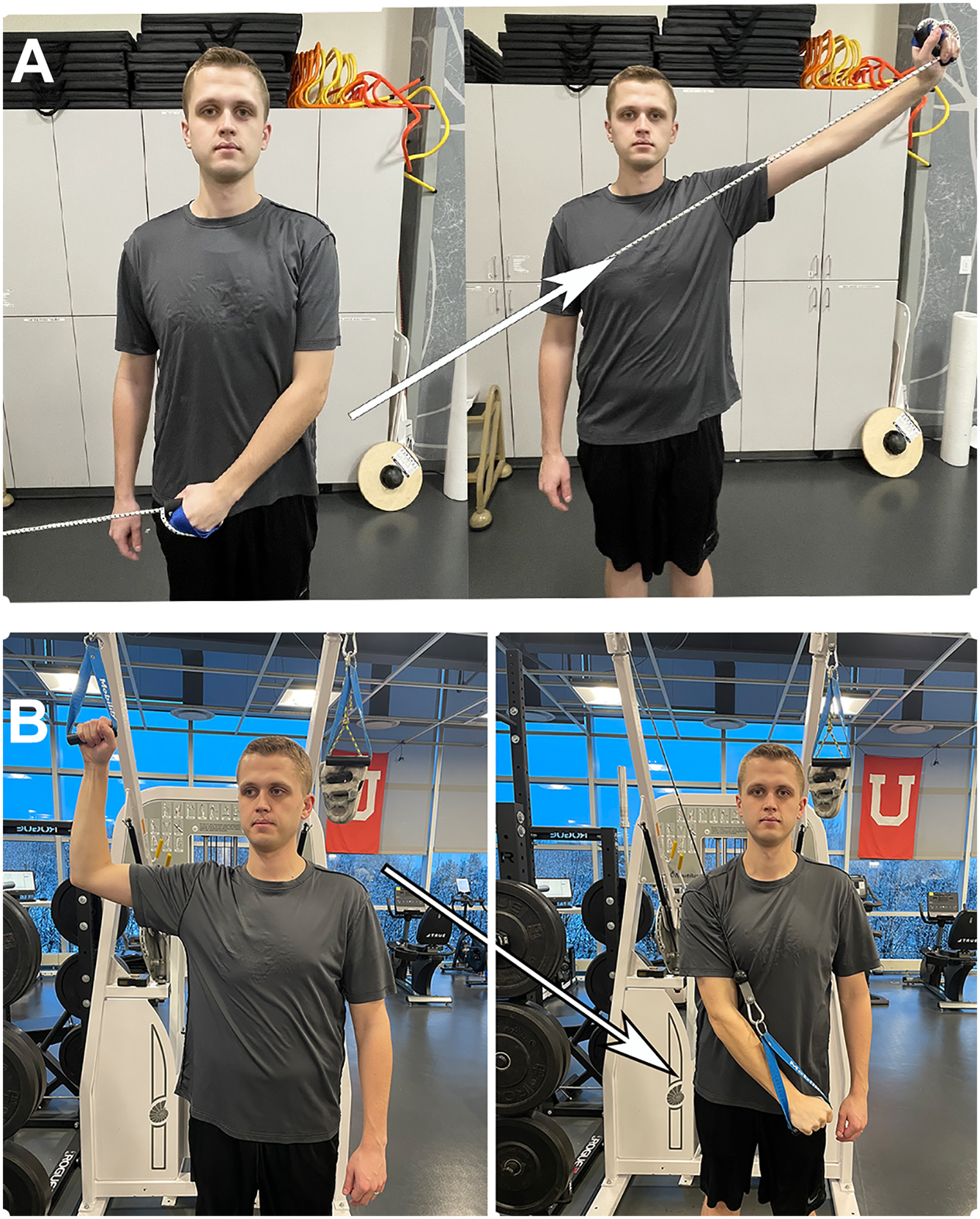
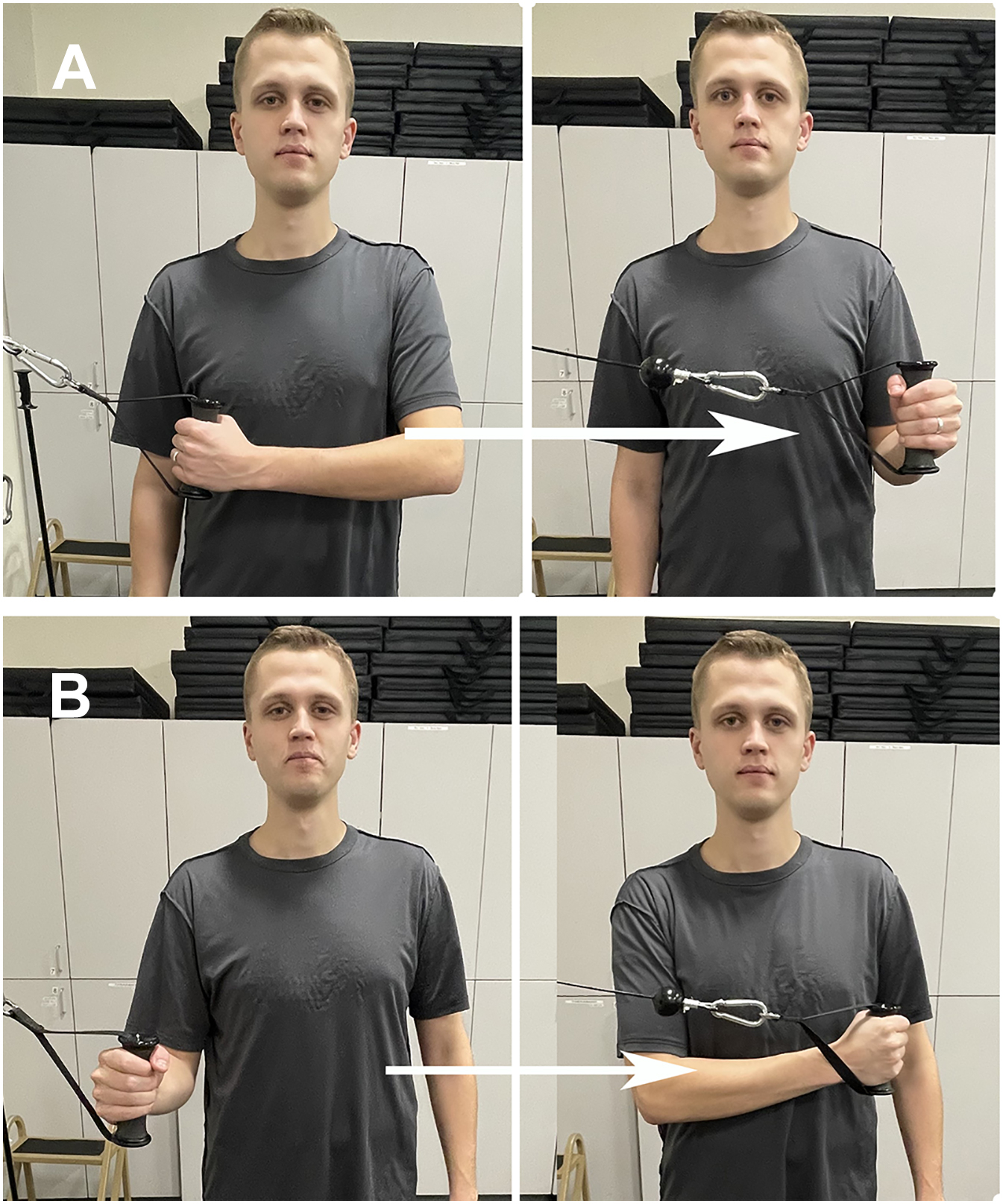
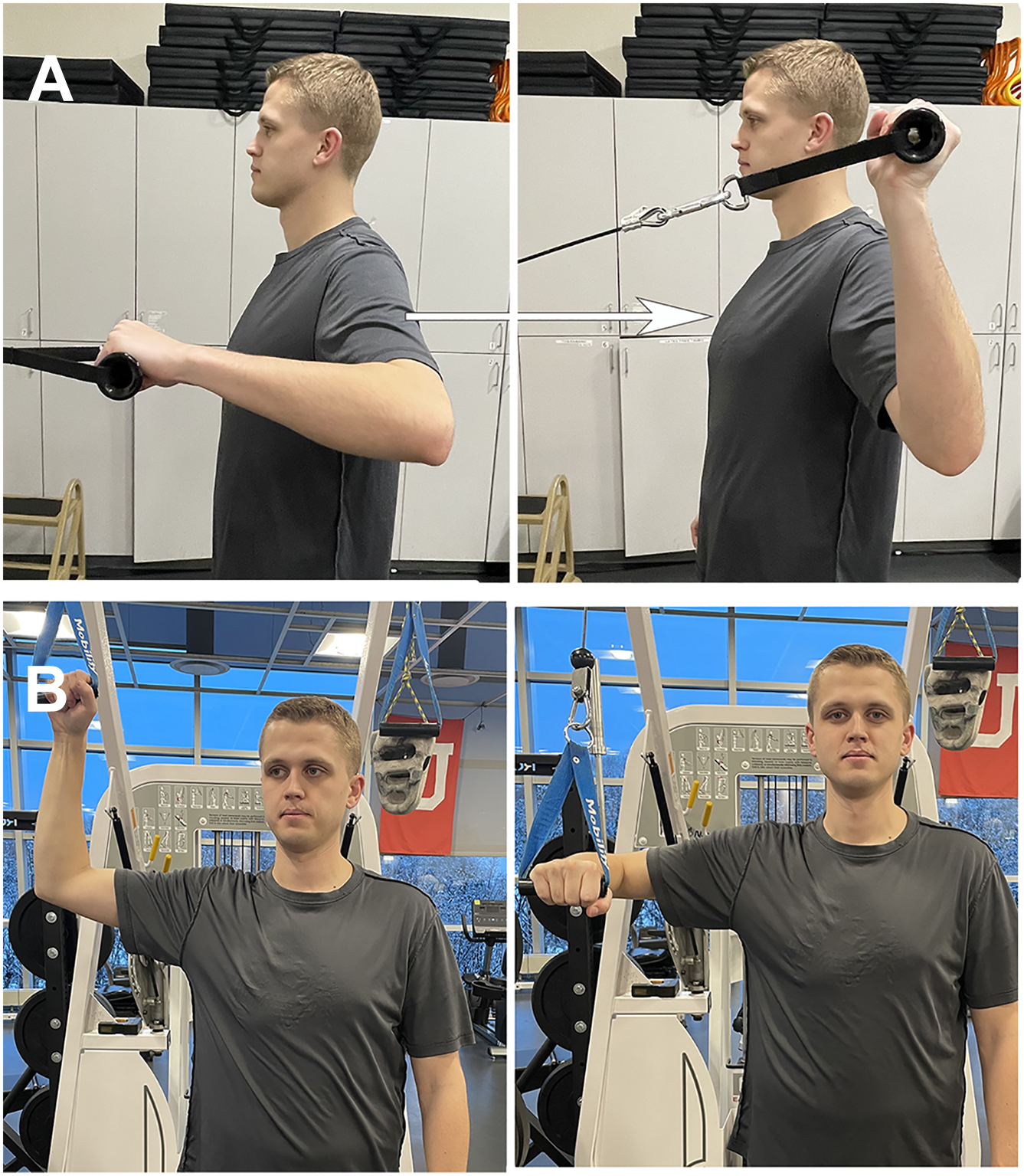
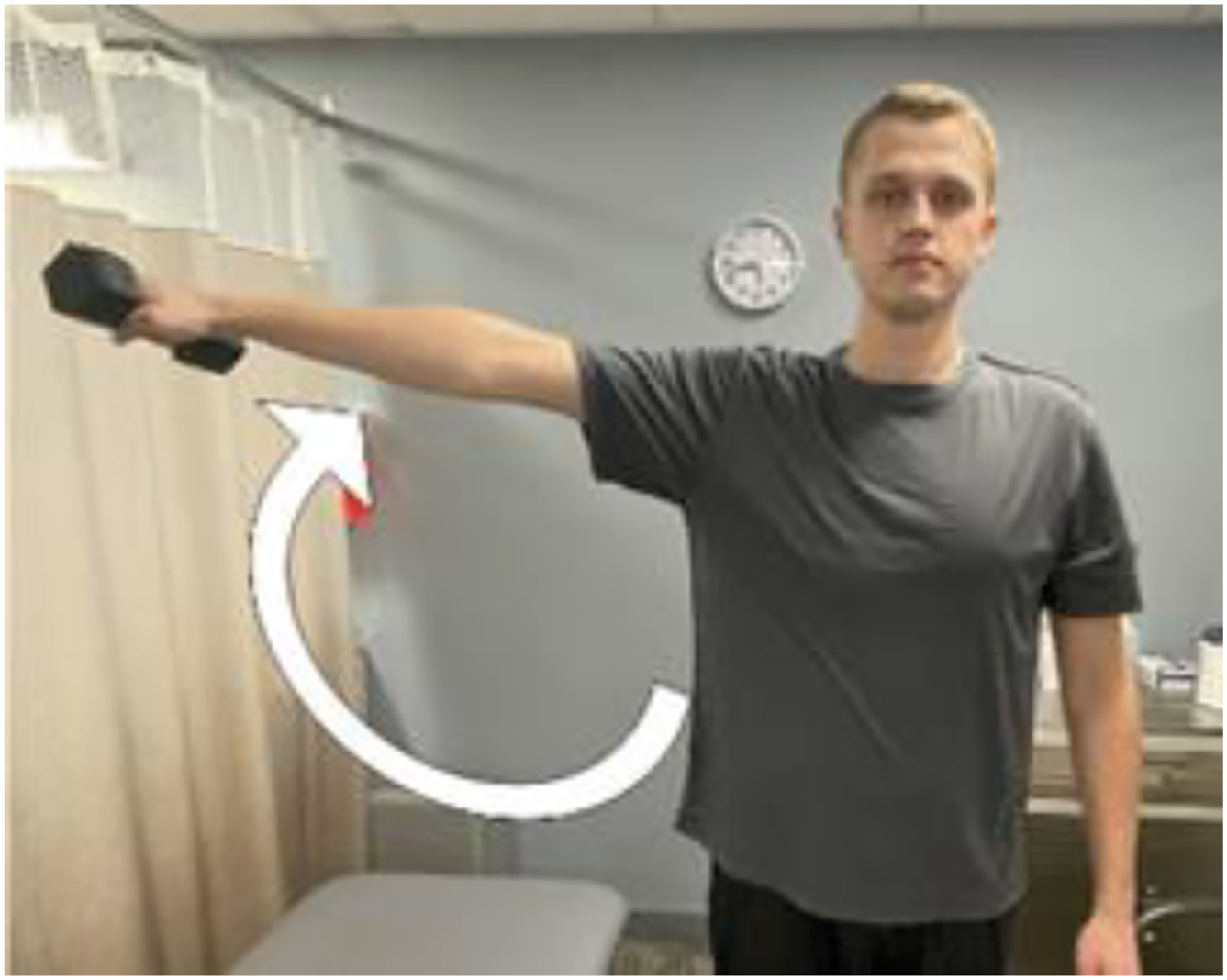
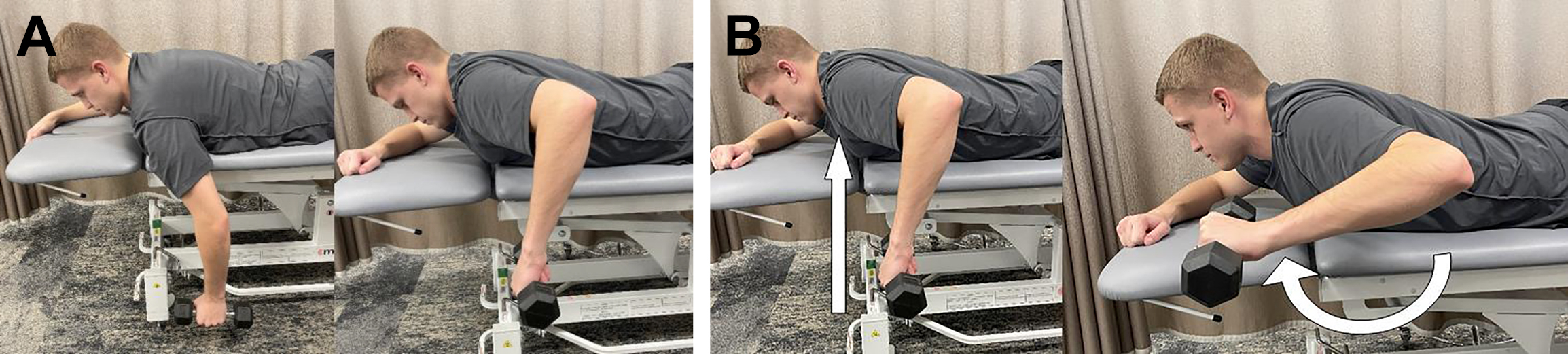
Plyometrics and Throwers Ten
Plyometrics are another aspect of rehabilitation that has gained popularity in all levels of baseball. Plyometrics utilize the stretch-shortening muscular cycle to develop power and improve strength and is thought to not have negative effects on muscle given it showed no significant rises in creatinine kinase or lactate dehydrogenase. , The exercises are widely published and have shown improved throwing velocity in programs greater than 7 weeks, as well as improved grip strength, side step, and standing long jump. , Plyometrics can be combined with the widely published Throwers Ten exercises and Advanced Throwers Ten exercises ( Figs. 1–14 ). These exercises are an important bridge between rehabilitation and return to throw as they utilize dynamic stabilization, neuromuscular control, and rotator cuff facilitation. The Throwers Ten in particular has shown improved torque and angular impulse on the dominant and nondominant arm by 10% to 14%, while also demonstrating an increase in throwing velocity. , These exercises function as a safe strengthening program that allows for an improved transition to a throwing program.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree