Reduction and Augmentation of the Breasts
Matthew R. Kaufman
Reza Jarrahy
Michael Jones
Reduction Mammaplasty
Although it is not altogether clear why many women in certain racial ethnic populations suffer from breast hypertrophy, the etiology is suspected to be some combination of hormonal, genetic, and developmental factors. Large-breasted women often have significant functional and psychosocial impairments, prompting them to investigate surgical options. In addition, these patients are prone to developing comorbid conditions, such as chronic back and neck pain, and often there are multiple medical professionals involved in the search for effective treatments.
Because reduction mammaplasty offers a cosmetic and functional resolution to the consequences of large breasts, it is associated with high rates of patient satisfaction. During the initial patient assessment, the physician must determine the patient’s desired breast size and be able to meet this desire using one of the various descriptions of surgical techniques.1,2,3 Some of the more common surgical methods are the inferior and superior pedicle techniques, whereas partial breast amputation with free nipple grafting is reserved for patients with massive breasts or significant risk factors.
Darker-complexioned women presenting for breast reduction surgery must be informed of the risk of unsightly breast scars and the possibility of needing scar revision treatments in the months to years that follow the initial procedure. Despite the increased risk of scarring that is present in these patient populations compared with their lighter skinned counterparts, most women will still undergo the procedure and achieve satisfaction because of the significant functional improvements.
Patient assessment and selection
Candidates for breast reduction surgery encompass a wide range of age groups, including young girls with virginal hypertrophy to elderly women seeking to reverse the effects of aging on large, uncomfortable, sagging breasts. During the initial assessment, a full history must be obtained, including age of breast development, pregnancy and lactation history, previous breast surgery, weight change, smoking, family history of breast cancer, and how past scars have healed. The patient should specifically state her goals regarding the desired breast size. During the physical assessment, a full breast exam must be performed. The physician should determine the degree of breast symmetry (or asymmetry) and the distances from the sternal notch to the nipple and from the nipple to the inframammary fold. These measurements will be important in determining the vertical lift requirements and the safest method of accomplishing the reduction; a common rule is that when the nipple to inframammary fold distance is greater than 17 cm, the inferior pedicle is less likely to support survival of the nipple. Another important consideration, especially pertinent in the darker-skinned patient, is the diameter of the nipple-areolar complex. In many women with mammary hyperplasia, this diameter will be greater than normal, and patients must be informed that it too will be reduced, along with the breast volume. Objective signs of breast hypertrophy should be elicited, such as bra-strap grooving, skin rashes or irritations, striae, postural abnormalities, and early kyphosis of the cervicolumbar spine. Preoperative assessment should include screening mammograms, especially for women older than 30 and for patients with a personal or family history of breast disease. It is also recommend that patients undergo mammography 6 months after surgery to establish a postoperative baseline. Patients with comorbid back pain conditions should be evaluated by an appropriate specialist and may require magnetic resonance imaging to objectify the chronic effects of breast hypertrophy on the spine.
Appropriate candidates for breast reduction surgery usually present with long-standing symptoms of back and neck pain resulting from large, pendulous breasts. Skin rashes, or intertrigo, and bra-strap grooving make up some of the cutaneous manifestations of breast hypertrophy. Women with severe breast asymmetry will also desire breast reduction to alleviate the unilateral symptoms plaguing their daily lives. Just as important are the psychosocial effects of breast hypertrophy that are especially disturbing to younger women or teenage girls suffering from virginal hypertrophy. The daily embarrassment that is often associated with this condition can be detrimental
to a teenager or young woman, thus negatively affecting both physical and mental development.
to a teenager or young woman, thus negatively affecting both physical and mental development.
The prevalence of obesity in ethnic populations has increased the number of people seeking breast reduction surgery as a way of treating the effects of weight gain on the breasts. Unfortunately, it is inappropriate to view reduction mammaplasty as a weight reduction procedure, and the best course of action is to recommend the patient lose weight before breast surgery. Ideally, a woman should be within 30 pounds of her ideal weight to be a surgical candidate. Abiding by this philosophy will improve patient satisfaction and reduce the rate of perioperative complications associated with surgery in obese patients.
Surgical techniques
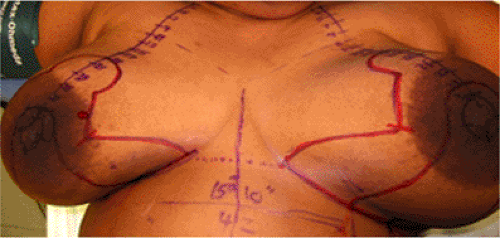
Arguably, the most common method of breast reduction surgery is the inferior pedicle technique, whereby the majority of parenchyma is removed from the medial, lateral, and superior quadrants, and the blood supply to the nipple-areolar complex is maintained from the inferiorly based soft tissues. The key to achieving surgical success is careful, accurate preoperative markings made with the patient seated or standing, usually in the holding area (Fig. 27-1). A complete technical description of the markings is beyond the scope of this chapter, so the reader is referred to previous publications that thoroughly outline the procedure.4,5 Notable aspects of the preoperative markings include setting the new nipple-areolar position by transposing the inframammary fold onto the breast mound and use of the keyhole pattern to design the resultant shape of the new nipple-areolar complex and determine the extent of skin resection. The markings will ultimately guide the surgeon toward the resultant breast scars, which include a periareolar incision and an “inverted T” incision at the base of the breast (Fig. 27-2). During the surgery, it is important to proceed in a systematic way, as even the most experienced surgeons can sometimes lose sight of the three-dimensional nature of the reduction procedure. It is also critical that there be attention to detail to achieve absolute breast symmetry and minimize resultant scarring (Fig. 27-3).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree