Recreating the Inframammary Fold with the Superficial Fascial System
Maurizio Nava
Joseph Ottolenghi
Egidio Riggio
Aesthetics of the Inframammary Fold Unit
The inframammary fold (IMF) is one of the basic elements in breast aesthetics. The beauty of the female breast is related to four IMF characteristics: contour, level, angle, and symmetry. Contour and level are permanent features after puberty. In contrast, angle and symmetry are changing features subsequent to both breast enlargement and aging events. The local examination must be consistently concerned with the four elements of the IMF.
Contour shapes the lower base of the breast mould on the thoracic wall, appears as an uninterrupted visual line, and is composed of three parts: the midpoint (i.e., the lowest point of the fold), and two segments, medial and lateral, respectively. The course draws a convex arch downward as being C-shaped, U-shaped, and nearly horizontal. Among them, the last one should be considered as the least attractive.
Level is found at the fifth and sixth ribs, and its lowest portion usually reaches the sixth intercostal space. The average distance from the areola is 5.5 to 7 cm for small breasts and 7 to 9 or more cm for large breasts. This transverse level is usually proportioned to the thorax length and the patient’s height.
Angle is given by the intersection of the lower profile of the breast mould with the thoracic plane. It is strictly related to breast ptosis. A decreasing degree is progressively reported for most of the female breast. An open angle appears in both prepubertal and small nonptotic breast. A 90-degree, or something more, angle accentuates the beauty of a youthful breast. In contrast, a sharp angle that appears in large, skin-redundant, hypoelastic, and elderly breasts, as also having fascial laxity, can be less pleasant. The IMF angle must be considered as one of the most important features in the aesthetic appearance of the breast.
Symmetry is affected by the earlier characteristics as comparing the left side with the right side. Generally, breast harmony is due to symmetry and embraces two prejudicial kinds of symmetry—metric and visual. Of course, metric symmetry must be of concern during the preoperative approach, but surgeons should always be aware of the patient’s expectancy and body self-perception, which are related to visual symmetry rather than to metric symmetry.
Anatomic landmarks are fundamental in creating IMF contour and level, even if from an apparent viewpoint, due to breast ptosis and weight, the angle sharpness is deeply influenced by the modifications of the fascial system by aging. Therefore, a clarification of the IMF anatomic structure is needed for better comprehension of the fundamental nature of IMF as a separate anatomic unit and for surgical respect of it.
Anatomy of the Inframammary Fold: the Superficial Fascial System
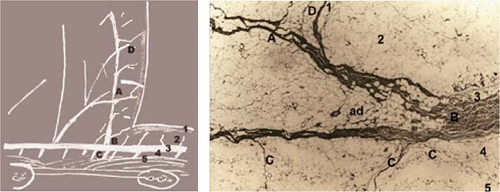
IMF formation and appearance are due to development of the breast and enlargement over time, as well as to its biological changes, including the aging breast, which influence the superficial connective frame of the breast (Fig. 43.1). There are three anatomic aspects of the superficial fascia that produce an IMF by themselves with no reference to large-scale structures as ligaments.
First, IMF appears to be a zone of subcutaneous adherence (i.e., thick retinacula between the superficial and deep fascia [zone of adherence]), where contiguous connective structures of both superficial and deep subcutaneous layers persist as different anatomic microunits of the same fascial frame, according to the concept of the skin-superficial/fat-superficial fascial system functional unit described by Lockwood (1), and applied in the study published by Nava et al. (2). Figures 43.2 and 43.3 show the superficial fascial system that is the fundamental frame of IMF.
Second, the superficial fascia of the inframammary region, direct prolongation of the abdominal one, extends to the retromammary space above the deep (muscular) fascia, deepening the level where IMF starts. The deeper plane is generated by the changing thickness of the deep subcutaneous layer that, in the abdomen, is separated from the deep fascia by a fatty layer, whereas, in the submammary region, this layer becomes more fibroareolar than fatty and hence thinner. Significantly, the sternal depression, similarly due to absence of fat in the deep layer and presence of adherent retinacula, can become a true fold in obese people, both male and female.
Third, the superficial fascial layer is a constant fibrous membrane thicker in the inframammary zone and in the whole abdomen (also called Scarpa’s), than in the retromammary zone of the female breast. Its thickening increases in time due to the action of the breast weight.
After clarifying the inframammary frame of the superficial fascial system, how to merge this with the entire connective frame of the mammary gland is another question to debate. The Cooper’s ligaments detach from the superficial fascia and go up to the skin. The same behavior can be observed regarding the capsular envelope, which is a fascial annex covering the anterior surface of the mammary gland. Such a fibrous band is made of merging thick retinacula, more apparent at IMF, at the site of detachment from the superficial fascia. This is the fibrous membrane that many authors confuse with the inframammary ligament: It can be interconnected to the muscular fascia through the superficial fascia; it can be joined to the presternal fascia at the medial extremity; the orientation follows the breast shape instead of the pectoral inferior border;
the density and thickness are related to age, breast size, and weight. It is not a true ligament but rather the capsule of a gland of ectodermal origin.
the density and thickness are related to age, breast size, and weight. It is not a true ligament but rather the capsule of a gland of ectodermal origin.
It should be said that the IMF anatomy has been a highly debated question for many decades and is strictly linked to the theories about the two-layered (3,4,5,6) or unilayered (7,8,9) superficial fascia. The fold had always been neglected by anatomists, perhaps because they did not believe it to have anatomic identity, even though it would appear to have a constant position. In contrast, plastic surgeons emphasized IMF identity until more recently (10,11), presuming the identification of a true inframammary ligament. According to Bayati and Seckel (10), this ligament should originate from the fifth rib periosteum medially, from the fascia between the fifth and sixth ribs laterally, and insert distally into the deep dermis of the submammary fold. Others tried to describe it through anatomic, histologic, radiologic, and ultrasonographic studies (12). Maillard and Garey described a crescent-shaped ligament between the skin and the anterior surface of the pectoralis major muscle, whose insertion was slightly inferior to the inframammary crease. Nevertheless, no anatomy textbook described any ligament, and Sterzi (9) did not address IMF in his anatomic study on the subcutaneous breast tissue in babies, virgins, women at puerperium, and older females.
Based on the authors’ anatomic dissections on fresh cadaver, histologic, and surgical investigations conducted on live dissections (2,3,4,5,6,7,8,9,10,11,12,13,14), it can be asserted that there is not a macrostructure featuring the IMF, but that its anatomic fundamentals lay on a special microstructure as totally generated by the superficial fascial system. In addition, breast parenchyma was not found in the histologic specimens. These statements were subsequently confirmed by Muntan et al. (15). These considerations were confirmed by another study; thus, preserving this superficial connective frame for a 1-cm thickness between dermis and muscular fascia, along the IMF contour, is not only precious but also oncologically safe (Fig. 43.3).
A clear and correct comprehension of the anatomy will facilitate surgeons safeguarding the IMF and rebuilding the interrupted frame after extensive breast surgery.
Surgical Procedures
Preserving the Inframammary Fold During Mastectomy
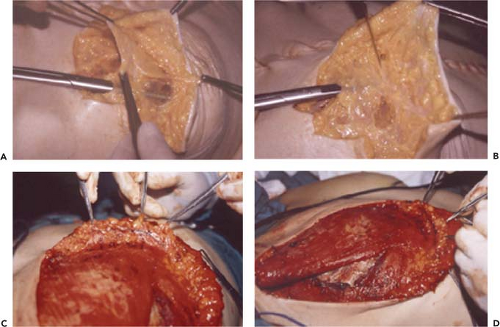
The breast resection can be delivered at the IMF—in the superficial subcutaneous layer and close to the glandular envelope—to be sure to include all breast tissue, but with the least damage of the dermis. Just a few millimeters above the inframammary crease, the knife cuts the Cooper’s ligaments and changes at the dissection plane to spare the superficial fascial system inside the IMF. Subsequently, the superficial fascia is scored a few millimeters upward and dissection arrives at the deep subcutaneous layer, above the muscular fascia. From this point, undermining is easily done in a cleavage plane, and the mammary gland can be radically removed in continuity with the axillary nodes if needed. Figure 43.4 (top) shows the conservative effect of an IMF-sparing radical mastectomy.
These proceedings allow reconstruction work improvement and help manage the inframammary redefinition after radical modified mastectomy, including skin-sparing ones.
Preserving the Inframammary Superficial Fascial System During Implant Pocket Undermining
These are four features to be considered for a good reconstruction: the IMF, the inferior pole, the superior slope, and the projection. The first two are defined by recreating the IMF, and the other two are defined by a correct implant selection. A better final aesthetic outcome in reconstructive surgery starts with a correct mastectomy.
The maintenance of the inframammary fascial system attachments to the deep plane (fasciomuscular layer) is mandatory along the IMF contour. Neither resection nor undermining below the IMF level should be made in both the superficial and the deep subcutaneous layers. Preserving and restoring the attachments (deep retinacula) between the superficial system and muscular plane are important maneuvers to be able to maintain the mastectomy field isolated from the implant submuscular pocket. The pocket’s dissection should always end inferiorly where the IMF appears. At this level, only if the integrity of the superficial plane was maintained after breast resection, the muscular fibers of the pectoralis major and the serratus anterior can be scored along the IMF contour, just 1 to 2 mm above the IMF level (Fig. 43.4, bottom).
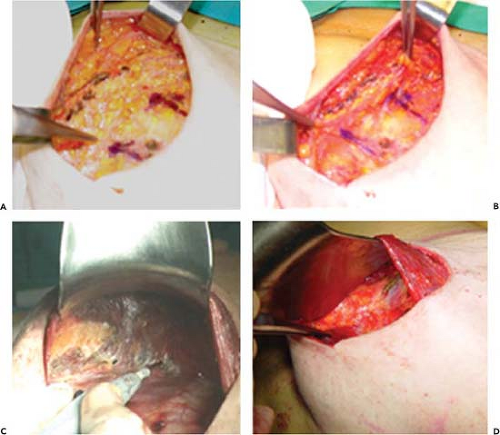 Figure 43.4. Mastectomy sparing the inframammary fold. Intraoperative views: fascial frame preserved at the mastectomy site (A, B), and superficial fascial plane preserved inside the submuscular pocket after scoring the serratus anterior and pectoralis major muscles (C, D).
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|