Reconstruction of the Cheek
Introduction
Achieving aesthetic surgical outcomes after reconstruction of cutaneous cheek defects requires knowledge of cheek anatomy and facial aesthetic regions. The size and location of the defect and the structures adjacent to the defect are assessed to determine where tissue can be recruited for construction of skin flaps without adversely affecting the nose, lips, and eyelids by secondary tissue movement. Analysis of each cheek defect is essential, and fundamental concepts of cutaneous flap biomechanics should be addressed (see Chapter 3) to facilitate tension-free wound closures with optimally positioned scars.
Fundamental Concepts
Anatomy and Aesthetic Units
The cheek is the largest facial aesthetic region and is juxtaposed to the orbital, nasal, and lip aesthetic regions. The aesthetic region of the cheek has the following boundaries: inferior bony orbital rim, nasofacial (cheek-nose junction) sulcus, line from the lateral canthus to the root of the helix, preauricular crease, melolabial crease, labiomandibular crease, and inferior border of the mandible (Fig. 20-1). The cheek can be conceptually divided into areas based on the difference of underlying bone, soft tissue, skin quality, and skin laxity. On the basis of these anatomic differences, there are four aesthetic units: medial, lateral, zygomatic, and buccal. The skin of the medial and buccal units is thicker and more mobile than the skin of the other units of the cheek. The skin of the lateral unit is moderately fixed to the underlying fascia, and the skin of the zygomatic area is quite fixed, in part by the cutaneous retaining ligaments in the region. This unit also has the least skin laxity.1
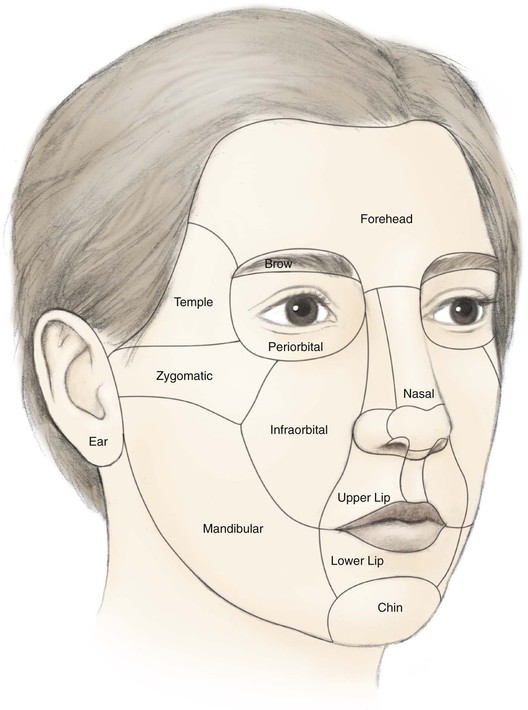
FIGURE 20-1 Aesthetic boundaries of cheek aesthetic region: inferior bony orbital rim, nasofacial sulcus, melolabial crease, labiomandibular crease, inferior border of mandible, preauricular crease, and line from lateral canthus to root of helix. Aesthetic region of cheek based on inherent mobility and thickness of skin may be divided into units: infraorbital (medial, buccal), zygomatic, and mandibular (lateral).
Several important ligaments collectively referred to as cheek retaining ligaments support the soft tissues of the cheek. Retaining ligaments in the area of the zygoma (known as McGregor’s patch)1 serve as strong bone anchors for supporting the skin overlying the zygoma. More inferiorly and anteriorly, a dense attachment to the skin known as the mandibular retaining ligament is present at the cheek where it joins the lower lip. This ligament accounts for the formation of the labiomandibular crease. Fibrous attachments of the superficial musculoaponeurotic system (SMAS) to the cheek skin at the junction of cheek and upper lip create the melolabial crease. The labiomandibular and melolabial creases provide important landmarks for concealing incisions and represent aesthetic boundary lines between the cheek and the upper and lower lips. The contour of the cheek is due to the convexity of the maxilla and the malar fat pad. The fat pad is well known to plastic surgeons for its relationship to aging of the midface. In addition to retaining ligaments, the cheek is supported by the muscles of facial expression. Most notable is the zygomaticus major positioned deep to the malar fat pad and invested by the SMAS.1
Lymphatic drainage of the cheek is primarily to the submental, submandibular, and preauricular lymph nodes. Additional drainage occurs to the second echelon of lymph nodes in the superior jugular chain.2 The vascular supply to the cheek skin is derived from three major sources, which perfuse the dermal and subdermal plexuses.1 The superficial temporal artery provides a minor supply through the transverse facial branch. The infraorbital artery provides collateral supply to the midcheek with anastomotic connections to the facial artery. The facial artery and its continuation as the angular artery provide the majority of blood to the skin of the cheek. The venous drainage is based on vessels that follow the named arterial supply.
The facial nerve provides motor innervation to the muscles of facial expression that form a base on which the subcutaneous tissue and skin of the cheek rest. The majority of sensory innervation of the cheek is provided by branches of the second division of the trigeminal nerve through the infraorbital nerve. The third division of the trigeminal nerve contributes to the sensory supply of the lateral cheek through the auriculotemporal nerve and of the inferior cheek through the mental nerve.
Flap Planning
When possible, scars should be positioned at the border of aesthetic units to provide the best camouflage. When scars cannot be placed in borders of aesthetic units, they are aligned parallel to relaxed skin tension lines (RSTLs), which are curvilinear in the cheek (Fig. 20-2). RSTLs are a result of the intrinsic elasticity of the skin and are perpendicular to lines of maximal extensibility.3 Therefore, wound closure oriented in an axis parallel to RSTLs results in less wound closure tension and more favorable scar camouflage. Wrinkles located in the lateral canthal region are largely due to the action of the orbicularis oculi muscle and provide a useful site in which to place incisions. In general, the boundaries of cheek aesthetic units and facial creases are more favorable locations than the RSTLs for positioning of scars.3
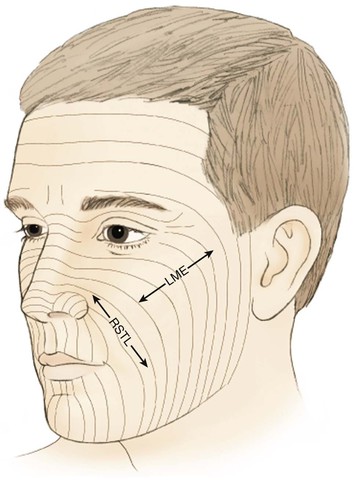
FIGURE 20-2 Configuration of relaxed skin tension lines (RSTLs), which are perpendicular to lines of maximal extensibility (LME). Elliptical excisions parallel to RSTLs result in less wound closure tension because skin recruitment is in axis of LME.
Medial Cheek Defects
Healing by secondary intention of small defects of the medial cheek (1 cm or less) can result in an acceptable appearance, particularly on concave surfaces such as the perialar and melolabial regions. However, most skin defects of the cheek do not heal with an acceptable aesthetic result when they are allowed to heal by secondary intention. This may be related to facial motion and the slightly convex surface topography of the cheek.
Primary wound closure is an excellent option for repair of smaller cutaneous defects of the cheek. Typically, it results in a linear suture line with minimal tension on the closure because wide skin undermining is possible. In general, undermining up to 4 cm beyond the borders of the defect improves tissue recruitment, whereas undermining more widely adds little to decreasing wound closure tension (see discussion of this in Chapters 3 and 6).4 Primary wound closure is a particularly good option when the resulting scar can be placed in the borders of the cheek aesthetic region or parallel to RSTLs. An example is a defect adjacent to the junction of the cheek and nasal sidewall (nasofacial sulcus) repaired with primary wound closure, resulting in a scar positioned in the sulcus, thus providing excellent camouflage (Fig. 20-3). Because most cutaneous defects created by micrographic surgery are circular, an ellipse can be designed such that the resulting scar is parallel to RSTLs. When the ends of the ellipse encroach on a facial structure or extend beyond the borders of an aesthetic unit, an M-plasty may be used to shorten the length of the closure. This technique eliminates or reduces the necessity of the scar’s crossing boundaries of aesthetic units (Fig. 20-4).
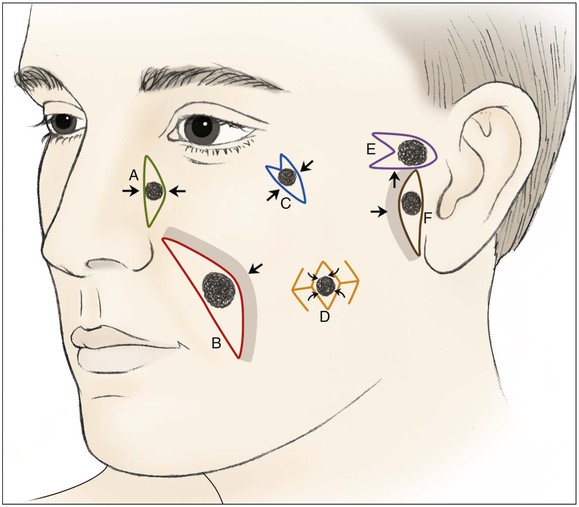
FIGURE 20-3 Various reconstructive techniques for small and medium-sized defects of cheek: primary closure (A); primary closure with asymmetric skin undermining (B; shaded area represents greater undermining); elliptical closure with M-plasty (C); rhombic flaps (D); advancement with M-plasty (E); and primary closure with asymmetric skin undermining (F).

FIGURE 20-4 A, A 3 × 2-cm skin defect of inferior medial cheek. Primary wound closure planned with bilateral M-plasties designed. B, Wound repaired. C, Postoperative result at 3 weeks. (Courtesy of Shan R. Baker, MD.)
The V-Y subcutaneous tissue pedicle island advancement flap is an effective way of reconstructing small defects of the medial cheek adjacent to the alae (Fig. 20-5). The flap is designed as an island of skin with a triangle shape, preserving the subcutaneous tissue beneath the skin island. Extending the incision used to create the flap to the proper depth is important. If incisions are too shallow, the ability to advance the flap will be restricted; and if incisions are too deep, the nerve supply to the facial musculature may be compromised. The flap is advanced and the wound closed so that the suture line assumes a Y-shaped configuration. The blood supply to the flap is from perforators that enter the subcutaneous tissue pedicle. The margins of the flap can be conservatively undermined to allow better mobilization and skin edge eversion during wound closure. The island flap is particularly useful for repair of defects adjacent to the nasal alae (see discussion in Chapters 6, 9, and 12). This area has a natural triangle shape, and part of the resulting scar will typically be in the melolabial crease.5

FIGURE 20-5 A, A 2.5 × 1.5-cm skin defect of medial cheek. V-Y subcutaneous tissue pedicle island advancement flap designed for repair. B, Flap dissected before transfer. C, Flap in place. D, Postoperative result at 5 months.
Medium-sized (2 to 3 cm) medial cheek cutaneous defects can be reconstructed by a number of different methods. Primary wound closure with extended incisions to remove standing cutaneous deformities may be used when defects are located near the border of the cheek aesthetic region. The surgeon may use asymmetric or differential undermining of the wound margins to position the wound closure suture line at or parallel to the border of the aesthetic region. This approach may provide excellent scar camouflage as the borders of the region are where natural shadows or lines of topographic transition occur. Primary wound closure is a particularly useful technique when defects are on or adjacent to the superior aspect of the melolabial fold (Fig. 20-6). When defects are not directly in the junction of the cheek with the lips or nose, the intervening skin may sometimes be excised to position the suture line in the aesthetic border of the medial cheek. Defects that are adjacent to the nasofacial sulcus are particularly amenable to primary wound closure (Fig. 20-7). In such cases, the skin lateral to the wound is advanced medially and anchored to the periosteum at the nasofacial sulcus by a 4-0 long-lasting absorbable suture. This may prevent effacement of the nasofacial sulcus and reduce wound closure tension.

FIGURE 20-6 A, B, A 3 × 2-cm skin defect of medial cheek involving melolabial crease. Wound closed primarily. Standing cutaneous deformity (broken line) excised in melolabial crease. C, D, Postoperative views at 7 months. Scar is in aesthetic boundary of melolabial crease. No revision surgery performed. (Courtesy of Shan R. Baker, MD.)

FIGURE 20-7 A, A 4 × 2-cm skin defect of medial cheek. Wound closed primarily. Anticipated standing cutaneous deformity marked with horizontal lines. B, Postoperative result at 2 months. (Courtesy of Shan R. Baker, MD.)
Transposition flaps are useful for repair of medium-sized defects of the medial cheek (Fig. 20-8). However, advancement flaps or rotation advancement flaps are easier to design and to dissect because of the considerable mobility of the skin of the medial cheek (Fig. 20-9). This mobility is related to the ample subcutaneous fat beneath the skin of the medial cheek. Although the type of flap selected depends on the position and size of the defect, flaps used to repair medial cutaneous cheek defects generally involve some component of pivotal and advancement motion (Fig. 20-10). As the diameter of the medial cheek defect increases, the length of the laterally based flap increases, resulting in a flap with more medial advancement and less pivotal movement (see Fig. 20-10). Regardless of the amount of rotation or advancement, it is essential to minimize an inferiorly oriented vector of tension that increases the risk of postoperative lower lid retraction (Figs. 20-11 and 20-12). The flap is typically undermined in the subcutaneous tissue plane, but SMAS flaps may also be elevated to correct contour defects or to reduce wound closure tension. When using any cheek flap to repair defects adjacent to the nose or lower eyelid, the surgeon must make several decisions about flap design. First, the surgeon must decide whether the tissue medial to the defect should be sacrificed to position incisions at the nasofacial junction (see Fig. 20-12). Widening the initial defect to the position of the nasofacial sulcus allows the standing cutaneous deformity that forms from advancement inferior to the defect to be excised in the melolabial crease. Another consideration is whether to excise eyelid skin to position the scar in a subciliary position (see Fig. 20-12). Placement of the incision in the subciliary line results in a less conspicuous scar and avoids persistent lower eyelid edema but requires the removal of normal eyelid skin. A disadvantage of advancing cheek skin to the level of the subciliary line is a greater risk of ectropion or inferior eyelid retraction, particularly in older individuals with poor muscle tone. The ability of the eyelid to tolerate scar contraction can be estimated by the snap test in a fashion similar to evaluation of the muscle tone of the eyelid before blepharoplasty surgery. The subciliary line is the preferred location for positioning of scars in younger patients because of the excellent scar camouflage it provides. Properly performed advancement flaps using suture suspension of the flap to the periosteum of the bony orbital rim rarely lead to problems with eyelid retraction. However, in older patients and patients with poor orbicularis muscle tone, the eyelid skin should not be excised. If in doubt, it is far better to preserve all of the skin of the eyelid and to attempt to position scars along the inferior bony orbital rim in the aesthetic border between the cheek and the eyelid. Some authors advocate routine lateral canthopexy to tighten the lower eyelid to prevent retraction when cheek advancement flaps are used to repair cheek defects in the vicinity of the lower eyelid.6 Regardless of incision placement, it is important to anchor the flap to the periosteum of the inferior bony orbital rim to prevent excessive downward traction on the eyelid. The superior medial tip of an advancement flap may be de-epithelialized and the peninsula of dermal tissue used to anchor the flap to the periosteum of the medial canthal region to provide additional medial support to the flap.



FIGURE 20-8 A, A 1.5 × 1.5-cm skin defect of medial cheek. Transposition flap designed for repair. Anticipated standing cutaneous deformity marked inferior and lateral to defect. B, Flap in place. C, Postoperative result at 2 months. (Courtesy of Shan R. Baker, MD.)
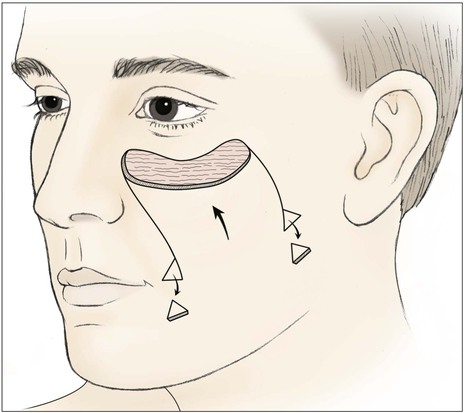
FIGURE 20-9 Unipedicle advancement flap designed to repair medial cheek defect. Standing cutaneous deformities excised at base of flap.
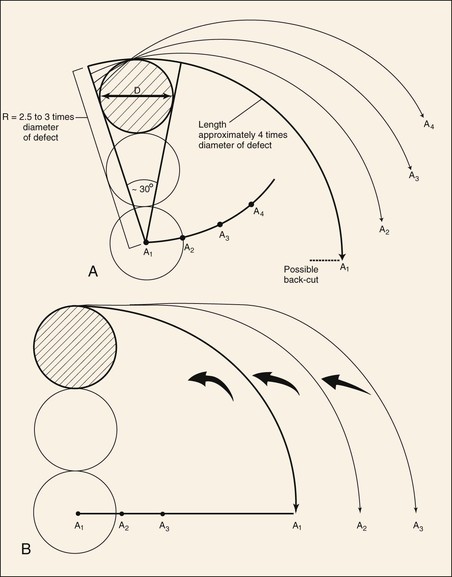
FIGURE 20-10 Dynamics of rotation advancement flaps. A, Rotation (pivotal) flaps are drawn using radius (R) that is 2.5 to 3 times diameter (D) of defect. Location of pivotal points (A1-A4) may be modified to cause flap design to change from pure pivotal (A1) to primarily advancement (A4). Note that as pivotal points progress from A1 to A4, base and tip of modified flaps become wider and flap is designed for greater advancement and less pivotal movement. B, If pivotal point (A1-A3) is moved on a line perpendicular to vertical axis of defect, flap will manifest greater advancement and less pivotal movement. (From Murakami CS, Nishioka GJ: Essential concepts in the design of local skin flaps. Facial Plast Surg Clin North Am 4:455, 1996.)

FIGURE 20-11 A, A 2 × 2.5-cm defect of medial cheek and eyelid. Rotation advancement flap designed for repair. B, Rotation advancement flap elevated in subcutaneous plane, with greater degree of advancement as flap is extended laterally toward preauricular crease. Flap reflected inferiorly. C, Flap in place. Standing cutaneous deformity at base maintained to optimize vascularity to distal aspect of flap. Deformity removed 2 to 3 weeks later. D, Postoperative result at 6 months.

FIGURE 20-12 A, A 4 × 3-cm medial cheek defect. Rotation flap designed for repair. Incision for flap placed in subciliary line. Nasofacial sulcus and melolabial crease marked. Skin between defect and nasofacial sulcus and melolabial crease removed to position advancing border of flap in aesthetic boundary. B, Incision for flap extended to preauricular crease and posterior auricular sulcus. Anticipated standing cutaneous deformity marked with horizontal lines on melolabial fold. C, D,
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








