Bilobe Flaps
Introduction
The original design of the bilobe flap is attributed to Esser,1 who described its use in 1918 for reconstruction of nasal tip defects. Zimany2 and others expanded the use of the flap to reconstruct defects on the trunk and soles. However, most authors now share the opinion that this flap is most useful for facial reconstruction, particularly of the nose.
Biomechanics
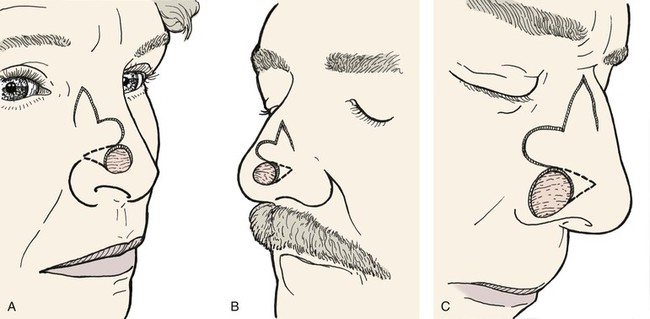
The bilobe flap would appear to be a modified rotation flap with some component of transposition. However, during transfer of the flap, there is noticeably less restriction of tissue movement than would be present with a pure rotation flap. This ease of tissue movement of the first lobe is the result, in part, of transposing the triangle-shaped peninsula of skin located between the defect and the first lobe of the flap. The transposition of this skin peninsula adjacent to the distal portion of the first lobe of the flap in essence represents a modified Z-plasty (Fig. 10-1). Likewise, there is a triangular peninsula of skin that forms between the first and second lobes that is also transposed during closure of the donor site of the second lobe. Thus, the bilobe flap in some ways represents a modified double Z-plasty. This results in repositioning of the skin adjacent to the defect and the two lobes of the flap. This in turn results in an overall reduction in wound closure tension compared with use of a single transposition or rotation flap.
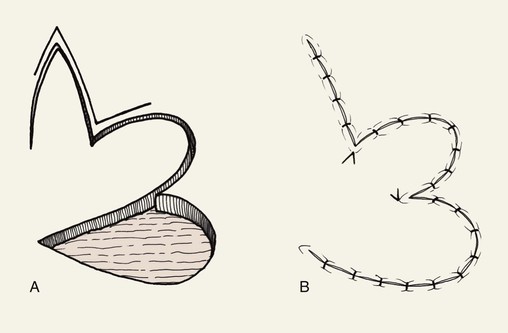
FIGURE 10-1 A, B, Bilobe flaps are modified Z-plasties that reposition skin adjacent to defect and two lobes of flap. This results in greater distribution of wound closure tension than with single-lobe transposition flaps.
Flap Design
McGregor and Soutar3 altered the design of bilobe flaps and noted that the degree of pivotal movement could be varied greatly from the original 90° between each lobe. In 1989, Zitelli4 published his experience using the bilobe flap for nasal reconstruction. He emphasized the use of narrow angles of transfer, 45° between each lobe, so that the total pivotal movement of tissue occurs over no more than 90° to 100°. This eliminated the need to excise standing cutaneous deformities, and trap-door deformities were frequently avoided. Burget5 confirmed the excellent results with this design for reconstruction of the nose. Other surgeons also advocated a similar design for repair of skin defects of the cheek, chin, and lips.6,7 They used narrow angles between the lobes of the flap and achieved better results than with use of traditionally designed bilobe flaps that are transposed through an arc of 180°.
Variations of the bilobe flap are useful. On the nose, the flap may be based medially, although it works best and is most often designed with a lateral base (Fig. 10-2). The lobes of the flap may be designed with rhombic shapes for smaller defects. Bilobe flaps may be used to repair large defects located on the cheek in lieu of larger cervical-facial rotation advancement flaps. They may also be used to transfer skin from the postauricular area to cover helical rim defects that might otherwise require skin grafting.
Clinical Applications
Cheek
The bilobe flap may be used to repair medium-sized (3-6 cm) skin defects of the cheek. It is particularly useful when simple rotation or transposition flaps will not provide sufficient tissue for repair. This occurs when the defect is large and located in the midcheek away from the central part of the face. In this situation, the amount of remaining adjacent cheek skin available for construction of a local flap may be insufficient to cover the cheek defect and still enable closure of the flap donor site. Instead, a bilobe flap designed to recruit upper cervical skin can be useful. Obviously, the lines of wound closure do not fall in RSTLs on the cheek, but the advantage of reducing wound closure tension outweighs the disadvantages of the curvilinear scar created by use of the flap. Like all transposition flaps, bilobed flaps take advantage of lax skin adjacent to the defect to assist in wound closure. The flap is designed to resemble a mitten (Fig. 10-3). The first lobe adjacent to the cheek defect is designed slightly smaller than the defect, and the second lobe is designed to be even smaller. The flap is raised in the subcutaneous tissue plane and transposed into position. The trick is to make sure the donor defect of the second lobe can be closed primarily. This is determined by the pinch test to see if the skin in the proposed area of the second lobe is sufficiently loose to permit primary wound closure. The test is accomplished by gathering the skin of the designed second lobe between the thumb and index finger. If sufficient skin laxity is present, the pinch test should enable the surgeon to approximate the anticipated borders of the second lobe defect.
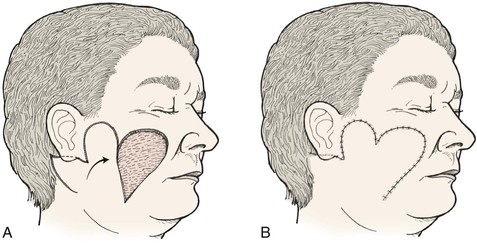
FIGURE 10-3 A, B, Bilobe flaps useful for repair of cutaneous cheek defects when simple rotation or transposition flaps will not provide sufficient tissue for repair.
Bilobed flaps may be used anywhere on the cheek; however, care should be taken in using the flap because not all the incisions required to create the flap lie parallel to the natural lines of the face, and the aesthetic result could be disappointing. The flap is best used to repair large to moderate-sized defects of the central cheek. In such cases, the remaining lateral preauricular skin is used to construct the first lobe, and the posterior auricular or superior cervical skin is the source of the second lobe.
Nose
The bilobe flap is well suited for reconstruction of the nose. Many surgeons with experience using bilobe flaps report that it is best suited for use on the caudal third of the nose. In one review of 400 nasal reconstructions, the bilobe flap was the most commonly used flap.4 With little wound closure tension on the first lobe, there is little or no distortion when the flap is used for repair of defects located near the alar rim, provided the first lobe is made sufficiently large. The use of skin adjacent to the defect allows excellent skin color and texture match. The donor site of the second lobe is closed primarily. This is possible because the second lobe is harvested from the lax skin of the upper dorsum and nasal sidewall, where primary approximation of the donor site of the second lobe can occur.
Bilobe flaps of the nose must be geometrically precise and are designed by the following method (Figs. 10-4 and 10-5).8
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree