Reconstruction of the Eyelids
Physiology of the Ocular Anterior Segment
Interruption of tear drainage from damage to the lacrimal outflow system is common after eyelid reconstruction. The lacrimal puncta are normally in contact with the ocular surface and eversion or ectropion may occur, especially with lower eyelid reconstruction. The lacrimal canaliculi connect the puncta with the lacrimal sac, located posterior to the palpable anterior limb of the medial canthal tendon. The upper and lower canaliculi are encased in fibers of the orbicularis oculi muscle, which insert onto the lateral wall of the lacrimal sac. Contraction of the orbicularis oculi during blinking pumps the tears into the lacrimal sac. From there, the tears drain to the inferior nasal meatus via the nasolacrimal duct through the maxilla. Surgery in the region of the medial canthus frequently results in epiphora caused by injury to the canaliculi, the lacrimal sac, or the orbicularis oculi fibers that form the lacrimal pump. Primary repair of the canaliculi is obligatory when trauma or tumor excision results in their interruption.
Surgical Anatomy of the Eyelids
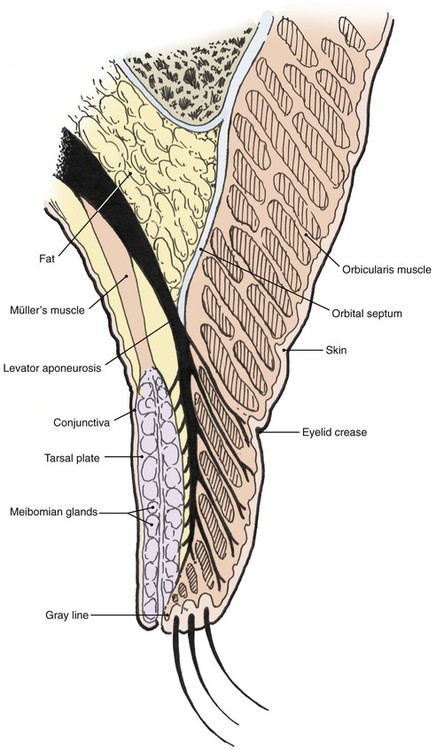
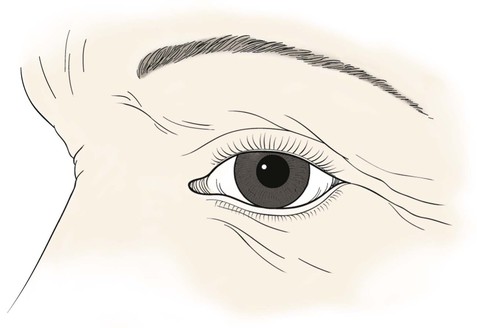
The multilaminar structure of the eyelids varies according to distance from the palpebral fissure. For the upper eyelid below the lid crease, the layers include the epidermal skin with minimal dermis, orbicularis oculi muscle, levator aponeurosis, tarsus, and conjunctiva. Above the lid crease, the layers include skin, orbicularis oculi, orbital septum, orbital fat, levator aponeurosis, Müller’s muscle, and conjunctiva (Fig. 17-1).
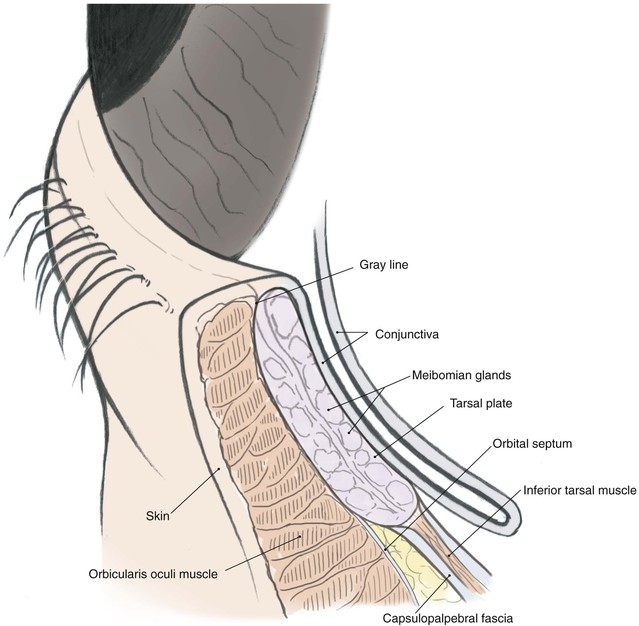
The lower eyelid has similar structures, except that the retractor (analogous to the levator muscle) is the capsulopalpebral fascia. This fascia is an extension of the inferior rectus muscle sheath that inserts at the inferior border of the lower eyelid tarsus and causes passive downward movement of the lower eyelid in downward gaze. A sympathetically innervated inferior tarsal muscle analogous to Müller’s muscle is also present in most individuals (Fig. 17-2).
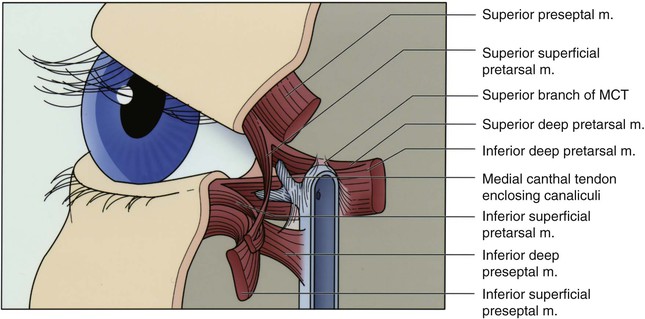
The lateral canthal tendon anchors the tarsal plates posteriorly and superolaterally to Whitnall’s tubercle inside the orbital rim. The lateral eyelids are thus kept snugly against the globe in all positions of gaze. Medially, the medial canthal tendon is the centerpiece of medial canthal anatomy. The medial canthal tendon has an elastic lateral portion that supports the lacrimal canaliculi and then splits into anterior, superior, and posterior limbs, all of which blend with the lacrimal sac fascia.1 The thick anterior limb inserts on the maxillary bone, and the superficial preseptal orbicularis muscle fibers insert on the anterior limb (Fig. 17-3). The superior branch extends to the lacrimal sac apex and covers the anterosuperior portion of the lacrimal sac.2 The thin posterior limb forms the anterior fascia of the pretarsal orbicularis muscle and inserts on the posterior lacrimal crest formed by the lacrimal bone. It acts as a horizontal supporting band that posteriorly directs forces generated by the pretarsal muscle fibers. The lateral portion of the medial canthal tendon invests the fragile lacrimal canaliculi. Reconstruction at either canthus must re-create the deep attachments of the canthal tendons inside the orbit to avoid symptomatic eyelid malpositions.
The tarsal plates are composed of dense connective tissue and house the meibomian glands that produce oil for the tears. The upper eyelid tarsus is 10- to 12-mm in height and tapers medially and laterally. It is 16- to 20-mm in length and approximately 1-mm thick. The lower eyelid tarsus is 4- to 5-mm in height but similar in length and thickness to the upper tarsus. Both are anchored medially and laterally to the orbital rim by the canthal tendons, as described before. The posterior surface in each case is lined with densely adherent conjunctiva.
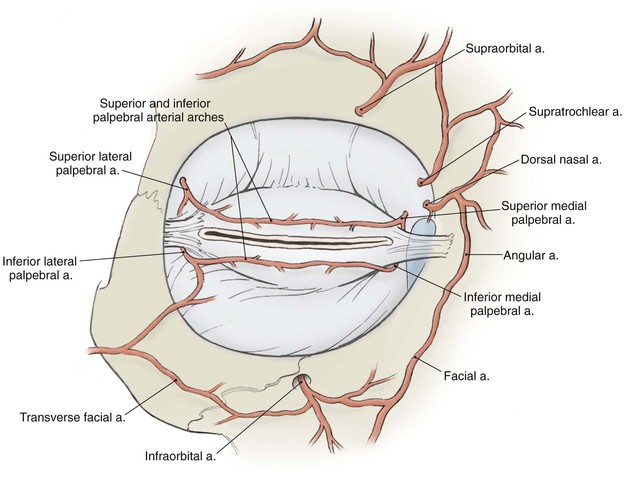
The vascular supply to the region comes from the internal and external carotid systems. Branches from the ophthalmic artery in the posterior orbit pass forward as the anterior ciliary arteries and contribute to the superior and inferior tarsal arcades in the eyelids (Fig. 17-4). Branches from the facial artery supply the medial and lateral canthus and also contribute to the eyelid vascular arcades. Risk of eyelid vascular compromise exists if the arteries are interrupted both medially and laterally.
Anesthesia
Topical tetracaine 1% or proparacaine 0.5% eye drops are used to anesthetize the ocular surface and are repeated as needed for patient comfort. Frequent lubrication of the cornea with ophthalmic petrolatum ointment or hydroxypropyl cellulose eye drops will also improve patient comfort during and after surgery.
Reconstructive Objectives
1. Nonkeratinizing mucosal epithelium to line the inside of the reconstructed eyelid to protect and to wet the cornea
2. Rotationally stable eyelid margin with a mucocutaneous junction to protect the eye from skin, lanugo hairs, and lashes
3. Posterior apposition to the globe in all areas of the reconstructed eyelid
4. Moderately flexible, firm connective tissue frame to provide support and shape for the eyelid
5. Adequate protractor muscle to close the eyelids, to provide a normal blink, and to assist in posterior apposition of the eyelid to the eye
6. Lack of orbital septal contracture or attachments that restrict eyelid excursion
7. Supple, thin skin that permits normal eyelid excursion
8. Adequate levator muscle function to provide upper lid clearance of the pupil
9. Appropriate height and shape of the reconstructed eyelid and the medial and lateral canthi to maintain symmetry with the contralateral side
The single most useful reconstructive strategy to achieve most of these objectives is conversion of vertical surgical tension to horizontal tension in the eyelids whenever possible.
Surgical planning is facilitated by conceptually dividing the eyelids into anterior and posterior lamellae. The anterior lamella is composed of the skin and the orbicularis muscle; the posterior lamella is composed of the conjunctiva, tarsus, and eyelid retractors. For full-thickness defects, both lamellae usually require reconstruction. In these cases, at least one of the reconstructed lamellae typically must include a blood supply. Commonly used, reliable surgical techniques are listed in Tables 17-1 and 17-2 and involve various flaps and grafts. Selection will depend on the size, location, depth, and configuration of the defect. Some superficial defects may require only reconstruction of the anterior lamella, and choice of flap or graft is primarily dependent on the need to restore a mobile, cosmetically satisfactory eyelid or to restore normal canthal position. When necessary, reconstruction of the lacrimal tear drainage system is accomplished concomitantly.
TABLE 17-1
Algorithm for Full-Thickness Lower Eyelid Reconstruction
| Size of Eyelid Margin Defect (eyelid width) | Repair |
| <25% | Direct closure |
| 25%-50% | Direct closure with lateral cantholysis |
| 25%-80% | Tarsoconjunctival graft and skin-muscle flap |
| 33%-66% | Semicircular flap |
| 50%-75% | Semicircular flap with periosteal flap |
| 50%-100% | Tarsoconjunctival flap and skin graft |
Algorithm for Full-Thickness Upper Eyelid Reconstruction
| Size of Eyelid Margin Defect (eyelid width) | Repair |
| <25% | Direct closure |
| 25%-50% | Direct closure with lateral cantholysis |
| 25%-50% | Tarsal rotation flap and skin-muscle flap or skin graft |
| 25%-75% | Tarsoconjunctival graft and skin-muscle flap |
| 33%-66% | Semicircular flap with periosteal flap |
| 50%-100% | Cutler-Beard flap |
Relaxed Skin Tension Lines
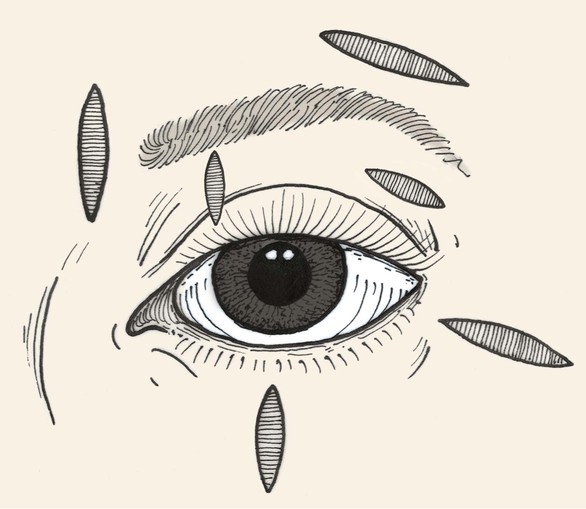
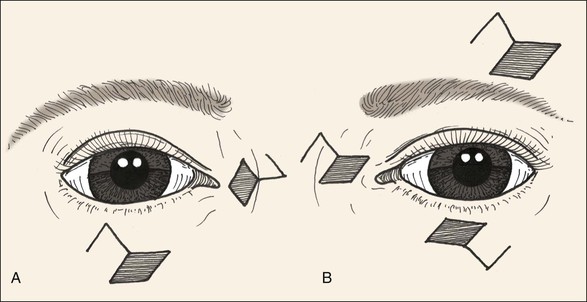
Relaxed skin tension lines (RSTLs) are a generally useful guide for the reconstructive surgeon in the attempt to minimize cutaneous scars.3 Around the eyes, these lines follow the lines of facial expression (Fig. 17-5) and are oriented horizontally in the upper and lower eyelid skin. Unfortunately, vertical tension created by closure of elliptical defects oriented along RSTLs in the eyelids has a substantial risk of creating iatrogenic cicatricial eyelid malpositions, including retraction and ectropion. Asymptomatic laxity in the medial and lateral canthal tendons, commonly present in the elderly, will permit downward migration of the lower lids. Similarly, ineffective senescent or neuropathic orbicularis muscle tone will predispose patients to lower eyelid ectropion or upper eyelid retraction and lagophthalmos. For these reasons, horizontal tension is usually preferred for closure of eyelid wounds, and the long axis of any ellipse will be perpendicular to the eyelid margin (Fig. 17-6). Excessive dermatochalasis in the upper eyelid that would otherwise require blepharoplasty may permit the use of horizontally oriented ellipses in the lid crease for some individuals. Conversely, for the glabella, medial canthus, eyebrows, and lateral canthus, use of RSTLs for wound orientation will produce satisfactory outcomes (see Fig. 17-6).
Local Skin Flaps for Superficial Defects
The simple ellipse is often used for excision of small facial lesions, including those in the periocular area. Whereas the long axis of such an ellipse is usually oriented parallel to RSTLs, ellipses are oriented perpendicular to RSTLs in the eyelids to minimize vertical tension and the risk of cicatricial ectropion. Because the ellipse sacrifices up to 160% of the surface area of the excised lesion of interest, modified ellipses such as the double S ellipse and O-Z plasty can be used to conserve normal tissue (Fig. 17-7).
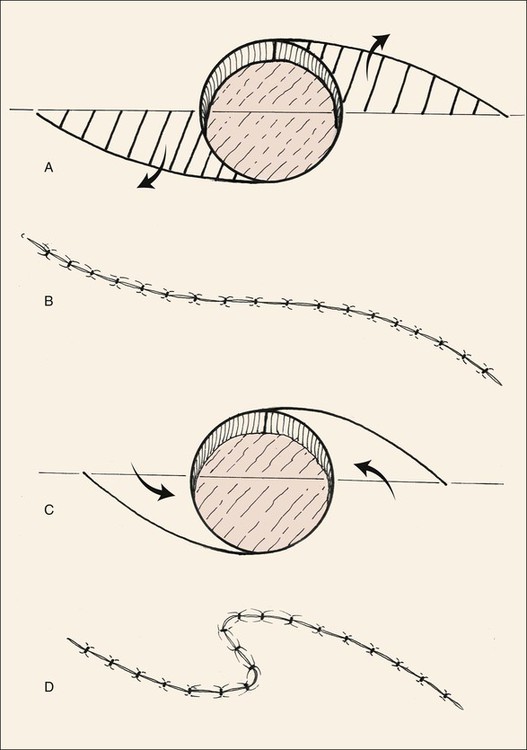
FIGURE 17-7 A, S-shaped ellipse in which alternate halves of ellipse are excised (lined area), sacrificing less normal tissue. B, Wound is closed in O-to-S plasty. C, O-to-Z plasty. Curved incisions are made from opposite tangents of circular defect. D, Wound closure assumes Z configuration.
Local skin flaps are preferred to free skin grafts for reconstruction of anterior lamellar defects in the periocular region for many reasons.4 Adjacent skin usually provides a better texture and color match than with grafts from distant sites, and flaps undergo substantially less contraction during healing. In addition, the rich vascular supply in the region permits the use of flaps that would be more tenuous in other parts of the body. Furthermore, the ample vascular supply of local flaps can be used to support free grafts for posterior lamellar reconstruction. Prior irradiation or multiple prior surgeries may reduce local circulation.
Rhomboid transposition flaps are the most useful adjacent skin flap in the periocular area, especially for medial5 and lateral canthal defects. The principles of design can be found in Chapter 11 of this text. Specific to this region is the need to avoid distortion of the eyebrow, eyelid crease, eyelid margin, and canthal angles. Common flap designs are shown in Figure 17-8. The vector of maximal wound closure tension must be parallel to the lid margin in the lower lid and most commonly in the upper lid as well. Maximal tension may be vertical in the lateral and medial canthal regions, provided the canthal position is not changed.
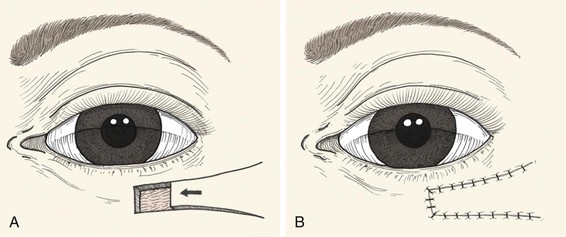
Other advancement and transposition flaps can be used to repair certain anterior lamellar defects (Figs. 17-9 to 17-12). Among those commonly used are the standard unipedicle and bipedicle rectangle-shaped advancement flaps and V-Y and Y-V advancement flaps. The unipedicle rectangular advancement flap is well suited to the region and can be used to close defects up to 25 cm2. Cutaneous defects of the eyebrow or the anterior lamella of the medial upper and lower eyelids can be repaired with this flap. The resulting scars fall into or parallel to the lid creases and avoid injury to the lid margin. V-Y advancement flaps can be used to lengthen the palpebral fissure or to close donor sites.6 Y-V advancement flaps are useful in the management of epicanthal folds7 and scar contractures.
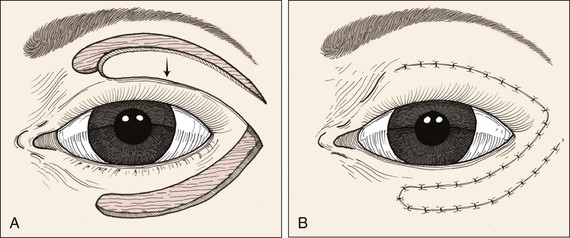
FIGURE 17-9 Transposition flap used to repair anterior lamellar defect of lower eyelid. Flap can be transferred as cutaneous or musculocutaneous flap.
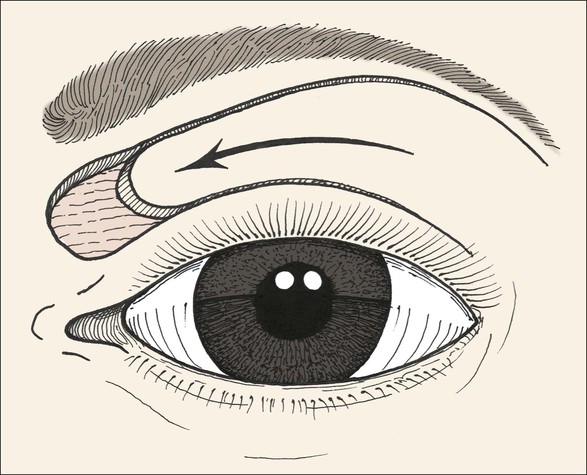
FIGURE 17-11 Musculocutaneous advancement flap used to repair medial upper eyelid defect. When it is combined with lower eyelid and cheek advancement flaps, large medial canthal skin defects can be successfully repaired.



FIGURE 17-12 Eyelid defect repaired with anterior lamella flaps. A, Lower eyelid and medial canthal defect. B, Defect closed with medial canthopexy to reinforce medial canthal tendon, rhombic flap from nose, and advancement flap from melolabial fold. C, Postoperative view at 1 year. Note maintenance of lower eyelid height.
Healing by second intention is generally not an accepted strategy for eyelid wounds because the incidence of cicatricial ectropion is substantial. However, in the medial canthus, healing by second intention (or laissez-faire) is more often successful,8,9 especially if the defect is 1 cm or less in diameter and centered between the upper and lower eyelids.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree