Re-Creating the Inframammary Fold: the Internal Approach
Scott L. Spear
Ali N. Mesbahi
Michael Beckenstein
It is easy to underestimate the importance of the inframammary fold in creating the appearance of an attractive breast. A well-defined and well-positioned inframammary fold can turn an amorphous mound into a pretty and natural-appearing breast. This topic went unaddressed until the late 1970s and early 1980s, when first Pennisi (1) and then Ryan (2) described their respective external approaches to re-creating a natural fold under a reconstructed breast. The external approach technique can be found in Chapter 41.
As breast reconstruction and breast augmentation have become more popular, additional techniques have been described with more emphasis on creating or re-creating a fold without an additional external incision at the level of the fold (3,4,5,6,7,8). Although most of the literature on this topic addresses creating a fold with an implant breast reconstruction, the inframammary fold may need to be created, raised, or lowered in conjunction with prosthetic breast reconstruction, breast reduction, and breast augmentation. Repositioning of the inframammary fold is addressed in the section on breast reduction. In this chapter, we describe the management of the inframammary fold in breast augmentation, prosthetic breast reconstruction, and autologous breast reconstruction.
Achieving symmetry in breast reconstruction requires matching the volume of the remaining breast, matching the position, creating a similar inframammary crease, and providing a comparable amount of skin on the reconstructed breast, particularly as measured from the new nipple to the new fold. In reconstruction with minimal or no ptosis or in breast augmentation patients where the fold has been surgically displaced inferiorly, the fold must be set at the desired level but not necessarily deepened as in a breast reconstruction in the patient with a pendulous breast. Re-creating or resetting the fold in the nonptotic patient resembles a capsulorrhaphy or capsulopexy as described by Spear in 1988 and Parsa in 1990, respectively. Where simply correcting the level of the fold is the mission, the procedure must focus primarily on achieving symmetry in the fold position. Deepening the fold and recruitment of upper abdominal skin to create ptosis in such patients is neither necessary nor desirable. Conversely, in reconstructing a pendulous breast, the exact height of the fold is of less importance than the overall appearance and silhouette of the breast because the reconstructed fold will probably not be seen in the upright position.
Reconstructing the fold after breast augmentation or after prosthetic breast reconstruction in the nonpendulous breast is quite similar. In either case, the normal inframammary crease has been destroyed by previous surgery that has included either a mastectomy or placing an implant below the level of the pre-existing fold. Reconstruction of the fold even in this setting requires an understanding that creating a fold requires the marriage of two flaps or planes of tissue that can also include some shifting of the overlying skin flap at the time it is attached to the underlying chest wall. Re-creating the fold thus requires planning at what level on the chest wall the new fold will be created and also at what level on the breast skin the attachment will be made. In some patients, the overlying skin may be tacked back directly and posteriorly, whereas in other patients the fold may be only slightly low, but the breast skin may have been severely stretched, creating the need to reduce the amount of skin on the lower breast. Less commonly, the fold may be quite low, but the amount of breast skin is not at all low or barely in excess. In such cases, the existing breast skin may need to be tacked, not straight back, but actually up to the desired fold level on the chest wall. This type of advancement or recruitment maneuver is similar to the procedure for re-creating the fold in a pendulous breast.
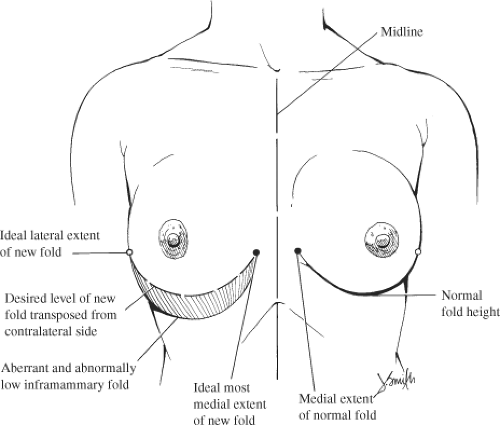
In the nonpendulous breast patient, planning the repair of the inframammary fold begins with a careful inspection of the patient and, if available, the photographs (Fig. 42.1). What is the vertical height disparity between the folds of the two sides? Are the other borders of the breasts proportionate? At what level and how far medially does the other fold begin? Mark on the patient the level of the normal fold on the normal side, including a mark for the point where it begins to deepen medially. Mark the midline. Mark the level of the aberrantly low fold on the side to be corrected. In bilateral cases, the normal fold must be estimated. Transpose the normal fold onto the side to be corrected. It should lie superior to the existing aberrant fold. On the aberrant side, mark the key point where the fold should first deepen medially. This point should lie equidistant from the midline as the key point on the normal side. The inframammary fold line transposed onto the abnormal side actually represents the desired level for the fold on the chest wall but not necessarily the ideal point on the skin for reattachment. Make note of the relationship between the proposed new fold and the pre-existing aberrant one. What is the maximum vertical shift necessary? Where do the two folds converge?
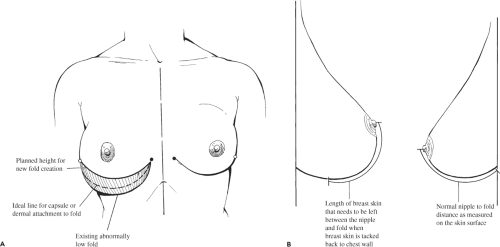
In the case of augmentation, now measure the distance from the nipple to the fold on the normal side and from the nipple to the proposed new fold on the abnormal side. This measurement can be made using a flexible or cloth tape measure in the upright patient or a ruler in the supine patient. Most of the time, these measurements will be equal on the two sides, but occasionally the abnormal side’s proposed fold line will leave either too much or too little skin on the breast if this line on the skin is tacked directly posteriorly to the new line on the chest wall. In those unusual circumstances, an additional line must be drawn on the abnormal side corresponding to how much breast skin must be left on the side to be corrected (Fig. 42.2). Marking three points can create this curved line: the medial and lateral end points of the proposed new fold and the ideal vertical skin length between the nipple and the new
fold. Where the breast skin has ballooned out, this additional curved line will be drawn above the proposed new fold line but will join it at the medial and lateral extremes. Where there is scant breast skin, this line will actually lie below the proposed new fold line; something that almost never happens in breast augmentation.
fold. Where the breast skin has ballooned out, this additional curved line will be drawn above the proposed new fold line but will join it at the medial and lateral extremes. Where there is scant breast skin, this line will actually lie below the proposed new fold line; something that almost never happens in breast augmentation.
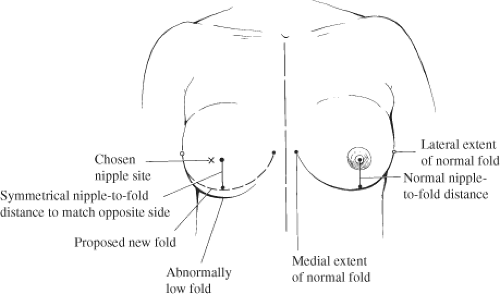
This planning technique is admittedly more difficult in breast reconstruction where the nipple landmark is absent on the reconstructed side (Fig. 42.3). However, the planning is otherwise nearly identical. The only difference is that the nipple site must be chosen on the reconstructed breast before the nipple-to-fold distances can be measured, equalized, and then
drawn. It is just as important in breast reconstruction as in augmentation that the skin available on the lower pole of the breast beneath the nipple be equalized at the same time as the inframammary folds are equalized.
drawn. It is just as important in breast reconstruction as in augmentation that the skin available on the lower pole of the breast beneath the nipple be equalized at the same time as the inframammary folds are equalized.
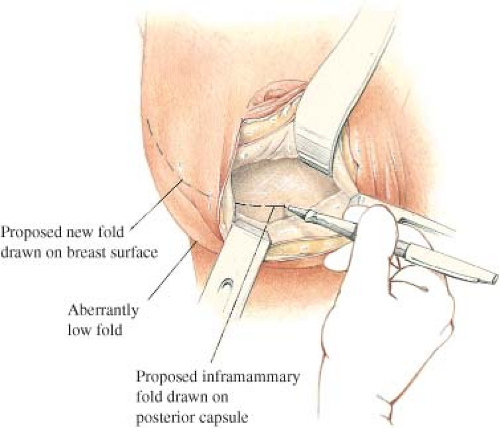 Figure 42.4. The desired fold height is drawn on the chest wall or posterior capsule surface to mimic the desired fold height drawn on the skin.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|