Radial Forearm Free Flap in Intraoral Reconstruction
D. S. SOUTAR
I. A. McGREGOR
EDITORIAL COMMENT
Postoperatively, the radius must be protected from undue stress because the incidence of fracture can be significant when a segment of the radius has been removed with the flap. The ulnar artery version of the forearm flap has not been included in the Encyclopedia because the safety of this flap is still being debated.
The radial forearm flap is a fasciocutaneous flap based on the radial artery and venae comitantes, together with the subcutaneous forearm veins. Several reports (1, 2, 3, 4, 5) already have demonstrated the versatility, usefulness, and reliability of this flap both as a pedicled flap in reconstructive surgery of the hand and as a free flap in the expanding field of free tissue transfer. This flap can be used as either a fasciocutaneous flap or as an osteofasciocutaneous flap (6, 7) for reconstructing defects resulting from excision of intraoral malignancies.
INDICATIONS
Resection techniques that preserve all or part of the mandible and reconstructive techniques that aim to restore mandibular continuity result in smaller intraoral defects. Such defects do not readily accommodate large bulky flaps without distorting the oral cavity and disturbing oral function and competence.
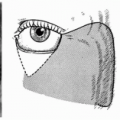
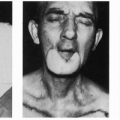
The radial forearm flap offers thin, pliable predominantly hairless skin that is well suited to replace oral mucosa following tumor excision. The flap readily conforms to the varying contours within the oral cavity and subsequently settles remarkably quickly, showing little or no evidence of contracture or “pin-cushioning” (Fig. 202.8). This may be related to the presence of the deep fascia on the undersurface of the flap that, perhaps, does not contract to the same degree as subcutaneous fat.
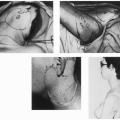
Bone may be included as an osteocutaneous flap to reconstruct the mandible and oral mucosa in a single stage (see Fig. 202.9). The fascial attachment of skin to bone allows a mobility of the skin that simplifies closure of the oral mucosa.
The donor defect is relatively painless, even in patients from whom bone has been removed. This causes the patient minimal discomfort in the early postoperative period, thus facilitating recovery and early mobilization. In the longer term, skin grafts on the forearm appear to give a satisfactory cosmetic result, particularly in elderly patients.
ANATOMY
Much of the skin of the forearm is supplied by the radial artery, which is covered proximally by the fleshy belly of the brachioradialis. It soon emerges distally between the brachioradialis and the flexor carpi radialis to lie superficially, covered only by skin, subcutaneous tissue, and the deep fascia.
The artery, together with its two venae comitantes, is invested in a condensation of the deep fascia known as the lateral intermuscular septum (Fig. 202.1). This septum separates the flexor and extensor compartments of the forearm and is attached to the periosteum of the radius distal to the insertion of pronator teres.
The artery gives off branches that pass through the deep fascia to supply the underlying flexor muscles and branches that spread out on the deep fascia to form a fascial plexus and
supply the overlying skin. By means of this vascular network, the radial artery can supply the skin of the palmar and radial aspects of the forearm and provide a periosteal blood supply to the distal radius.
supply the overlying skin. By means of this vascular network, the radial artery can supply the skin of the palmar and radial aspects of the forearm and provide a periosteal blood supply to the distal radius.
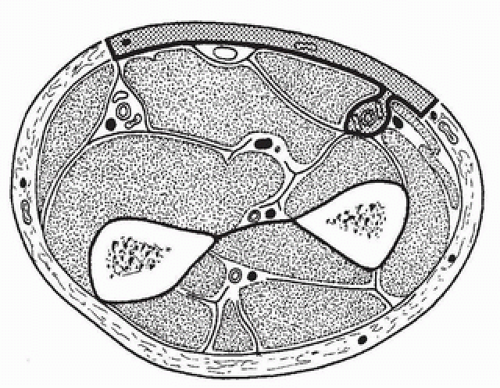 FIGURE 202.1 Fasciocutaneous flap. Cross section through the forearm distal to pronator teres showing the position of the radial artery and the plane of dissection for elevation of the fasciocutaneous flap. (From Soutar et al., ref. 7, with permission.) |
Venous drainage of the forearm flap is provided by two venae comitantes that accompany the artery and a variable pattern of subcutaneous forearm veins that drain into the cephalic, basilic, and median cubital veins. Routinely, both venous systems communicate by means of a constant branch from the venae comitantes, which drains into the median cubital vein.
The forearm flap is ideally suited for free-tissue transfer because the artery can be readily palpated for much of its length and the superficial subcutaneous veins of the forearm are easily identified. The diameter of the artery, usually in excess of 3 mm, remains relatively constant from its origin to the wrist joint, making anastomosis of either proximal or distal ends equally straightforward. Furthermore, the absence of significant arterial disease, particularly atheroma in elderly patients, has been most remarkable.
FLAP DESIGN AND DIMENSIONS
Using a template, a radial forearm flap can be designed to replace the amount of resected tissue accurately, thereby minimizing distortion and functional disturbance within the oral cavity. The radial artery, which is subcutaneous for much of its length in the forearm, can be palpated and its course marked on the skin surface. The superficial subcutaneous forearm veins are similarly marked, and the appropriately designed flap is outlined.
The arteriovenous system on which the forearm flap is based is capable of supplying all the skin of the forearm from above the elbow to the wrist, except for a narrow strip overlying the ulna posteriorly. In practice, such large flaps are not required in intraoral reconstruction.
The quality of the skin and the length of the vascular pedicle required for easy anastomosis most often influence the choice of donor site. The presence and distribution of hair on the forearm may influence site selection (Fig. 202.2), although such hairs tend to be short and fine and cause little trouble following flap transfer.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree