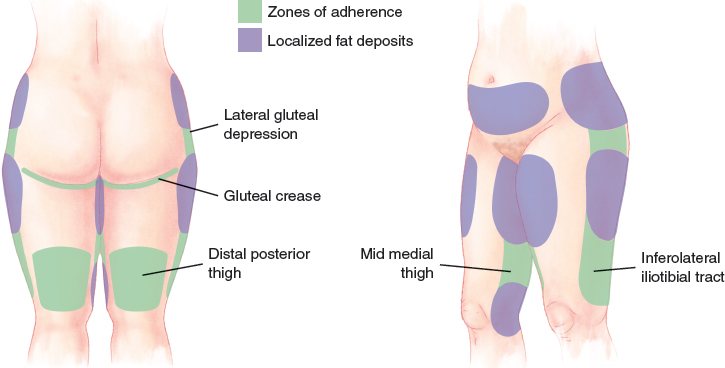
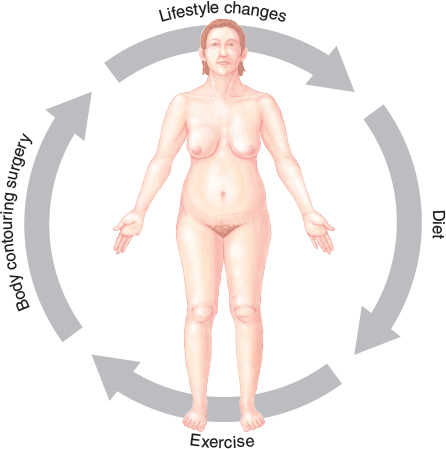
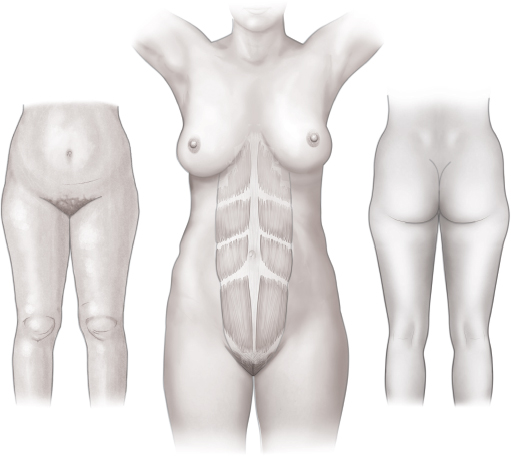
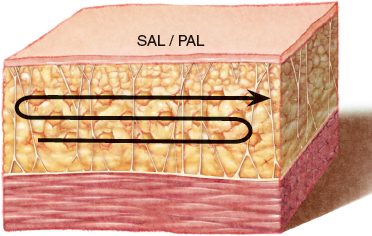
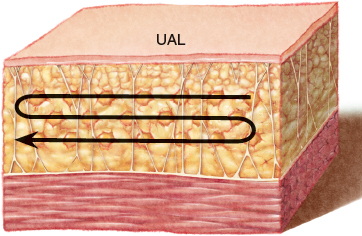
CHAPTER 11 An appreciation of the aesthetically pleasing human silhouette is fundamental. The aesthetically pleasing female silhouette has a concavity below the rib cage that changes to a convexity over the hips and thighs. The anterior and posterior thighs should have a shallow, convex arc. The female buttock crease should extend in a curvilinear fashion (round) to blend with the lateral thigh. The female abdomen should be concave in the epigastrium, with a smooth transition to a convex lower abdomen. The aesthetically pleasing male silhouette tends to be more linear, with only relative concavities in the pelvic region and convexity in the buttocks area (square). The flanks taper from the lower ribs to the iliac crest, and the buttock crease is more angular and square. The anterior infraumbilical region should be flat rather than convex. The surgeon’s ability to perform liposuction relies on having sound knowledge of the three-dimensional anatomy of the fat layers. Although anatomic structures such as Scarpa fascia in the abdomen or the superficial fascial system in the proximal thigh exist, it is more practical to view the subcutaneous adipose tissue layers as superficial, intermediate, and deep thirds when performing body contouring with liposuction. In most patients liposuction should be performed on the intermediate or deep adipose tissue layers. In fact, preservation of the superficial adipose tissue layer is crucial to preventing complications, including dimpling, waviness, hyperpigmentation, burns, and other contour irregularities. The deep adipose tissue layer lies just superficial to the investing fascia covering the underlying muscle and is composed of loose, less compact fat, which can often be safely aspirated without creating any contour irregularities. A notable exception to this rule is the deep fat within the buttocks. This area is more flaccid and prone to undesirable skin ptosis if this deep fat is removed. The superficial adipose tissue layer abuts the dermis and is composed of more dense, tightly adherent fat and thus presents the highest risk of complications when treated with liposuction. In patients with good skin quality, the rule is to maximally preserve the superficial adipose tissue layer. Treatment in the superficial layer should be performed with very specific objectives. For example, if there is a distinct contour problem, such as noticeable dimpling or slight to moderate skin redundancy, the use of ultrasound-assisted liposuction at a diminished power level with a blunt-tipped cannula can improve results by enhancing skin contraction, resulting in improved contour. The ultrastructure of the subcutaneous tissue layers can be characterized as a superficial layer composed of dense fat lobules among numerous fibrous septa and a deeper adipose layer of amorphous, irregular fatty pockets. In the abdomen, Scarpa fascia separates these two layers from one another, whereas in the thigh they are separated by the superficial fascial system. The superficial fascial system sends elements through the deep compartment, attaching to the investing fascia of the underlying musculature. These extensions become dense at the zones of adherence, where the superficial subcutaneous plane is adherent to the underlying investing fascia. The zones of adherence exist where there is minimal or no deep fat layer, and the superficial fat layer and its overlying dermis are thin. These zones are more susceptible to contour deformities. The zones of adherence in the waist and thighs include the gluteal crease, lateral gluteal depression, middle medial thigh, inferolateral iliotibial tract, and distal posterior thigh. These zones accentuate localized fat deposits between them. In the trunk men tend to accumulate weight in the flank, the area immediately superior to the iliac crest, whereas women tend to carry excess fat over the iliac crest area. In men a zone of adherence lies along the iliac crest and defines the inferior margin of the flank. In women the zone lies within the gluteal depression overlying the greater trochanter, allowing a cascade of fat to occur over the iliac crest. In general, aggressive liposuction of the zones of adherence should be avoided. However, if necessary, liposuction of the zones of adherence should be performed with small (less than 3 mm) cannulas at low-pressure suction. In 2004 the Committee on Patient Safety of the American Society of Plastic Surgeons published the first “Practice Advisory on Liposuction” (subsequently updated in 2009) to help guide the appropriate selection and treatment of patients seeking liposuction. Liposuction is very effective for the treatment of localized fat deposits, particularly of the trunk and thighs. In certain patients liposuction can be useful to contour other areas, including the chest, breasts, arms, and neck. Patients should generally be healthy and have a commitment to long-term positive lifestyle changes, including both healthy diet and exercise, to achieve the greatest long-term result after body contouring. A physical examination should be conducted with specific attention to skin tone and quality, the presence of scars, hernias, asymmetries, dimpling or cellulite, location of fat deposits, areas of adherence, and perceived deviations from the ideal sexspecific contour. One useful test to determine whether liposuction will be adequate or an excisional body contouring procedure is required is attempting to grasp the area of concern. Skin in areas amenable to liposuction can only be pinched, whereas skin that can be grasped is generally treated best with an excisional body contouring procedure. Specific anatomic areas and problems are best treated with certain liposuction cannulas. For infiltration, cannulas are typically smaller in diameter (1 to 3 mm), with blunt tips. Infiltration cannulas are available in several lengths. In general, shorter cannulas are less prone to bending and offer more control. The type of aspiration cannula will depend on the liposuction modality that is used. A multitude of aspiration cannulas ranging in diameter, length, and tip design are available. The diameters of aspiration cannulas typically range from 2 to 10 mm for suction-assisted liposuction. For ultrasound-assisted and power-assisted liposuction, the diameters of aspiration cannulas range from 2 to 6 mm. Aspiration cannulas are available in various lengths. Myriad tip designs are available, including both blunt and sharp tips. The number, characteristics, and positions of the tip ports can also vary greatly. Each cannula has particular advantages suited to a specific liposuction modality and should be used to achieve a specific treatment goal. For example, a 4 mm diameter three-port Mercedes tip aspiration cannula is well suited for power-assisted liposuction of most areas of the trunk and thighs. However, treatment of the zones of adherence requires the use of aspiration cannulas less than 3 mm in diameter to prevent overtreatment of these areas. A variety of liposuction modalities and their proposed advantages and disadvantages have been described, including suction-assisted liposuction, ultrasound-assisted liposuction, power-assisted liposuction, syringe-assisted liposuction, laser-assisted liposuction, and water-assisted liposuction. However, suction-assisted liposuction, ultrasound-assisted liposuction, and power-assisted liposuction have the longest track record and are suitable for most applications. Suction-assisted liposuction (SAL) was the first modality described and remains the most commonly used method. SAL removes adipocytes and other tissue through mechanical avulsion by the cannula tip combined with a negative pressure suction. SAL has been described for the treatment of localized fat deposits that have proved unresponsive to diet and exercise in virtually all areas of the body. SAL is performed starting with larger diameter cannulas (4 to 6 mm) in the deep and intermediate adipose tissue layers and transitioning to smaller diameter cannulas (2 to 3 mm) if the treatment of the superficial adipose tissue layer is necessary. Ultrasound-assisted liposuction (UAL) has undergone many refinements since its introduction by Zocchi in 1992. UAL uses ultrasound energy delivered by the cannula tip to cause cavitation of adipocytes, facilitating aspiration. The application of ultrasound energy may also contribute to skin tightening in the treatment area and supporting structures. UAL is particularly advantageous in patients with diminished skin tone, in liposuction of fibrous areas such as in the treatment of gynecomastia, and during secondary liposuction. UAL requires a three-stage technique. During the first stage, room-temperature solution is infiltrated into the intermediate adipose tissue layer in a 1:1 ratio of infiltrate to estimated total aspirate volume. In the second stage, Power-assisted liposuction (PAL) uses the reciprocating motion of the cannula to facilitate fat removal through mechanical avulsion by the cannula tip combined with negative pressure suction. The tip oscillates within a distance of approximately 2 mm. In addition, PAL can be used without the negative pressure suction to create small in situ fat grafts that can be either aspirated or redistributed as necessary to improve contour. Several studies comparing PAL with SAL have shown that this modality results in less operator fatigue and provides a faster rate of fat aspiration. PAL is particularly advantageous in large-volume liposuction; it can help reduce operator fatigue and treat fibrous areas, such as in gynecomastia surgery and secondary liposuction. In patients undergoing secondary liposuction, PAL can be applied to release scarred areas, redistribute existing fat, and harvest large volumes of fat for transfer to other areas. Liposuction can be performed with local or general anesthesia. However, several tenets should help guide the appropriate choice of anesthetic. Small-volume liposuction (less than 1 L) can be safely performed with an infiltration solution containing a local anesthetic and additional sedation if needed. However, general anesthesia may be preferable and more comfortable for patients in more extensive, complex, large-volume or combination procedures, with an emphasis on endotracheal intubation if the patient will be placed in the prone position. Both epidural and spinal anesthesia should be avoided because of the potential for vasodilation and hypotension, leading to the need for aggressive fluid resuscitation and resultant fluid overload. In most patients liposuction involves the removal of less than 5 L of total aspirate and can be safely performed as ambulatory surgery. In the past, large-volume liposuction (greater than 5 L of total aspirate) was more commonplace. However, because of the increased risks of fluid shifts and lidocaine toxicity with large-volume liposuction, ASPS recommends that large-volume liposuction should be performed in an appropriate health care facility with overnight monitoring of postoperative vital signs and urine output. In addition, the concentration of lidocaine in the infiltration solution may need to be decreased, particularly in obese patients (BMI greater than 30), to avoid the risk of lidocaine toxicity. In some patients it may be more reasonable to stage procedures to avoid unnecessary risk from combining large-volume liposuction with other procedures. During liposuction, fluid shifts can manifest in both extremes of fluid status: hypovolemia resulting from underresuscitation or pulmonary edema and/or congestive heart failure resulting from overresuscitation. Communication with the anesthesia provider throughout the procedure will ensure optimal fluid resuscitation. If necessary, urine output can be monitored with a Foley catheter. Four crucial elements should guide intraoperative resuscitation: intravenous fluid maintenance (body weight dependent), third space losses, the volume of the wetting solution infiltrated, and the volume of total aspirate. When large-volume liposuction is performed, the following guidelines should be used to ensure optimal resuscitation: 1. Preoperative fluid losses should be replaced as needed at the discretion of the surgeon and anesthesiologist. 2. Maintenance intravenous fluids and fluid boluses should be administered during surgery based on the patient’s vital signs and urine output. 3. A superwet technique should be used. 4. An additional 0.25 ml of Ringer’s lactate solution should be given during surgery for every 1 cc of total aspirate. Liposuction was originally performed with a dry technique without the use of any infiltration solution. However, 20% to 45% of the aspirate was composed of blood, and this approach was quickly replaced by the wet, superwet, and tumescent techniques that use infiltration solution for anesthesia and hemostasis. The use of infiltration solution has dramatically improved the safety of this procedure and allowed for liposuction of larger volumes with reduced blood loss. Table 11-1 Estimated Blood Loss With Different Infiltration Solutions
Principles of Liposuction
Adipose Tissue
THE AESTHETICALLY PLEASING SILHOUETTE
THE ADIPOSE TISSUE LAYERS
THE ZONES OF ADHERENCE
Indications
Preoperative Planning and Preparation
LIPOSUCTION CANNULAS
LIPOSUCTION MODALITIES
Suction-Assisted Liposuction
Ultrasound-Assisted Liposuction
Power-Assisted Liposuction
Surgical Technique
ANESTHESIA
Liposuction Infiltration Solution
Infiltration Solution | Estimated Blood Loss (Percent of Total Aspirate Volume) |
Dry | 20 to 45 |
Wet | 4 to 30 |
Superwet | 1 |
Tumescent | 1 |
We prefer to perform liposuction with a superwet technique and typically use an infiltration solution in a 1:1 ratio to the estimated total volume of aspirate. The infiltration solution is composed of 30 ml of 1% lidocaine, 1 ml of 1:1000 epinephrine, and 1 L of Ringer’s lactate crystalloid for the first 5 L of infiltration. For infiltration volumes greater than 5 L, the infiltration solution is made without lidocaine to prevent lidocaine toxicity.
 Jamil Ahmad Frank Lista
Jamil Ahmad Frank Lista  Rod J. Rohrich
Rod J. Rohrich