(1)
Klinik für Plastische Gesichtschirurgie, Marienhospital Stuttgart, Stuttgart, Germany
Electronic supplementary material
The online version of this chapter (doi:10.1007/978-3-662-49706-7_1) contains supplementary material, which is available to authorized users.
Keywords
SeptoplastySeptal reconstructionSeptal extension graftSeptal exchange techniqueExtracorporeal septal reconstruction1.1 Surgical Principles in Primary Septoplasty
The septum is the central part of the framework of the nasal skeleton. It is partially cartilaginous, partially bone. It is also perhaps the most underestimated and neglected structure of the nose. In a review of 469 of our own rhinoplasties performed in 2009, 198 procedures were found to be revision cases. One hundred and fifty-three of these revision cases (77.2 %) required surgical correction of a residual septal deformity that created a negative functional and aesthetic outcome. And whereas the functional importance of the nasal septum is often appreciated, its importance to the aesthetic outcome of surgery is often greatly underappreciated. As a consequence, failed cosmetic and functional surgeries are increasingly common.
Only a straight septum will permit the nose itself to remain straight. This is particularly true for the so-called septal “L-strut,” the L-shaped outer septal perimeter composed of both the dorsal and caudal segments. Unfortunately, the technical solutions and advice given in textbooks for septoplasty are often difficult to translate into reliable clinical results. For example, the scoring technique as well as the expectation that the scoring technique will keep a septum straight by releasing the unbalanced tension lines often does not work. Therefore, in addition to straightening the septum, it must also be properly supported and secured after scoring. For this reason, in all cases in which we release the septum from the premaxilla, for example, to take out a spur or to shorten the vertical length of the caudal septum, we make a drill hole through the anterior spine (Fig. 1.1a) and fix the caudal septum with at least three stitches to keep the cartilage anchored to different parts of the spine (Fig. 1.1b). Moreover, if we feel that scoring will help to straighten the septum, we always apply a splint of ethmoid bone to keep the scored cartilage straight during the healing process (Fig. 1.2).
Following the classification of Bahman Guyuron, the ultimate objective is a straight septal framework. If the central part is bent but the L-strut is still straight, it is relatively easy to remove the deviated segment, straighten it, and put it back. However, if the dorsal strut is straight but the caudal septum is deflected (i.e., the L-strut is bent), it may be difficult to achieve a completely straight septum without reconstructing the L-strut. There are two options to solve this problem: a less difficult one that preserves the straight part and takes out only the deformed segment (Fig. 1.3; see Case 3) or a more complicated procedure that involves taking out the entire septal framework, called an extracorporeal septal reconstruction (Fig. 1.4). The latter option means that the whole septum is removed, preferably with the bony and the cartilaginous segments in one piece. By measuring the original length of the dorsum as well as of the anterior border of the septum, straight segments with the required dimensions can be sought for reconstruction. Frequently, there is a straight segment located at the bony cartilaginous junction that measures between 30 and 35 mm. This can be used as the new dorsum. Typically, the anterior border measures between 18 and 20 mm, and a separate straight replacement piece can also be found. However, if a straight segment with the required dimensions is unavailable, the remaining bent segments can be straightened by “laminating” reciprocally bent pieces to balance the deflection. In all cases of an extracorporeal septoplasty, spreader grafts are inserted to keep the dorsal septum straight and to simultaneously support the internal nasal valve (Fig. 1.5).
A precise fixation of the replanted septum is essential for the success of the procedure. First, it is essential to suture the reconstructed septum to the upper lateral cartilages (Fig. 1.6) and in most cases to the nasal bones as well (Fig. 1.7). However, in noses with long upper lateral cartilages, it is often sufficient to only fix the replant to the upper lateral cartilage. Conversely, in cases with long nasal bones and short upper lateral cartilages, fixation to the nasal bones is a must (Fig. 1.7). This first requires drilling perforations in the nasal bones to permit placement of mattress sutures.
Recently we developed two additional techniques for securing the reimplanted septum back to the bony vault. With our previously described technique, it was sometimes difficult to find the opposite drill hole when passing the suture through the reimplanted septum. Therefore, we now use what we call the “crisscross” technique. With this method, we drill a hole through the distal nasal bone on the right side and then pass the suture obliquely through the reimplanted septum until it emerges from the contralateral ULC. We then drill a hole through the distal left nasal bone and repeat the process. In this manner, the reimplanted septum is securely fastened at the keystone area with a crisscrossing mattress suture where we begin the suture fixation (Fig. 1.8).
If the nasal bones are too short to permit access for drill hole placement, my collegue Sebastian Haack suggested to create osseous drill holes using a percutaneous technique called the “transcutaneous-transosseous-cerclage technique” (TTC-technique). The drill holes are created by mounting the hub of an 18-gauge needle over a cylindrical drill bit and then penetrating the skin with the needle before drilling through both nasal bones and the reimplanted septum with a single pass (Fig. 1.9). The needle is then left in position but disconnected from the drill, and a 4-0 PDS suture is fed retrograde through the needle tip until it emerges from the needle hub. The needle is then removed leaving the suture in place, and a small hook is passed subcutaneously to retrieve the suture tails from beneath the skin flap. The suture is then tied over the bony dorsum to immobilize the reimplanted septum leaving the suture buried subcutaneously.
After secure fixation of the septum to the nasal dorsum, the caudal septum is stabilized in a longitudinal groove, which is drilled to the anterior spine. Before fixation, precise adaptation of anterior septal length is established by trimming excess cartilage from the base of the caudal septum. Only then is the septum fixed to the anterior spine through a transverse drill hole placed through the nasal spine, resulting in safe and reliable immobilization (Fig. 1.1).
Before fixation of the replanted septum to the anterior nasal spine is performed, it must be confirmed that the spine rests in the anatomic midline. If this is not the case, treatment depends on whether the spine is wide and broad enough to permit partial resection on one side so that the remnant is positioned in the midline (Fig. 1.10). If so, the caudal septum can be successfully secured to the spinal remnant. In cases where the anterior spine is dislocated by more than 2–3 mm, we amputate the spine with a Lindemann burr, reposition the bony fragment onto adjacent bony structures, and secure the fragment with microscrews and microplates (Fig. 1.11). However, in such cases it is often difficult to fixate the caudal septum to the repositioned nasal spine, making it necessary to fix the septum directly to the microplate (Fig. 1.12).
In severely deformed noses, there can be problems with minor dorsal irregularities because concurrent osteotomies are often needed to straighten the bony nasal pyramid. Camouflage can be accomplished with different onlay grafts such as reinsertion of a modified dorsal hump (Fig. 1.13), morselized cartilage (Fig. 1.14), free transplanted diced cartilage (FDC) (Fig. 1.15), or a fascia graft, either autogenous or allogenic (Fig. 1.16). The graft should cover the whole dorsum to create a smooth and uniform surface.
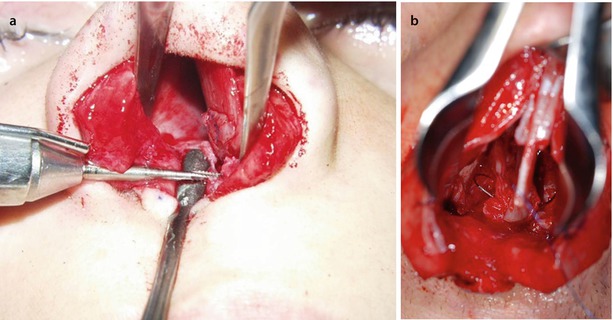

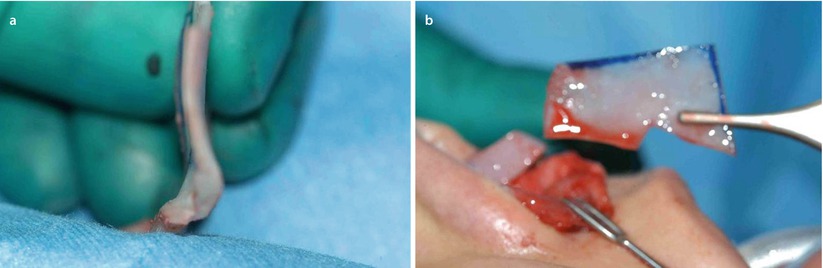
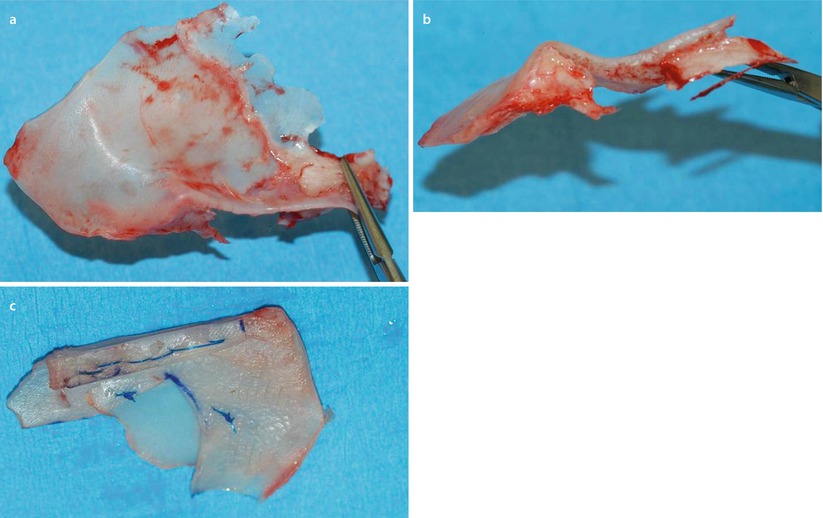
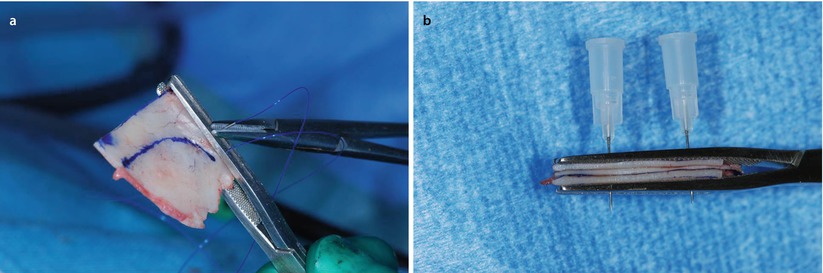
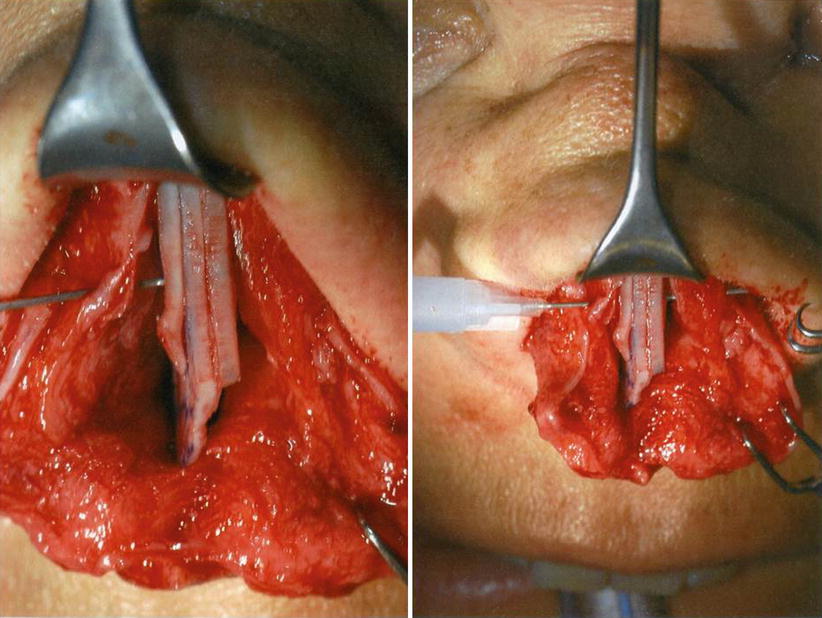
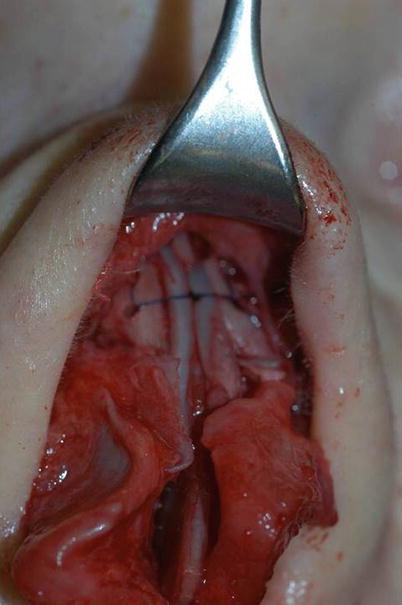
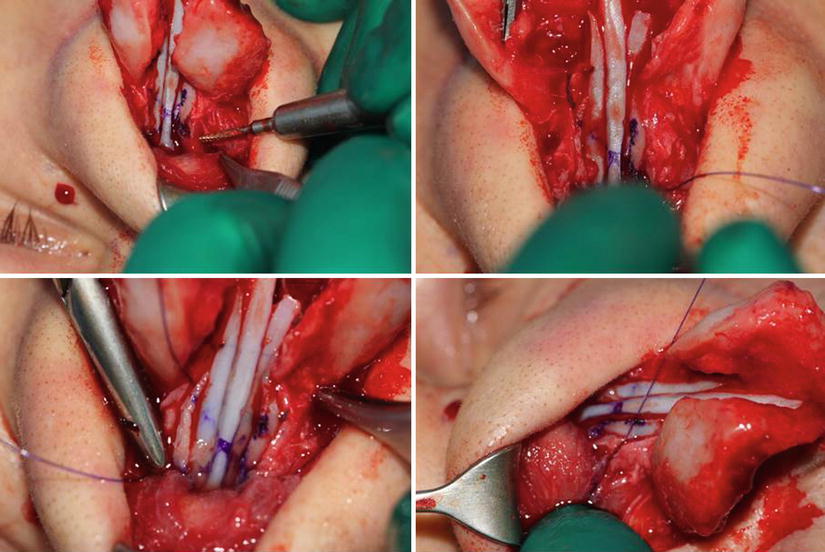
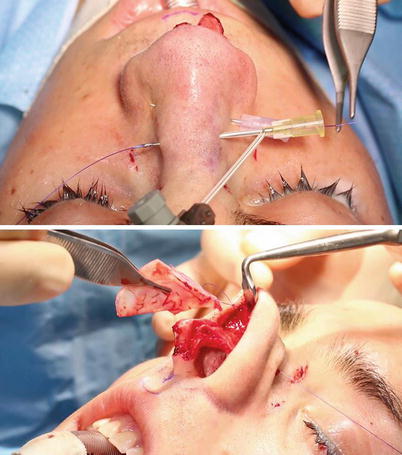


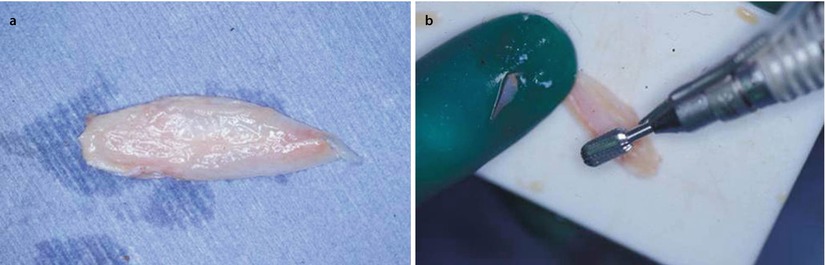

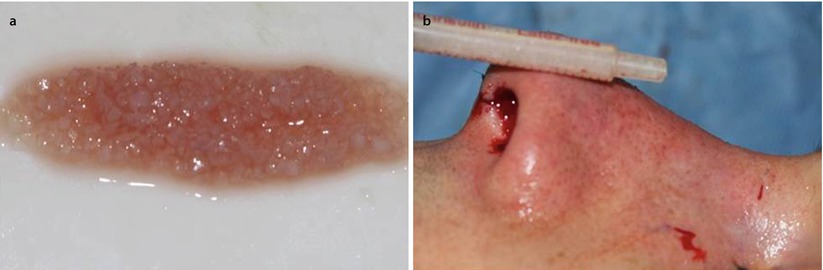
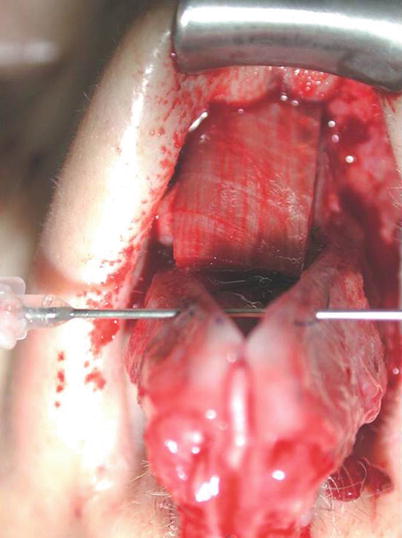
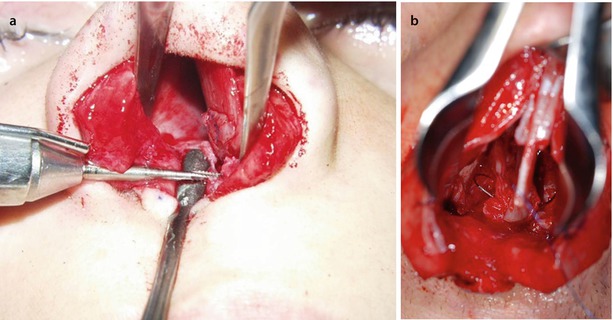
Fig. 1.1
(a) Drilling a hole through the anterior nasal spine (ANS) with a Lindemann fraise. (b) Fixation of the septum to the anterior nasal spine via a transverse bony drill hole

Fig. 1.2
Splinting of the scored septum using the perpendicular ethmoid plate
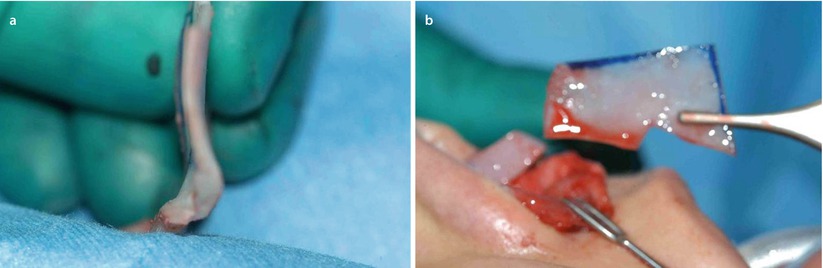
Fig. 1.3
(a, b) Endonasal septal correction with reinsertion of straight segment
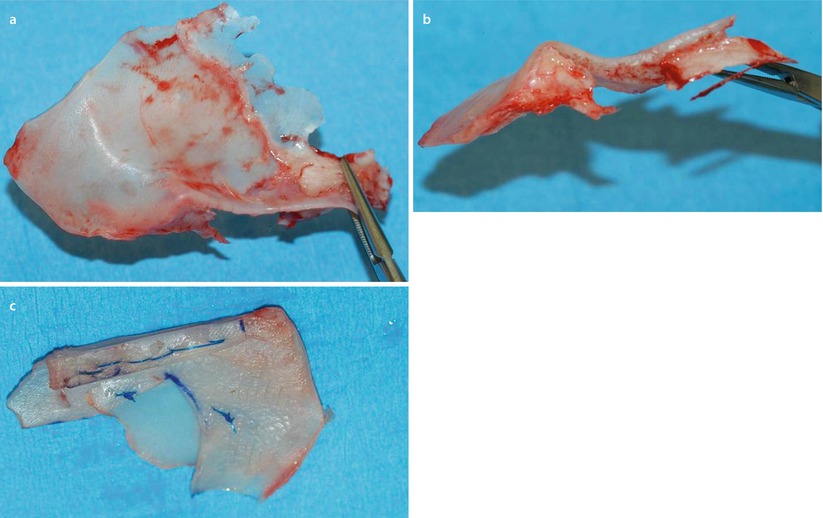
Fig. 1.4
(a–c) Explanted severely deformed septum
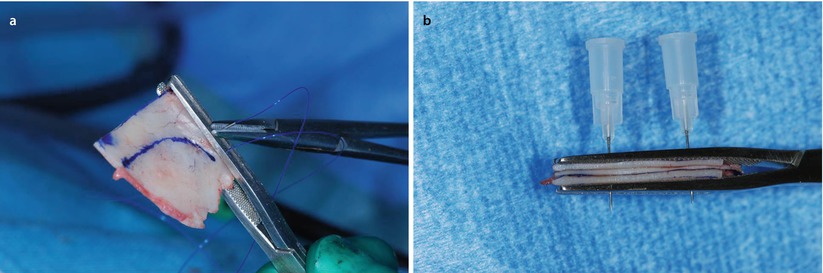
Fig. 1.5
(a, b) Creation of L-shaped neoseptum fixing spreader grafts
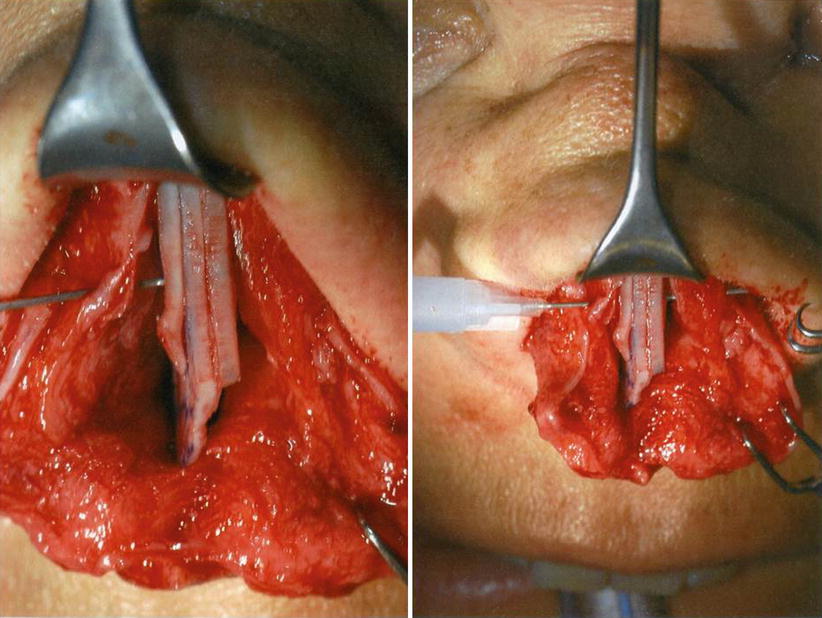
Fig. 1.6
Suture fixation of neoseptum to the upper lateral cartilage
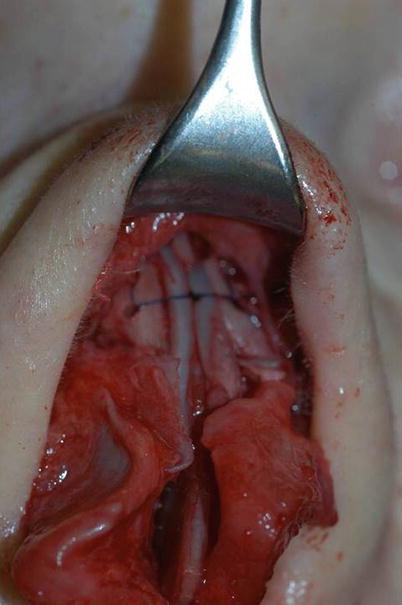
Fig. 1.7
Suture fixation of the neoseptum to the nasal bones using bony drill holes
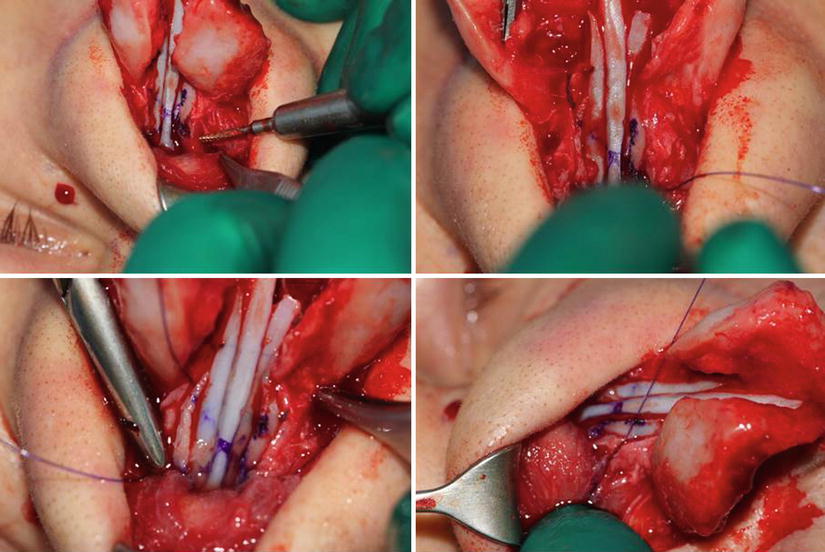
Fig. 1.8
Crisscross technique for reconstruction of the keystone area
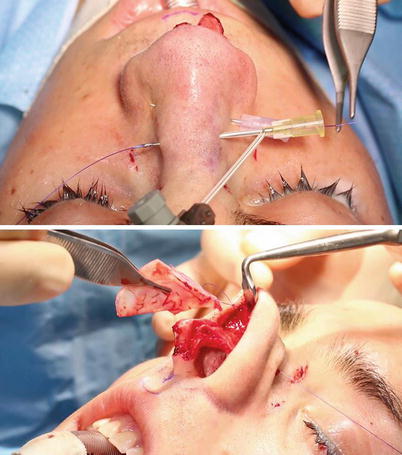
Fig. 1.9
TTC technique to fix the septal replant to the bony pyramid

Fig. 1.10
Partial resection of the anterior nasal spine
Fig. 1.11
Fracturing and fixation by osteosynthesis of the anterior nasal spine

Fig. 1.12
Fixation of the septum to a microplate
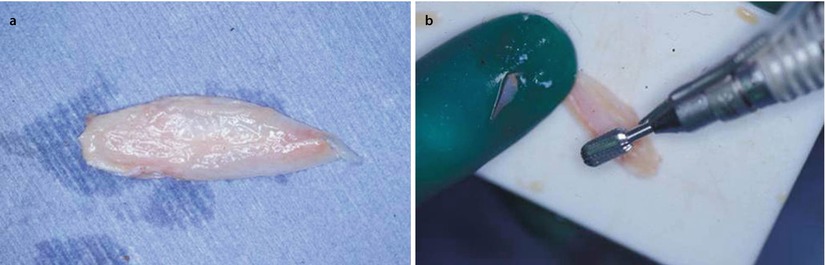
Fig. 1.13
(a) Removed hump after using compound technique. (b) Molding the hump with a cylindrical drill for dorsal grafting

Fig. 1.14
Dorsal graft from morselized cartilage
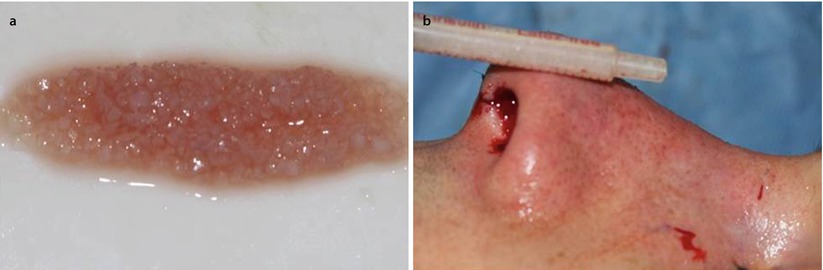
Fig. 1.15
(a, b) Camouflaging dorsal irregularities with free diced cartilage (FDC)
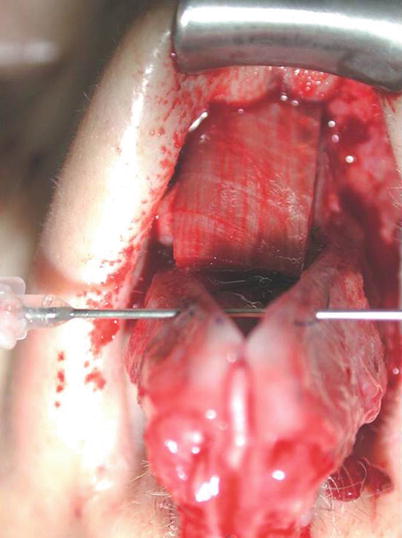
Fig. 1.16
Dorsal graft from allogenic fascia lata (Tutoplast)
1.2 Case Studies: Primary Septoplasty
1.2.1 Case 1: Technique: Fixation of the Caudal Septum to the Nasal Spine
Through the open approach, the nasal spine is bluntly dissected from the soft-tissue attachments using scissors or a round knife. This dissection is carried out between the two medial crural segments of the lower lateral cartilage to expose the spine along the bony floor of the nasal cavity, where it continues as the maxillary crest. The relation to the caudal septum and the shape of the spine can be clearly seen, and its central location can be confirmed. A power-driven Lindemann burr is used to drill two or three transverse holes across the nasal spine for firm fixation of the caudal septum. An anteroposterior oriented midline groove is then burred into the nasal spine to receive the relocated septum. It is necessary to adequately mobilize the septum from the maxillary crest to allow it to return to the midline for fixation. This technique is also used in the replantation of the septum in an extracorporeal septoplasty. A nonabsorbable 4.0 suture such as a Prolene suture is used to achieve firm fixation with multiple passes through cartilage and bone.
A 28-year-old male presented with breathing problems and a nose that was slightly deviated to the right. In profile, a small hump was seen. The columella was oblique rather than vertical, and the caudal septum was displaced into the left nasal vestibule. Endonasal examination also revealed a wide spur on the left side.
Intraoperatively, the septum was found to be too tall and was dislocated off the premaxilla into the left nasal vestibule (Fig. 1.17). The base of the septum was subsequently shortened and mobilized from the maxillary crest to permit midline repositioning, where it was seated into the predrilled groove (Fig. 1.18). Firm suture fixation to bone was then possible through the drill holes in the nasal spine.
Postoperatively, the axis of the nose is seen to be straight with a vertical columella and near symmetrical nostrils. In profile, the dorsum was straight (Figs. 1.19, 1.20, and 1.21).
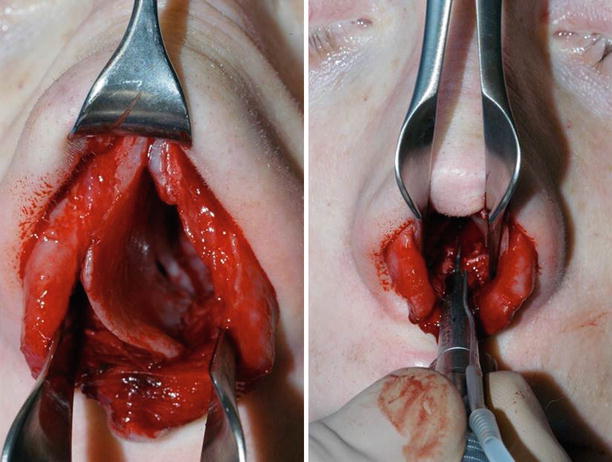
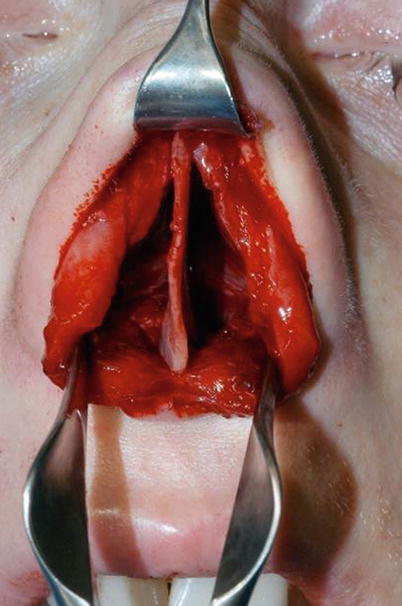
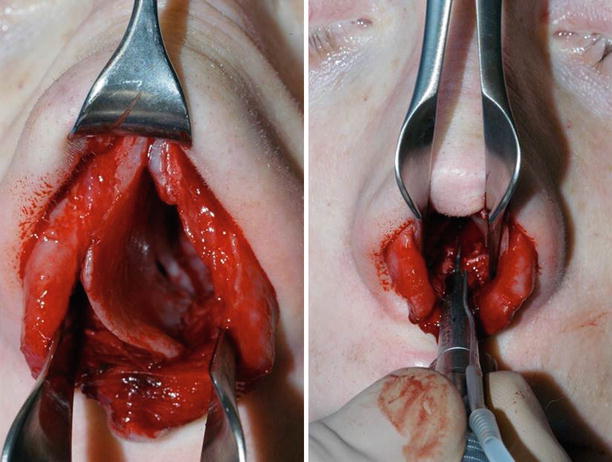
Fig. 1.17
The dislocated septum, drilling a groove into the anterior nasal spine (ANS)
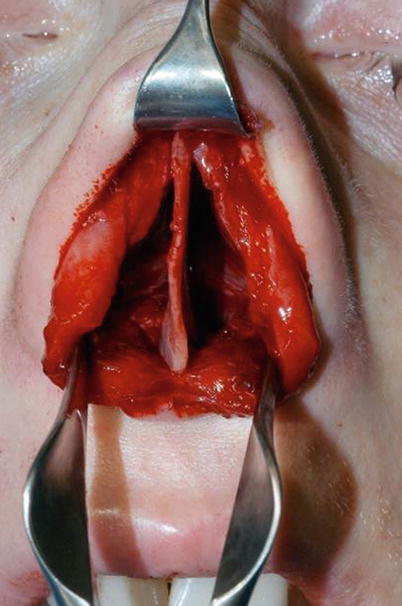
Fig. 1.18
The shortened septum is fixed in the midline