Chapter 11 Primary Rhinoplasty
Summary
Introduction
When reviewing the literature, it is readily apparent that the history of rhinoplasty is rooted in the surgeon’s thorough understanding of the three-dimensional nasal anatomy of the nasal region, proficiency in nasal and facial analysis, and firm grasp of the core concepts in manipulating nasal soft tissues, cartilage, and bone.1 Having satisfied these requirements, the surgeon relies on his or her aesthetic sense to craft a result that will produce a balanced, harmonious nose in relationship to the rest of the face.2 The initial operation is critical to the long-term result in primary rhinoplasty, because the tissues are virginal and undistorted by prior operative procedures.
Indications
Patient Selection
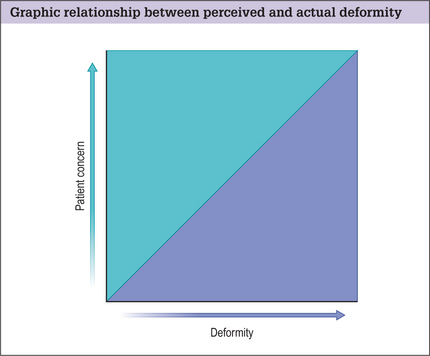
Proper patient selection is vital to a successful outcome. Some patients will likely be dissatisfied regardless of the surgery result. This emotional dissatisfaction often supersedes technical failure as the most common cause of poorly perceived results.
Gunter and Gorney3–5 have both commented on ‘danger signs’ that may be exhibited (Box 11.1). Individuals who meet these criteria should be approached with caution because surgical intervention may not be in the best interests of either the patient or the surgeon.
Similarly, Gorney employs two systems to identify potential problem patients:
Preoperative History and Considerations
Patient Factors
Other red flags in rhinoplasty include:
It should be noted that men tend to have a poorer understanding of their deformity than women and have a more difficult time elucidating the changes they want.6–8
Nasal History
A full and complete nasal history should be obtained. This includes a prior history of:
Anatomic Features
Having determined that the patient is an appropriate candidate for surgery, the next element to proper preoperative surgical planning is critical facial analysis.9,10
Each individual nose has different proportions, morphology, and relative relationships with the surrounding face. To preserve nasofacial harmony, it is crucial to perform a systematic and meticulous analysis of the nose and face. The evaluation is performed in a systematic manner cultivated by the surgeon to assure consistency.11–13
Skin type
The native skin quality influences the operative plan and subsequent techniques performed.
First, skin type, thickness, and texture are assessed.
Systematic analysis of the nose and face
Next, a systematic analysis of the nose and face is undertaken.
Look for potential anomalies of the underlying facial skeleton
We divide the face into thirds using horizontal lines adjacent to the:
The upper one-third is the least important because it is the most variable.
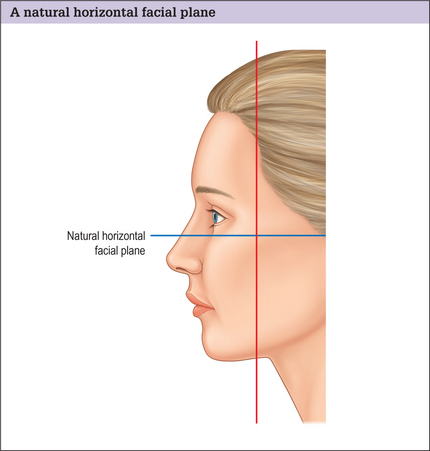
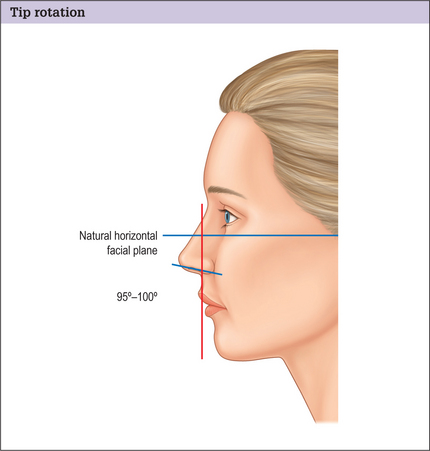
A natural horizontal facial plane is determined by drawing a line perpendicular to a plumb line superimposed over the head in repose and the eyes in straightforward gaze. This will serve as a future point of reference (Fig. 11.2).
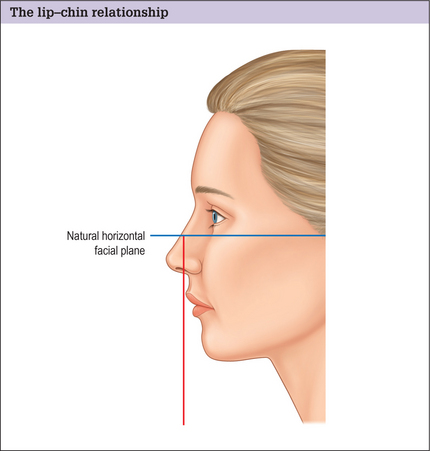
The lip-chin relationship is assessed by dropping a vertical line from a point one-half the ideal nasal length tangential to the vermillion of the upper lip. The lower lip should lie no more than 2 mm behind this line (Fig. 11.3). The ideal chin position is gender dependent. The female chin should be slightly posterior to the lower lip, but equal to the lower lip in men. Discrepancies in these relationships may warrant orthodontics, orthognathic surgery, or a chin implant.
Nasal features
Frontal view
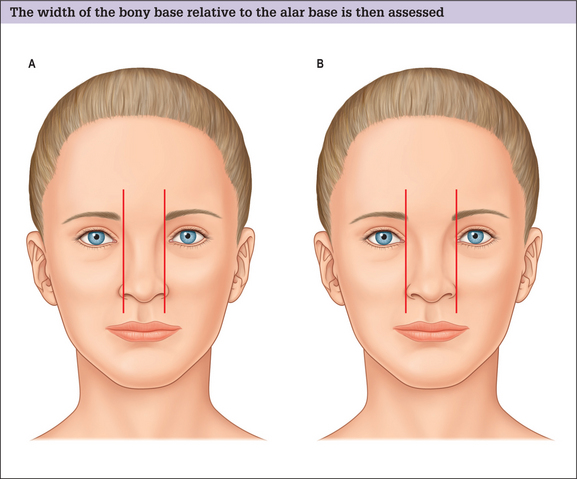
A relationship between the bony base width and the alar base is then assessed. The bony base width should be 80% of the normal alar base width, and a normal alar base width 2 mm wider than the inter-canthal distance, or the width of one eye (Fig. 11.4A&B). If the bony base is greater than 80% of the alar base width (assuming the alar base width is normal), osteotomies will be required to narrow the dorsum. Males tend to have a wider bony base than females and it is important not to over-narrow the male dorsum creating a feminized result.
Next the alar base and alar rim are analyzed. If the alar base width is over 2 mm and greater than the intercanthal distance, it must be determined whether the cause is a narrow intercanthal distance, a true increased interalar width, or alar flaring:
The tip is assessed to determine:
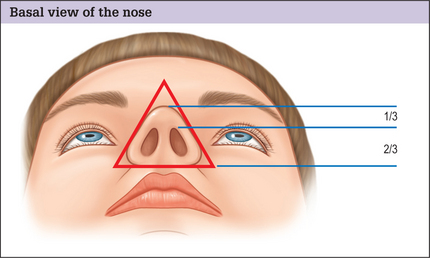
Basal view
The basal view of the nose is addressed next, with the outline of the nasal base describing an equilateral triangle with a lobule-to-nostril ratio of 1 : 2 (Fig. 11.6). The nostril itself should have a teardrop-like geometry, with the long axis from the base to the apex oriented in a slight medial direction.
Lateral view
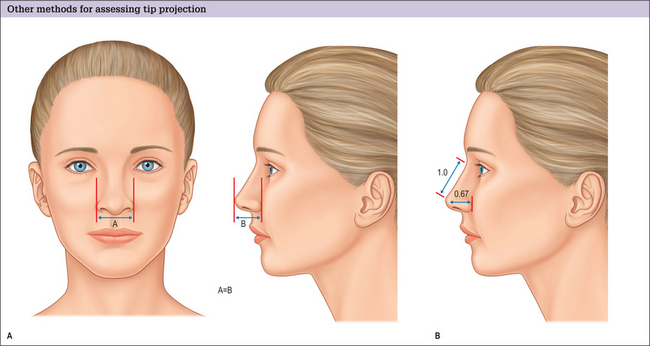
Tip Projection
Tip projection is addressed on the lateral view. We describe two methods to accomplish this.
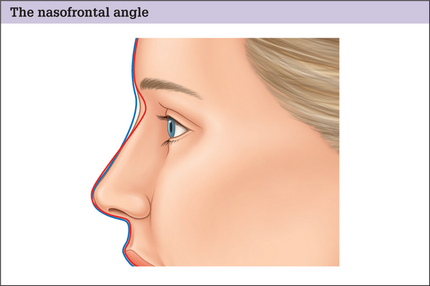
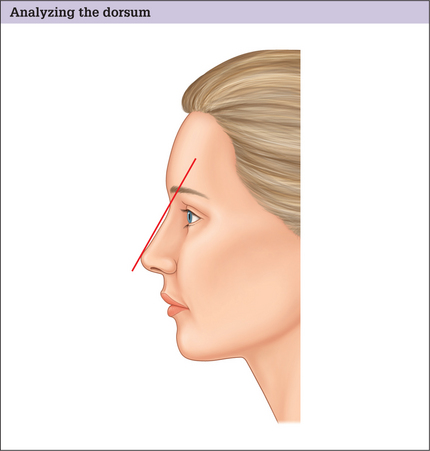
Dorsum
The dorsum is then analyzed. The ideal nasal dorsum should lie approximately 2 mm behind and parallel to a line from the radix to the tip-defining points in women, but should be slightly higher in men to avoid feminizing the nose (Fig. 11.10).
Tip Rotation
The nasolabial angle is used to determine the degree of tip rotation. This angle is obtained by measuring the angle between a line coursing through the most anterior and posterior edges of the nostril and a plumb line dropped perpendicular to the natural horizontal facial plane. This angle should be between 103–105 in women and 95–100 in men (Fig. 11.11).
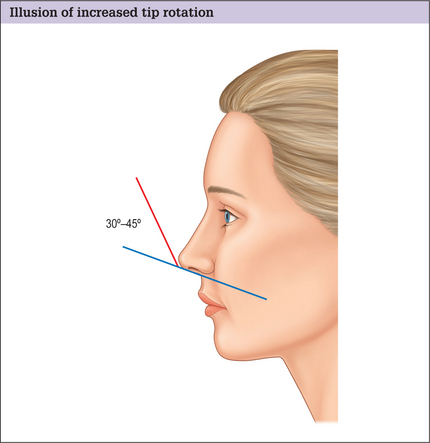
Do not confuse the nasolabial angle with the columellar-labial angle, which is formed at the junction of the columella with the infratip lobule. This angle is normally 30–45 ° (Fig. 11.12). Increased fullness in this area is usually caused by a prominent caudal septum giving the illusion of increased rotation, even though the nasolabial angle is normal.
Alar-columellar relationship (lateral and frontal views)
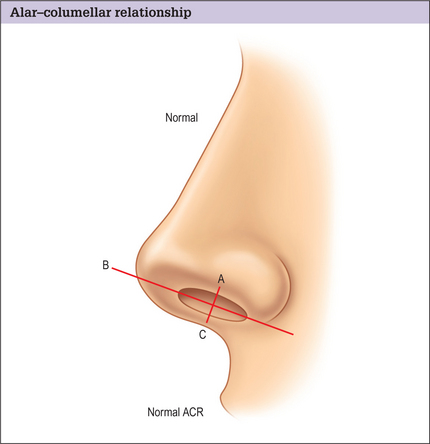
The alar-columellar relationship is then assessed.
A line is drawn through the long axis of the nostril, and a perpendicular line drawn from alar rim to columellar rim that bisects this axis. The distance from the alar rim (point A) to the long axis line (point B) should equal the distance between the long axis line to the columellar rim (point C) if the alar-columellar relationship is normal (Fig. 11.13).
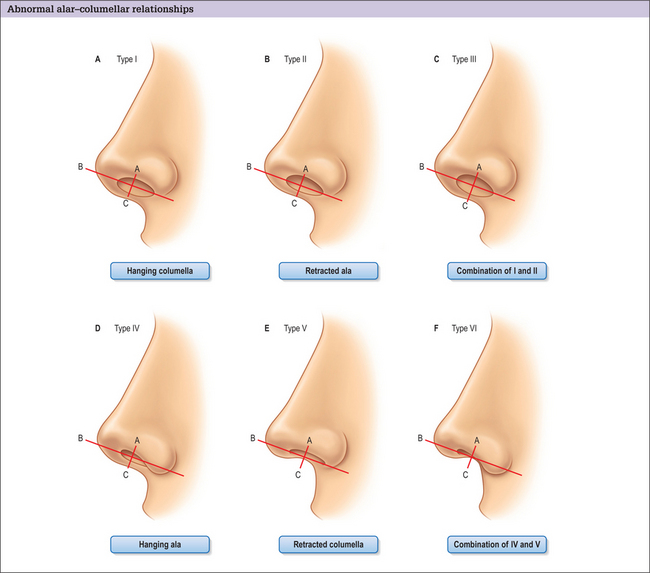
If these measurements are not normal, nasal dismorphology can be categorized into six classes:16,17
Differences between male and female noses
The proportions given above generally apply to Caucasian women. Generally, the male face tends to have a squarer, less rounded appearance, with stronger more pronounced features. The key differences in males are summarized in Box 11.2.7
Box 11.2 Key features of male noses (compared with female noses)*
* These proportions are general guidelines and vary between gender and racial origin. They are only meant to be used as a systematic method of analysis with general proportions and relationships. Each nose should be individualized to the patient’s facial structure and tempered by their desires to create nasofacial harmony and balance.
Intranasal exam
An intranasal exam completes the preoperative analysis. This is performed with a nasal speculum, headlight, and vasoconstriction. The septum, turbinates, and internal nasal valve are evaluated for obvious deformities or pathology. If turbinate hypertrophy is identified, the underlying etiology should be investigated. Turbinate enlargement may be:
Patient Counseling
After the initial history and physical examination, the procedure is fully discussed with the patient. The risks and benefits of the procedure are detailed, and all questions answered. The patient is provided with a written, detailed estimate of surgical charges with complete explanations. It is recommended that patients sign a form accepting financial responsibility. A second clinic visit is encouraged to review the previous discussions. The deformities are reiterated, questions answered, and the consent reviewed and signed. A preoperative instruction sheet and a list of medications to be avoided are also provided (Box 11.3).
Box 11.3 Preoperative instruction sheet
Two weeks before surgery
Morning of surgery
Prior to surgery we convert our operative plan into a graphic re presentation (using Gunter Graphics5) to assist us in the operating room. Modifications to the plan are documented intraoperatively, transposed to the graphic depictions postoperatively, and placed in the patient’s chart for future reference.
Operative Approach
Relevant Anatomy
Skin
The thickness, mobility, and sebaceous character of the nasal skin vary along its length, with the upper two-thirds being thinner, more mobile, and less sebaceous than the inferior one-third.18
Muscles
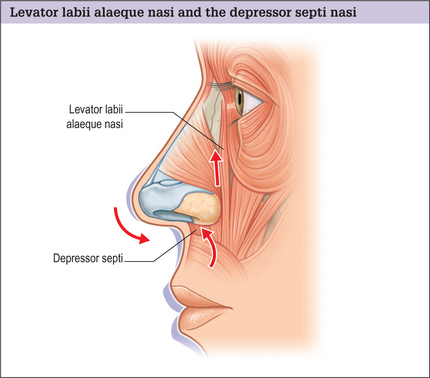
Two muscles, in particular, are important in rhinoplasty:
Evaluation of the depressor septi nasi is routine in our preoperative assessment. Its effect on depressing the nasal tip and shortening the upper lip can be appreciated in some patients on animation (especially when smiling). In the subgroup of patients in whom this muscle significantly alters the nasal appearance, we dissect and transpose the muscle. By doing so, several goals are achieved:
Blood supply
The vascular supply to the nose is derived from branches of the ophthalmic and facial arteries (Fig. 11.16).
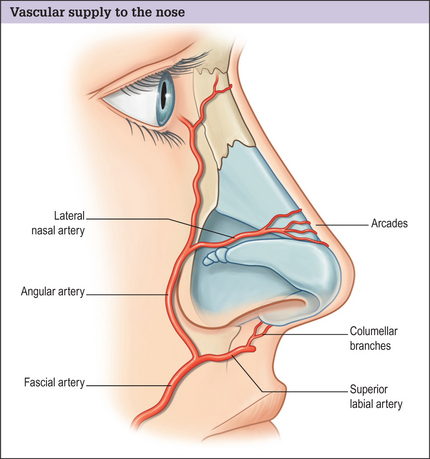
Fig. 11.16 Vascular supply to the nose. This is derived from branches of the ophthalmic and facial arteries.
In our 1995 study,21 we found the lateral nasal arteries to be present (either singularly or bilaterally) in 100% of cases, with the columellar branches present 68.2% of the time.
Toriumi et al.22 studied the vascular and lymphatic anatomy of the nose and determined that the transcolumellar incision itself did not compromise major venous or lymphatic outflow. Furthermore, they recommend dissection just above the perichondrium in the deep areolar plane, leaving the musculoaponeurotic layer intact, which preserves the major arterial vascular supply and avoids damage to the venous and lymphatic vasculature that lies in a more superficial (subcutaneous) plane. In this way, bleeding and postoperative edema are minimized.
Nasal vaults
Bony vault
The bony vault (Fig. 11.17) constitutes the upper one-third to one-half of the nose and is made up of the paired nasal bones and the ascending frontal process of the maxilla. It is important to note that the nasal bones are narrowest and thickest above the canthal level. As a result, osteotomies are rarely indicated above this level.