Chapter 8 Periorbital Rejuvenation
Summary
Introduction
Ernst Fuchs coined the term blepharochalasia in 1896.1 The term is used now for idiopathic recurrent swelling, although Fox first used the term dermatochalasis over 50 years later. In the 19th century, the correction of ptosis was performed by resecting skin. William Bowman first described both anterior and posterior approaches.2 The first cosmetic surgery article was written by Charles Conrad Miller on the excision of ‘bag like folds of skin of the eyelid’.3 He went on to describe a subciliary incision as well as a supratarsal fold incision. The first cosmetic surgery text was published in 1907 by the same author.4 This new area of modern medicine was not as well accepted as the second book of cosmetic surgery by Frederick Strange Kolle.5 Kolle described the importance of marking the amount of skin to be excised preoperatively. A transconjunctival approach was first described by Julien Bourget along with the first pre- and postoperative photographs.6 The transconjunctival approach lost favor but regained popularity when Tessier used the same approach for access to the orbital floor.7 The retroseptal approach was introduced by Baylis and Sutcliffe in 1983.
The distinct fat compartments of the upper lid were first described by Bourget, but Salvadore Castanares described their relation to each other as well as the lower-lid fat pads.8 The importance of lacrimal gland prolapse was noted by Smith and Petrelli.9 Naugle realized the importance of lower-lid tightening in blepharoplasty.10 Multiple authors, including Rees, Flowers, Furnas, Aston, Skoog, and Sheen, have further advanced the art of blepharoplasty surgery. Hamra noted that correction of the periocular area extends to the lower face and includes redraping of the orbital fat with elevation of the SOOF and midface.11
Patient Evaluation
It is important to understand the patient’s concerns and to develop a complete plan of correction. The periocular area is complex anatomically and may have been affected by concomitant changes in several areas such as eyebrow ptosis, eyelid ptosis and/or midfacial descent. Dermatochalasis refers to the redundancy of eyelid skin. This is often associated with orbital fat protrusion or prolapse. Fat protrusion is more common in older individuals, but may be present in younger people with a familial predisposition. Significant dermatochalasis of the upper eyelids can lead to a heavy feeling around the eyes, brow ache, complaints of eyelashes being present in the visual axis, and reduction in the superior visual field.
It is important that complaints regarding lower eyelid bags and wrinkles are addressed. Candidates for lower blepharoplasty, especially those who smoke, occasionally exhibit bags over the malar area. The area of concern to the patient may prove to be the malar bags (Fig. 8.1) rather than the lower-lid fat pads themselves. When patients refer to their eyelid wrinkles, it is important to determine whether they are referring to the eyelid wrinkles that are present without animation (static wrinkles) or the wrinkles that become discernible when the patient is squinting or smiling. The surgeon must explain that the dynamic lines may not completely disappear after blepharoplasty. Static fine wrinkles may be addressed with laser or chemical resurfacing.
A history of dry eyes12 is an important factor in proceeding with blepharoplasty surgery. Other history and findings include Graves’ disease, diabetes, bleeding tendencies, hypothyroidism, renal dysfunctions, cardiovascular disorders, and hepatic dysfunctions. Lagophthalmos may be worsened after surgery and could result in corneal breakdown and infection if not detected during the clinical evaluation. Lagophthalmos may be caused by a seventh nerve palsy or lid retraction from trauma, surgery or midfacial descent. Other corneal diseases such as neurotrophic keratopathy are contraindications for eyelid surgery. This condition results in poor corneal wound healing and is caused by many diseases such as cerebrovascular accidents, multiple sclerosis, diabetes mellitus, herpes simplex and herpes zoster infections. Previous eyelid surgery, eyelid trauma, eye or eyelid inflammation and allergies are also pertinent to the impending surgery.
Blepharochalasis or dermatochalasis may be present, and it is crucial that the two are differentiated from one another. The former is a rare bilateral condition most commonly seen in younger women. These patients have thin, atrophic, ‘crepe-paper-like’ wrinkled skin loosely bound to the orbicularis muscle. Blepharochalasis is more prevalent on the upper eyelids, resulting in protrusion of the orbital fat because of a weakened septum. This condition can be familial, although some believe episodes of recurrent angioneurotic edema may contribute to its development. Prominent eyelid vascularity may be associated with this condition.13 Dermatochalasis is a common bilateral condition affecting both genders equally. It is generally seen in middle or older age groups, presenting as a horizontal redundancy of the skin along with herniation of intraorbital fat caused by aging. Other conditions include blepharopachynsis (thickening of the eyelid) and blepharomelasma.14
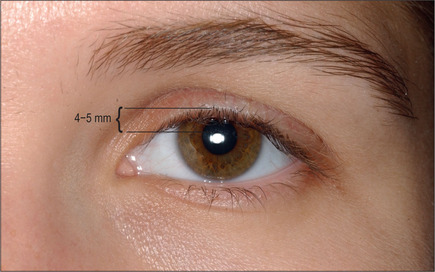
In straight gaze, the upper eyelid margin overlaps the limbus 1-2 mm.15 This overlap is increased on a patient with blepharoptosis. Since the full cephalocaudal diameter of the limbus is approximately 11 mm and a 1-2 mm overlap of the limbus is considered normal, any decrease in the visible portion of the limbus is a reflection of eyelid ptosis expressed in millimeters. For example, if only 7 mm of the iris is visible, the patient has 1-2 mm ptosis. A more accurate value is the margin reflex distance (MRD). This measurement is from the central corneal light reflex to the upper eyelid margin. The normal measurement is 4-5 mm (Fig. 8.2).
The examiner can obtain an accurate measurement of levator function (excursion) by holding a ruler next to the patient’s eyes. With the head immobilized, the patient is instructed to look downward, and the point corresponding to the eyelid is noted on the ruler. The patient is then instructed to look upward, and the corresponding point is again checked on the ruler. The distance between these two points reflects the levator function expressed in millimeters. It is often necessary to repeat this test several times to obtain a reliable number. Normal eyelid excursion is 15 mm or more. Excursion of 4 mm or less is considered poor levator function, 5-7 is fair, 8-10 is good and 10-15 is excellent. In general, patients with aponeurotic ptosis have good-to-excellent levator function and those with congenital ptosis have poor levator function. The position of the eyelid crease serves as a guide for the degree of ptosis and potential for levator dehiscence. A higher than normal upper eyelid crease (8-10 mm) may be a sign of levator dehiscence and aponeurotic ptosis. Common causes of neurogenic ptosis include myasthenia gravis, Horner’s syndrome and third nerve palsies. An example of a myogenic-type ptosis is myotonic dystrophy. Pseudoptosis may be caused by aberrant regeneration of the facial nerve with overactive orbicularis tone or may be present with contralateral lid retraction.
Excess fullness in the lateral portion of the upper eyelid, particularly in older patients, could denote prolapse of the lacrimal gland or an extension of the lateral (temporal) eyelid fat pad. Occasionally a significant degree of fullness is found in the lateral portion of the upper eyelid as a consequence of a prominent lateral supraorbital rim or excess retroorbicularis oculi fat (ROOF).16 The lower eyelid usually touches the lowest portion of the limbus. Generally, any scleral show is considered undesirable and may serve as a risk factor when removal of excess skin from the lower eyelids is planned. In this case the surgeon must either strengthen the lower-lid support mechanism or be extremely conservative with the skin removal. The fat pads in the medial, central, and lateral compartments of the lower eyelids are examined while the patient gazes straight ahead and upward. A depression above the infraorbital rim (malar groove) or nasojugal area should be assessed; correction of this condition will enhance the blepharoplasty results. Aesthetic surgery patients commonly exhibit hyperpigmentation of the lower eyelids and less commonly of the upper eyelids.
Slow, incomplete blinking may denote a weakness of the orbicularis muscle. Normal spontaneous blinking frequency is 10-15 blinks every minute, with the lower eyelid movement starting two-tenths of a second earlier than the upper eyelid.15
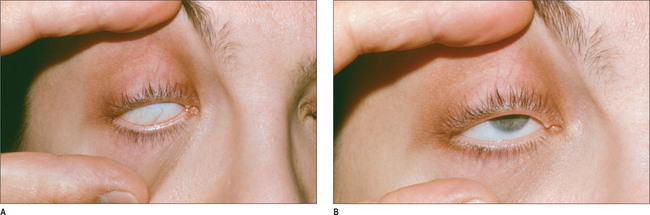
A negative Bell’s phenomenon is an indicator of potential for exposure keratitis postoperatively. The patient is asked to close his or her eyes while the examiner forcefully holds the eyelid open (Fig. 8.3). Normally, the globe will rotate cephalad. The surgeon has to be conservative when planning blepharoplasty if Bell’s phenomenon is poor or nonexistent.
The most projected portion of the malar soft tissue on the profile view should line up with the most projected point of the eye globe or project more anterior to it. Deficiency of the malar soft-tissue prominence (negative vector) creates a negative value and is a significant risk factor for dry eye syndrome or postoperative lid lag.12
A gross visual examination with a vision chart may disclose an abnormality of which even the patient is unaware. This abnormality could range from minimal to significant visual loss. A visual field examination may indicate a deficit in the visual field by a true ptosis of the eyelids or pseudoptosis related to dermatochalasia. The basic secretion test (basic Schirmer’s test) can be used to measure the amount of basal tear secretion without the overlying and less predictive reflex tearing arc. Topical ophthalmic anesthetic is placed in both eyes. The fornices are gently swept with a cotton-tip applicator. A 5 × 35 mm strip of Whatman No. 41 filter paper is folded 5 mm and placed on the lateral third of the lower-lid conjunctiva. While the patient closes the eyes, the strips of the paper are left in place for 5 minutes. Generally, wetting of the strips less than 10 mm from the fold is considered positive for some degree of dryness. This test can be variable in different patients and in the same individual at different times; therefore, it cannot always be fully relied upon. A tear break-apart time is a more reliable test for documentation of the dryness of the eyes. If there are questions concerning the amount of tear production or the eye condition, it is always prudent to secure an ophthalmologic consultation.
Further testing for a patient with eyelid ptosis includes the phenylephrine test. This test is contraindicated with a history of narrow angle glaucoma, labile hypertension or a shallow anterior chamber on examination. Phenylephrine may exacerbate increased intraocular pressure in a susceptible patient. This test is performed for consideration of a Müller muscle – conjunctival resection (Putterman procedure). First, the margin reflex distance is measured bilaterally. Topical phenylephrine 2.5% or 10% solution is then placed in the superior cul-de-sac while the patient is in a reclined position.17 Several minutes are allowed to pass and the margin reflex distance is re-measured with the patient in a sitting position. The eyelid height attained with the installation of topical phenylephrine can be achieved with an 8 mm Müller muscle conjunctival resection. Levator advancement surgery can be considered in patients with a negative phenylephrine test and normal levator function.
Operative Approach
Anatomy
The supratarsal crease is located 8–10 mm above the upper lid margin. This crease is formed by adhesion of the orbicularis muscle and fi brous attachments of the levator aponeurosis to the skin. A supratarsal fold that is too high or appears to be nonexistent suggests attenuated, split, or even absent levator attachment to the skin. A male skin crease is usually 6–8 mm and a female skin crease is 8–10 mm above the lid margin.18 A vast variation in the amount of skin present exists between individuals of various races, ages and ethnic descents. Those from the Far East have an absent supratarsal fold even with normal levator function. This results from either a lack of aponeurotic attachments to the skin or attachment at a site much lower than normal.
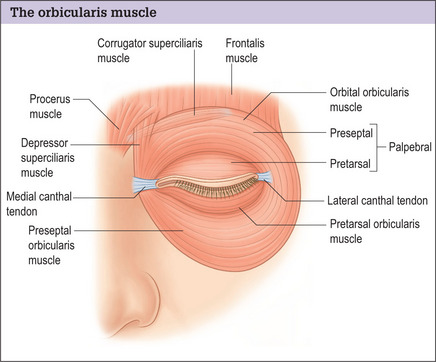
The orbicularis muscle has two segments concentrically distributed around the eye, the orbital, and palpebral portions (Fig. 8.4). The orbital segment of the muscle overlies the orbital rims. This muscle originates from the superomedial border of the orbital wall and the maxillary process of the frontal bone. The most cephalic portions of the fibers spread upward onto the forehead to interface with the frontalis and corrugator supercilii muscles superiorly and continue laterally to overlie the anterior surface of the temporalis fascia. There are additional fibrous attachments to the medial canthal tendon and the frontal process of the maxilla, as well as the inferior orbital rim. In the lower lids the orbital portion of the orbicularis facilitates the forceful closure of the eyelid during squinting and acts in concert with other mimetic muscles during animation.
The palpebral portion of the orbicularis oculi muscle is further divided into preseptal and pretarsal segments. The preseptal segment extends from the medial canthal tendon to the lateral raphe overlying the lateral canthal tendon. It has superficial origins from the anterior limb of the medial canthal tendon. The deep heads of the muscle, originating from the lacrimal fascia overlying the lacrimal sac, contribute to the lacrimal pump mechanism.19
The pretarsal segment of the orbicularis oculi muscle arises from the superficial heads at the anterior limb of the medial canthal tendon and from deep heads originating along the posterior lacrimal crest and the lacrimal fascia (Horner’s tensor tarsi muscle). The pretarsal muscle segments from both the upper and lower eyelids fuse laterally, forming the lateral canthal tendon that inserts onto the periorbital at Whitnall’s orbital tubercle.
The medial canthal tendon is composed of two heads. The more prominent superficial head attaches to the anterior lacrimal crest, whereas Horner’s muscle, the smaller, deeper head, attaches to the posterior lacrimal crest. The canaliculi are positioned just beneath the superficial head of the medial canthal tendon.15 A portion of the orbicularis muscle, known as the muscle of Riolan, which is the smallest striated muscle in the body, is situated at the lid border. The nerve supply to the orbicularis is via the seventh cranial nerve. These nerve fibers course within the posterior fascia of the muscle and enter through its deep side.20
The orbital septum is a thin sheet of fibrous tissue that lies deep to the preseptal portion of the orbicularis muscle. It serves as a protective barrier and impedes the spread of hemorrhage, infection or inflammation to the orbit. The orbital septum also restricts protrusion of the orbital fat. It extends from the arcus marginalis of the orbital rims, a confluence of the facial bone periosteum and the periorbita, to the tarsal borders. In the occidental upper eyelid, the orbital septum fuses with the levator aponeurosis approximately 2-3 mm above the upper border of tarsus.15 Once fused, the fibers pass downward to insert on the lower anterior surface of the tarsus. In the lower eyelid the orbital septum attaches directly to the inferior border of the tarsus with the capsulopalpebral fascia.21
A layer of fat between the orbicularis muscle and periosteum spans over the lateral half of the orbital rim and sometimes results in protrusion, necessitating its removal. This is termed the retro orbicularis oculi fat pad. There is a similar structure in the lower eyelid termed the suborbicularis oculi fat pad.22,23 The preaponeurotic orbital fat is another distinct layer situated between the levator muscle and the orbital septum of the upper eyelid. Two pockets of fat can be found in the upper eyelid and three in the lower eyelid.
The levator palpebrae muscle is the principal retractor of the upper eyelid. It originates from the periorbita overlapping the lesser wing of the sphenoid bone just above Zinn’s artery and traverses the orbital roof, extending anteriorly over the superior rectus muscle. The levator aponeurosis divides into two attachments approximately 10-12 mm proximal to the tarsal plate.24,25 The anterior aponeurotic fibers attach to the orbital septum at a variable distance above the tarsal border. The posterior fibers of the levator aponeurosis extend caudally to insert into the anterior surface of the tarsus 3-4 mm below its superior border. The levator aponeurosis possesses medial and lateral extensions designated as the horns. The lateral horn of the levator aponeurosis courses through the lacrimal gland, dividing it into orbital and palpebral lobes to attach to the superior edge of the lateral canthal tendon at the lateral retinaculum. The medial horn, which is not as thick as the lateral horn, passes over the sheath of the superior oblique tendon, fusing with the upper border of the posterior limbs of the medial canthal tendon and fibers of the orbital septum.
The superior sheath of the levator muscle condenses at the level of the equator of the globe to form the superior transverse ligament of Whitnall, a check ligament. It attaches medially to the trochlea of the superior oblique muscle, extending laterally to insert onto the capsule of the orbital lobe of the lacrimal gland. Whitnall’s ligament functions as a pulley to facilitate the change in the direction of the levator action from horizontal to vertical.26
The overall length of the levator muscle and its aponeurosis is approximately 55 mm. The muscular portion constitutes about 40 mm of the total length, and the tendinous portion measures 15 mm.15 The levator complex derives its innervation from the superior ramus of the oculomotor nerve (cranial nerve III).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree