Preoperative Evaluation of Patients Undergoing Cosmetic Blepharoplasty
Joseph A. Mauriello Jr.
The most important features of the preoperative evaluation are considered in detail in this chapter:
General medical and ocular history
Motivation for surgery
Examination
Evaluation of the tear film
Inflammatory signs
Consideration of thyroid ophthalmology and ocular rosacea
Symmetry of the upper lid position
Consideration of the diagnosis of myasthenia gravis
Lower eyelid laxity
Consideration of brow lift
Negative vector orbit
Objective photographic documentation of findings
Show photographs of patients who have undergone surgery
Establish reasonable expectations of what can be accomplished surgically
General medical evaluation
Preoperative instructions
Discussion of informed consent
Communication of payment information
General Medical and Ocular History
It is crucial to determine whether the changes in the periorbital area occurred gradually or whether an underlying medical condition such as thyroid eye disease or other inflammatory disease was responsible for more abrupt changes in the eyelid tissues. Development of eyelid edema over a few months may suggest thyroid eye
disease or other inflammatory process, and a workup is necessary prior to any cosmetic eyelid surgery. A review of the history of the present illness and of old photographs may be helpful and important in determining the time frame of the eyelid changes. A complete medical history, including review of systems and past, family, and social history, is necessary. These historical data are combined with the examination to establish a suspected diagnosis (1).
disease or other inflammatory process, and a workup is necessary prior to any cosmetic eyelid surgery. A review of the history of the present illness and of old photographs may be helpful and important in determining the time frame of the eyelid changes. A complete medical history, including review of systems and past, family, and social history, is necessary. These historical data are combined with the examination to establish a suspected diagnosis (1).
Any history of bleeding is extremely helpful. Bleeding after umbilical cord separation, circumcision, or at the time of first menstruation suggests a congenital bleeding problem. Abnormal bleeding after dental extraction or tonsillectomy also may indicate bleeding problems. Platelet defects or von Willebrand disease (prevalence of 1 % in the general population) may be associated with epistaxis or gastrointestinal bleeding (2). In such cases, a hematologic consultation may be indicated.
Aspirin containing products include (partial listing) Ecotrin, Bufferin, Anacin, Alka-Seltzer, Coricidin, Darvon, Fiorinal, Dristan, Excedrin, Midol, Sine-Aid, Sine-Off, Percodan, and Medipren (2, 3 and 4). These aspirin-containing products, as well as nonsteroidal antiinflammatory agents (e.g., Advil, Motrin), should be stopped for a minimum of 5 days (to avoid blood thinning). Herbs such as gingko, garlic, ginseng, and fish oils may precipitate bleeding and should be stopped 3 weeks prior to surgery. Discontinuation of clopidogrel (Plavix), aspirin, and other platelet inhibitors and anticoagulants, including warfarin (Coumadin) should be discussed with the prescribing physician. Because aspirin inhibits platelet function permanently, its effects last the lifespan of platelets, approximately 9 days. The herb, Arnica montana, appears to reduce postoperative ecchymosis and swelling.
Symptoms of underlying dry eye should be determined: frequency of itching, burning, and foreign body sensation in each eye, as well as any associated tearing or mucous discharge. Many drugs, including antihypertensive medications, estrogen replacement therapy, and antianxiety, antidepressant, and antipsychotic pharmacologic agents, may induce dry eye. Although dry eye is not a contraindication to blepharoplasty, knowledge of preexisting dry eye is important in order to warn patients of possible exacerbation of dry eye after cosmetic eyelid surgery (5, 6 and 7).
Motivation for Surgery
It is important to appreciate what the patient sees as the problem, as well as what he/she would like done. While examining the area of concern, the physician determines the anatomic features of the eyelid and periocular region that potentially could be corrected. In this way, the surgeon is able to analyze the surgical problem and whether it can be reasonably improved. In this manner, the surgeon is able to determine whether the patient’s needs can be met by the surgical plan. Sometimes, a patient wishes to undergo only upper or lower lid blepharoplasty. The surgeon should elicit such information. Although it is generally more cost effective to perform four-lid blepharoplasty, some patients may be unhappy should they undergo four-lid surgery and may experience an unusual and unhappy postoperative course. The surgeon must educate each patient so that the entire process of surgery is understood and the goal of informed consent is achieved. It is the obligation of the physician to provide informed consent and not to delegate this responsibility to a member of the staff.
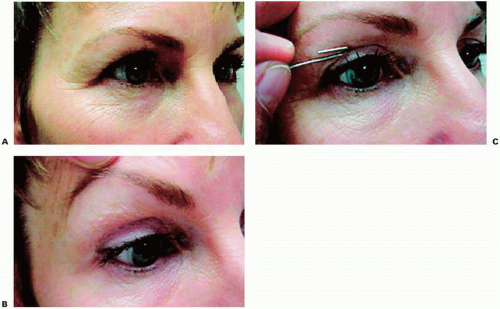
The surgeon, with mirror in hand, is able to point out any asymmetries of the eyelids. Any brow lift surgery should be discussed as well. A digital camera can be used to photograph the patient on the day of the initial examination in order to demonstrate on the photographs the specific anatomic areas of concern and possible surgical solutions (Fig. 1.1).
Khan (8) indicates that the face acts as a vehicle of communication and expression rather than simply as a vehicle of beauty. The surgeon may demonstrate to the patient “universal miscues” that emanate from the face. A tired appearance may relate to the drooping upper lid skin. Botulinum A (Botox) injections may relieve a stern appearance due to frowning from glabellar lines. The cosmetic surgeon should help the patient determine features of the face that serve to miscommunicate the intentions and feelings of the cosmetic surgery patient.
Although most patients who seek cosmetic surgery have a clear understanding of what they wish to achieve, a subset of patients have body dysmorphic disorder (BDD) or dysmorphophobia (9). This subpopulation of patients includes 2% of the general population and possibly 7% of the cosmetic patients who seek surgical consultation (10). Patients who meet the diagnostic criteria for BDD tend to have a general dissatisfaction with their overall appearance greater than the normal values of the general population. This level of satisfaction is defined in terms of “body image” that includes a cosmetic surgery patient’s perceptions, thoughts, and feelings about his/her body. Such patients demonstrate significantly greater dissatisfaction than a “normative sample” when queried about a specific bodily feature (11).
Rohrich (12) indicates that patients with BDD fixate on an imagined defect in appearance. This defect is exaggerated out of proportion to its severity to such a degree that the patient suffers significant distress. These patients are consumed by this “defect” and fixate unnecessarily on a particular portion of their anatomy. They constantly seek and undergo multiple surgeries and opinions. There is a resultant negative impact on their social and professional lives.
Patients with body dysmorphic syndrome or dysmorphophobia should be identified, if possible, because they may become distraught after surgery (12,13). Rohrich
states that cosmetic patient evaluation should include the patient’s personality traits, likes, and dislikes. The patient’s motivations for surgery should be clearly understood. If there is any suspicion of the disorder, a second visit, at a later date and prior to any surgical scheduling, may be helpful in sorting out these individuals. The patient with dysmorphophobia often is in a rush and does not want to wait to schedule surgery. The timing of the surgery should be appropriate and not rushed.
states that cosmetic patient evaluation should include the patient’s personality traits, likes, and dislikes. The patient’s motivations for surgery should be clearly understood. If there is any suspicion of the disorder, a second visit, at a later date and prior to any surgical scheduling, may be helpful in sorting out these individuals. The patient with dysmorphophobia often is in a rush and does not want to wait to schedule surgery. The timing of the surgery should be appropriate and not rushed.
Examination
Ophthalmologic examination includes a best-corrected visual acuity. Patients with any reduction in vision should be informed of the potential risks of surgery. For example, it is important to inform patients with underlying dry eye that irritation, transient blurred vision that usually results from postoperative edema, and tearing may occur after an upper or lower blepharoplasty. It is much better to warn patients of potential problems before they occur than to try to explain them after they have already affected the patient. The author has treated two patients with preexisting macular holes who were convinced that eyelid surgery adversely affected their vision. In each case, a retinal consultation was necessary after eyelid surgery to determine that the vision did not change compared to the preoperative visual acuity. In both patients, a postoperative tear film disturbance due to dry eye resulted in decreased vision for several weeks. In addition to visual acuity, it is essential to establish the ocular motility, including range of motion, and whether there is any preexisting ocular imbalance, such as a phoria or overt tropia. Superior oblique and inferior oblique palsies rarely occur after blepharoplasty.
EDITOR COMMENTARY
Postoperative diplopia occurs transiently due to local infiltrative anesthetic effects, especially on the inferior oblique or inferior rectus muscles after lower lid blepharoplasty. In addition, excessive dissection and cautery in the region of the superior and inferior oblique muscles should be avoided.
Evaluation of the Tear Film
On slit lamp examination, the tear film is evaluated. The author performs a Schirmer test after instillation of topical anesthetic. In addition, the tear breakup time is evaluated at the slit lamp. The tear breakup time should not exceed the interval between casual blinks at the slit lamp. The completeness and rate of blink should be studied at the slit lamp. In addition, the presence of a Bell reflex on forced closure is helpful in predicting whether exposure symptoms may develop after eyelid surgery. However, no test predicts with any degree of certainty those patients who will have dry eye symptoms after blepharoplasty.
The surgeon informs patients who have been diagnosed with dry eye about potential exacerbation of dry eye symptoms should an eyelid malposition develop after surgery. Such patients are warned about the need for increased topical lubrication after surgery. Specifically, this risk is increased by concomitant ptosis repair and brow lift. Any eyelid malposition such as lower lid retraction may exacerbate dry eye (6,7). Eyelid malpositions after blepharoplasty are much more closely correlated with postoperative symptoms and signs of dry eye than preexisting dry eye. In addition, partial paralysis of the orbicularis muscle due to denervation may have a similar effect. For this reason, skin-only dissection should be considered on secondary or revisional blepharoplasties. Furthermore, a lateral canthopexy to maintain lower lid position after cosmetic blepharoplasty helps prevent this complication in most cases.
EDITOR COMMENTARY
Any ptosis repair in severe dry eye may exacerbate the dry eye. Even uncomplicated upper lid blepharoplasty may precipitate transient but disabling postoperative symptoms by adversely affecting the precorneal tear film.
Patients who request a wide-eyed appearance must be educated about the need for conservative blepharoplasty. The velocity, completeness, and frequency of the blink may be adversely affected by upper lid scarring after surgery and result in damage to the corneal tear film. Removal of skin while retaining underlying orbicularis oculi muscle in upper lid blepharoplasty (14) potentially preserves eyelid function in patients who do not have excessively heavy redundant upper lid tissues.
Inflammatory Signs
Consideration of Thyroid Ophthalmopathy and Ocular Rosacea
Eyelid retraction, lid lag on downgaze and lagophthalmos, and decreased convergence may be found in patients with thyroid-related orbitopathy. Blepharoplasty should be reserved for patients with quiescent disease and undertaken after any proptosis, motility dysfunction, and eyelid retraction have stabilized for 6 months to 1 year or have been definitively treated. In patients with suspected thyroid eye disease, referral to an endocrinologist or internist may be necessary for appropriate systemic workup, including serum thyroid hormone levels (triiodothyronine [T3], levorotatory thyroxine [T4], thyroid stimulating hormone [TSH]). Orbital computed tomography may demonstrate enlargement of the extraocular muscles and increased orbital fat when systemic signs are completely lacking early in the course of the disease.
Ocular rosacea, a common condition, should be noted and may require treatment prior to blepharoplasty (15, 16, 17 and 18). The meibomian glands orifices of the eyelid margin are examined to determine if any lipid secretions are evident to suggest meibomian gland dysfunction that may be associated with ocular rosacea. In a series of 131 patients with ocular rosacea, the most common chief complaints related to the eyes were foreign body sensation, pain, burning, and redness (12). The most common ocular signs include telangiectasia and irregularity of the eyelid margin, meibomian gland dysfunction, blepharitis, and conjunctival hyperemia. The inflammatory condition has a predilection for the caruncle and plica semilunaris. Keratoconjunctivitis sicca occurs in approximately one fourth of patients (12). Isolated ocular findings without a skin rash are found in 15 % of patients (15). Tearing with partial nasolacrimal duct obstruction was not found in the series of 131 patients. In a review of 214 patients referred for evaluation of tearing over a 5-year period, seven patients had diagnosed acne rosacea with associated tearing and partial nasolacrimal duct obstruction on office lacrimal irrigation (18). All patients who complained of tearing responded to systemic doxycycline without further tearing after a minimal treatment period of 6 weeks. Acne rosacea is fairly common in patient population who are considering cosmetic blepharoplasty. The expertise of a dermatologist is recommended for patients with significant skin disease.
Symmetry of the Upper Lid Position
It is essential to observe the upper lid height and distance from the pupil marginal reflex to the upper eyelid margin (MRD-1) to assess preoperative symmetry. The distance from the center of the pupil to the lower lid margin (marginal reflex distance-2 [MRD-2]) is important as well. Even when the upper eyelid margins are symmetric with respect to the pupils, excess upper eyelid tissue that overlaps the
eyelid crease should be noted because mechanical ptosis may contribute to asymmetric MRDs. Manually elevating the eyelids eliminates the weight of excess skin weighing down the eyelid margin. The vertical height (distance in millimeters from upper to lower eyelid margin at its greatest vertical height) of the palpebral fissure should be measured. The horizontal length of the palpebral fissure (distance in millimeters from the medial canthus of the eye to the lateral canthus) establishes the presence of a lateral canthal dehiscence. The elasticity of the lower eyelid or orbicularis function is measured by a snap back test. Any lateral canthal downward dystopia should be noted and documented by photography.
eyelid crease should be noted because mechanical ptosis may contribute to asymmetric MRDs. Manually elevating the eyelids eliminates the weight of excess skin weighing down the eyelid margin. The vertical height (distance in millimeters from upper to lower eyelid margin at its greatest vertical height) of the palpebral fissure should be measured. The horizontal length of the palpebral fissure (distance in millimeters from the medial canthus of the eye to the lateral canthus) establishes the presence of a lateral canthal dehiscence. The elasticity of the lower eyelid or orbicularis function is measured by a snap back test. Any lateral canthal downward dystopia should be noted and documented by photography.
Consideration of the Diagnosis of Myasthenia Gravis
Variability of the eyelid position and double vision suggest myasthenia gravis, although all ptosis generally worsens at the end of the day due to fatigue. Neurologic consultation should be considered in patients seeking cosmetic eyelid surgery who also have variability in upper eyelid position, intermittent double vision, and orbicularis muscle weakness on forced eyelid closure (19, 20 and 21). Other signs include a positive ice test, Tensilon test, and fatigue on sustained elevation of the upper lid. Improvement of blepharoptosis is more significant after the ice test than from rest alone (19). Rest has been shown to improve the ptosis eyelid position. A surgical glove is filled with crushed ice and placed on the more ptotic eyelid for 2 minutes. The ice test does not improve ophthalmoplegia. Edrophonium (Tensilon) administration remains the more definitive test. Single-fiber electromyography is more sensitive than repetitive nerve stimulation, and is 19% to 100% positive in patients with generalized myasthenia gravis and 80% to 88% positive in patients with ocular myasthenia gravis (22).
An exaggerated Hering Law sign is apparent when the manual elevation of the ptotic upper lid causes the other lid to droop significantly. A Cogan twitch sign is evident when the patient changes from downgaze to fixate at an object in upgaze. The upper lid position of the fixating eye initially assumes proper height but quickly drops or twitches down by 1 or 2 mm. Serum antiacetylcholine receptor antibodies are evident in more than 90% of patients with generalized myasthenia and 45 % to 65 % of patients with ocular myasthenia (20). False-positive elevations are found in first-degree relatives of patients with myasthenia but also in patients with amyotrophic lateral sclerosis, primary biliary cirrhosis, and tardive dyskinesia (20). Because thymoma occurs in 10% to 20% of patients, a computed tomographic study of the chest is indicated, and patients should undergo consultation for possible surgical thymectomy (19, 20, 21, 22 and 23).
In the case of blepharoptosis repair in patients with myasthenia gravis whose ptosis does not respond to medical treatment, surgical undercorrection is preferable to overcorrection and is generally the rule (24,25). In 18 blepharoptosis repairs performed in 11 patients (3 with systemic myasthenia gravis and 8 with ocular myasthenia gravis), diplopia worsened in 1 patient, exposure keratopathy developed in 1 of the 6 patients who underwent frontalis suspension, and recurrence ptosis developed 2 years after the initial levator surgery in 2 of 11 patients who underwent external levator advancements.
Lower Eyelid Laxity
A lower lid eye distraction test of more than 8 mm is considered abnormal. A snap back test demonstrates orbicularis oculi muscle tone. Based on these two tests and clinical judgment, the eyelid may require horizontal tightening at the time of blepharoplasty.
Consideration of Brow Lift
The issue of a brow lift should be discussed in almost all patients requesting upper lid blepharoplasty. In my opinion, this procedure should be reserved for patients
with asymmetric brows. In a patient considering a brow lift for cosmetic purposes, a brow lift may be simulated to some degree by Botox injections. This subject will be considered as its own topic in Chapter 4.6. The editor believes that in order to remove excess skin above the lateral canthus, it is simpler to excise the skin conservatively and recreate a defined eyelid crease than to perform a brow lift. The brow has to be elevated to such a significant height to “conceal the extra skin” that direct eyelid skin excision is the more appropriate treatment (Fig. 1.1). In addition, the risks of surgery include scalp scarring with possible alopecia and sensory disturbances of the supraorbital and supratrochlear nerve.
with asymmetric brows. In a patient considering a brow lift for cosmetic purposes, a brow lift may be simulated to some degree by Botox injections. This subject will be considered as its own topic in Chapter 4.6. The editor believes that in order to remove excess skin above the lateral canthus, it is simpler to excise the skin conservatively and recreate a defined eyelid crease than to perform a brow lift. The brow has to be elevated to such a significant height to “conceal the extra skin” that direct eyelid skin excision is the more appropriate treatment (Fig. 1.1). In addition, the risks of surgery include scalp scarring with possible alopecia and sensory disturbances of the supraorbital and supratrochlear nerve.
Eyelid malpositions such as ectropion and entropion are noted. All of these problems may be surgically corrected at the time of cosmetic blepharoplasty. Analysis of the skin type is important, including a history of allergies. In general, thin skin will not do as well as thick, soft, luxuriant skin.
Negative Vector Orbit
Patients with a negative vector orbit should be informed of the potential risks of increased lower eyelid retraction after surgery (26,27). Simple transconjunctival blepharoplasty alone should not change lower lid position.
Jelks et al. (28) recommend that “vector analysis from the lateral view” be performed in all blepharoplasty. This relationship is appreciated from any view but is defined as the relationship of the most anterior projection of the globe relative to the lower eyelid margin and malar eminence. If the globe is anterior to the lower lid and malar eminence, a negative vector relationship is present. A positive vector is present when the most anterior projection of the cornea is posterior to the anterior projection of the lower eyelid margin and the malar eminence.
Like Jelks et al., Codner (29) emphasizes that patients with prominent eyes are more likely to develop inferior malposition or ectropion. In contrast, patients with enophthalmos or deep-set eyes are at risk for anterior displacement of the lid away from the globe after lower lid surgery, even when a canthopexy is performed to stabilize the lower eyelid. Results of patients with prominent eyes should be demonstrated to patients with such negative vector orbits prior to surgery.
EDITOR COMMENTARY
A canthopexy should be considered in any patient undergoing lower lid blepharoplasty when the anterior lamella is surgically manipulated and especially when there is horizontal eyelid laxity. Transconjunctival removal of fat is the only time a lateral canthopexy is not indicated. This caveat does not wholly apply to patients with a preexisting scleral show. In such patients, elevation of the middle aspect of the lower lid may be necessary by use of a posterior spacer graft.
Objective Photographic Documentation of Findings
Preoperative photographs are taken and are available at the time of surgery and help confirm all measurements. Photograph views include the following:
Full face frontal
Full face right and left oblique
Full face upgaze
Full face downgaze
Full face smiling
Digital photography is invaluable because photographs are available for immediate review (Fig. 1.2). It is important to show photographs of patients who have undergone surgery and especially to demonstrate both excellent and good results. This exercise helps to establish reasonable expectations of what can be accomplished surgically. Photographs should be standardized.
General Medical Evaluation
A general medical evaluation should be performed at the discretion of the patient’s personal physician and certainly in patients with cardiovascular disease or other systemic disease that may affect the surgical procedure (5). This request should be in writing.
Informed Consent of Risk and Benefits of Surgery
Part of the informed consent process is showing the photographs of patients (as those discussed earlier) who have undergone surgery in order to help the patient understand what can be accomplished by blepharoplasty (30, 31 and 32). Informed consent clearly states that the “patient’s right of self-decision can be effectively exercised only if the patient possesses enough information to enable an intelligent choice….” The obligation of the physician is to present the medical facts accurately to the patient or individual responsible for the patient’s care and to make recommendations based on sound medical practice. The physician is ethically bound to help the patient make choices from among the therapeutic alternatives. The physician should provide medical information to allow patients to make choices from among the therapeutic options consistent with good medical practice.
In New Jersey, failure to obtain the patient’s informed consent may subject the physician to a claim of battery, medical negligence, and/or professional conduct. This duty may not be delegated. The risks of refusing to undergo a recommended procedure also must be explained. Simple completion of a form does not, in itself, fulfill the obligation of informed consent. Disclosure or information sharing and “deliberations” between physician and patient permit patients to make reasoned decisions about their health care. Such deliberations and information should be recorded in the medical record in order to help refute a later allegation that the treatment rendered was not authorized. This documentation ideally should include the nature of the treatment, its expected benefits or effects, its possible risks and complications, and any alternatives to the proposed treatment. Risks and complications of alternative treatments should be included. The witness to the signature only attests to the signature. A witness to the informed consent process can later verify that the process took place. Although tape recordings and videotapes may be used as part of the consent process to explain the procedure, these materials are not a substitute for the informed consent process, that is, the actual discussion with the patient (28).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree