Upper and Lower Blepharoplasty with Combined Blepharoptosis Repair
Joseph A. Mauriello Jr.
Blepharoplasty can rejuvenate the entire face when properly executed in suitable patients. The procedure is performed on an outpatient basis, requires 1 to 2 hours of operating room time, and has relatively little postoperative downtime. Patients may return to work in a few days to 1 week. Patients and surgeon seek a reproducible operative result with few, if any, complications. Although unfavorable results may occur with any procedure, such complications after elective cosmetic surgery tend not to be well accepted by patients and can adversely affect a busy patient’s life. Therefore, it is this surgeon’s opinion that complications should be minimized.
Goals and General Principles of Upper Blepharoplasty
The main goals of upper blepharoplasty are to create symmetric upper lid creases and folds above the crease in relation to symmetrically positioned eyebrows. The position of the crease is critical. The eyelid crease incision should extend beyond the lateral canthus if skin overhangs the lateral canthus so that redundant upper lid skin can be excised. Patients should understand that most of the upper lid wound is hidden in the eyelid, except when the eyelids are closed. The lateral portion of the wound is always visible, but the wound may be covered by makeup 1 to several weeks after surgery.
The features of youth are as follows (1):
Fuller upper lid
Lower upper eyelid crease in youth
Lateral eyebrow descent initially, with medial descent at a later age
Reduced skin tone and elasticity with corrugations in the redundant areas
The youthful upper lid has a lower eyelid crease (Fig. 2.1) and more volume. Again, age invariably results in loss of tissue volume in the entire face and “facial
soft tissue ptosis” (1). The author favors preservation of both muscle and fat, especially the retro-orbicularis oculi fat (ROOF), whenever possible.
soft tissue ptosis” (1). The author favors preservation of both muscle and fat, especially the retro-orbicularis oculi fat (ROOF), whenever possible.
EDITOR COMMENTARY
The editor believes that the essence of blepharoplasty is to remove only sagging tissues and bulges that detract from the observer’s view of the eye and to create symmetry.
Surgical Technique of Upper Lid Blepharoplasty
The distance from the eyelid margin to the upper lid crease should be symmetric. Attaining symmetric distances from the lower edge of the eyebrow to the upper wound is not crucial and may not be entirely possible due to minor asymmetry of the eyebrow positions. The upper eyelid crease almost always is visible, at least as a remnant centrally. With age, it tends to detach and lose its deep attachments at its lateral and medial extents. Blepharoplasty only serves to restore and reinforce this crease at possibly a slightly lower level.
Upper Eyelid Incision
The upper eyelid crease tends to be lower in youth. The soft tissue loss that occurs in the brow region mimics brow ptosis. Volume replacement has been shown to restore such aging changes (1). As stated earlier, higher upper lid incisions result in deep or hollow upper eyelid supratarsal sulcus due to:
Excision of skin and muscle
Visible hypopigmented scars
The eyelid crease should be formed at the appropriate level, which is dictated by its anatomic position, generally 6 to 9 mm centrally from the eyelid margin. Discrete cauterization of the retained orbicularis muscle in the upper eyelid crease region facilitates formation of the crease. Lowering the upper lid crease maximizes the brow to fold distance and reduces the ptotic appearance of the eyebrows (1). Flowers indicates that when one brow is lower than the other, he attempts to excise
slightly more skin and muscle from the side with the lower brow (2). In addition, the pretarsal skin component is attached slightly higher onto the anterior tarsus and/or levator aponeurosis on the side with the lower brow (2). In any event, he states that brow lifts may accentuate the loss of soft tissue.
slightly more skin and muscle from the side with the lower brow (2). In addition, the pretarsal skin component is attached slightly higher onto the anterior tarsus and/or levator aponeurosis on the side with the lower brow (2). In any event, he states that brow lifts may accentuate the loss of soft tissue.
EDITOR COMMENTARY
This author has little experience masking asymmetric brow ptosis by varying the heights of the upper eyelid crease incisions or amounts of upper lid tissue excision. He prefers to create symmetric creases and treat the brow separately, most often with botulinum toxin type A (Botox, Allergan, Irvine, CA) injections if the patient desires and believes that brow lifts may accentuate upper lid hollowness. A lateral canthopexy by elevating the lateral canthal tissue tends to compensate for such hollowness.
The lower upper blepharoplasty incision slightly increases the distance from fold to the eyebrow; in this manner, the brow appears less ptotic. Therefore, whenever brow ptosis is evident, the eyelid margin to crease distance possibly should be decreased slightly.
EDITOR COMMENTARY
Rather than arbitrarily measuring the crease with a caliper, the author invariably in primary blepharoplasty locates remnants of the patient’s crease. It may be less evident medially and especially laterally, yet a significant remnant of the crease can always be found. The author tends to err on the low side of the crease when the incision is made. The author uses a “V” suture lateral horizontal eyelid shortening that can be titrated to correct the appropriate amount of lower eyelid horizontal laxity (see section on Three-Step Technique for Lower Lid Blepharoplasty). This technique helps to open the palpebral fissure horizontally and create a more full upper eyelid by elevating the canthus.
The medial part of the wound should only extend beyond the punctum when excess skin is present, especially in elderly patients. Tension lines created by suturing the medial aspect of the wound may result in webbing. During surgical closure of the wound, any movement of the medial aspect of the wound when the adjacent skin of the nose is grasped indicates that a web will develop from the medial edge of the wound toward to nose. The orbicularis muscle is debulked slightly with a Westcott scissors or Bovie cautery using a Colorado needle from the upper and lower edges of the medial aspect of the wound.
EDITOR COMMENTARY
Conservative skin incision is accomplished by avoiding the traditional eversion of the lash margin by the pinch technique (1). Cautery of the orbicularis oculi muscle at the lower part of the skin excision creates adhesions and enhances the eyelid crease.
Excision may be limited to skin only in younger patients with minimal redundant tissues and few symptoms of heaviness of the upper lids. The upper eyelid crease should be maintained at its physiologic level, that is, where the preexisting eyelid crease is evident. The incision may be made at a slightly lower position in order to create the appearance of a relatively full youthful upper eyelid (1, 2, 3 and 4).
EDITOR COMMENTARY
In addition, the skin-only dissection certainly should be considered in patients with dry eye and, of course, in those with significant volume loss. Patients with abundant upper lid excess tissue may be better served by excision of skin and muscle.
Suturing the upper eyelid wound is initiated at a point just above but usually 1 to 3 mm lateral to the upper punctum. Again, the medial portion of the upper lid wound may be left unsutured as long as the skin of the upper wound edge and the skin of the lower wound edges are equidistant from the point at which the initial medial suture is initiated.
Skin sutures are removed at 7 days because of tension induced by redundant orbicularis muscle. The author prefers 6-0 plain sutures at this time.
EDITOR COMMENTARY
It is critical to remove a minimal amount of skin vertically in the medial third of the upper lid blepharoplasty incision in order to prevent vertical traction and lagophthalmos. In contrast, it is important to remove bulging fat medially but to retain temporal fat. This technique creates symmetry medially yet allows the upper eyelid to retain a youthful fullness.
Conservative Excision of Upper Lid Fat
Fat removal is minimized except when there are irregular bulges in the medial aspect of the upper eyelid. Fat excision is limited to medial fat, especially the fat that is white and located inferomedially. This fat can be distinguished from preaponeurotic fat, which is more yellow. Lateral fat pockets are retained in order to avoid an excavated upper eyelid appearance. Such lateral pockets generally do not bulge irregularly and should not be excised. Therefore, this author generally does not remove retro-orbicularis fat. Any irregular protuberances of fat medially are excised in order to create a “crisp” appearance. The bulging fat medially is perceived by the observer as interfering with a clear view of the eye. The eye itself is universally beautiful and expressive in combination with symmetric movements of the surrounding soft tissues.
Any medial fat bulge is excised and clinically appears as white fat. Most preaponeurotic yellow fat is retained. Frileck prefers to avoid fat removal. In fact, he places fat grafts in the upper eyelid during primary blepharoplasty (5) and asserts that surgical elevation of the brow will expose the latent hollowness that may have been masked by brow ptosis and dermatochalasis. A muscle-sparing skin excision upper lid blepharoplasty is performed (see Chapter 3). The implanted graft size is reduced by 10% in volume when an open sky technique is used for patients who previously had undergone upper lid blepharoplasty and were left with superior sulcus hollowing and redundant skin (6,7).
EDITOR COMMENTARY
The author believes that fat grafts complicate primary surgery and that the risks of scarring of the grafts should not be taken when a patient seeks primary upper eyelid cosmetic blepharoplasty. Such scarring may be unacceptable to patients undergoing cosmetic surgery. Dermis fat grafts may be performed as secondary procedures (see Chapter 3).
Concomitant Treatment of Blepharoptosis
EDITOR COMMENTARY
Any blepharoptosis should be addressed at the time of blepharoplasty. As outlined in Chapter 1, the surgeon must educate the patients about the risks and benefits of such repair and specifically the necessity to adjust the upper lid position within 2 weeks of surgery in the event a levator aponeurotic repair is performed.
Levator aponeurotic blepharoptosis repair is accomplished through the blepharoplasty incision. The technique of levator advancement should reduce or eliminate as many variables that may affect the intraoperative eyelid and, therefore, final eyelid position. The levator aponeurosis is advanced (a) without epinephrine in the local anesthetic to avoid stimulation of Müller muscle, (b) using a 6-0 silk rather than a monofilament nonabsorbable suture to secure the advanced levator to avoid possible cheese-wiring and late recurrence of ptosis, and (c) with excision of a strip of preseptal orbicularis muscle just above the tarsal border to create surgically apposed “raw” surfaces for firm attachment of the “advanced” levator aponeurosis (8).
An upper eyelid crease incision is made and a skin-muscle flap is undermined to within 3 mm of the lashes. A buttonhole is made through the orbital septum where the underlying fat bulge is evident. The tissues are elevated to prevent damage to the underlying levator aponeurosis. Adhesions between the orbital septum and levator aponeurosis are lysed, and the underlying levator aponeurosis is exposed by blunt dissection with cotton-tipped applicators. Often the levator aponeurosis is extremely thin medially, especially in older patients. A horizontal band of residual orbicularis oculi muscle and fused orbital septum and levator aponeurosis are excised just superior to the tarsus, and the underlying smooth pink Müller muscle is evident. Excision of these layers provides a cut edge for placement of the 6-0 silk sutures through the edge of the aponeurosis. Three double-armed 6-0 silk sutures are brought through the upper tarsus at its medial, middle, and lateral sites, and then each arm is brought through the edge of the levator aponeurosis. The patient sits up during the procedure to allow determination of the appropriate eyelid position and contour.
Postoperative adjustments in eyelid generally are delayed for 1 week after surgery to allow edema to resolve and to help predict final eyelid position. Levator adjustments may be performed as late as 14 days after surgery. In a series of 122 consecutive aponeurotic advancements in 110 patients (12 bilateral cases), 5 (4.1%) patients were candidates for revision because the operated eyelid was greater than 1 mm from desired height (8). All five eyelids were undercorrected by 2.0 to 2.5 mm. Four of the five patients underwent revision at 8, 11, and 14 days (two patients) after surgery. The fifth patient did not undergo revision. Four additional patients had overcorrections from 2 to 2.5 mm that resolved with eyelid massage.
After 14 days, the eyelid has sufficiently scarred, thereby prohibiting simple manipulation of the levator without sharp dissection of scar tissue. Additional surgery at this point contributes to excessive scarring that may impact adversely on normal eyelid function and blinking. Any compromised eyelid function may lead to exposure symptoms, especially in patients with dry eye. Furthermore, surgical planes are more difficult to define in the scarred lid. Revisional surgery may prove more traumatic than surgery performed within 14 days of the initial surgery. In such early revisional surgery, the eyelid wound is bluntly opened with forceps and minimal local infiltrative anesthesia. The levator sutures are easily found and adjusted (8).
Another approach to ptosis surgery is minimal ptosis surgery performed by a posterior conjunctival approach. When the posterior lamellar structures of the upper eyelid are excised, the anterior lamellae bulges anteriorly. The effect is to reduce unwanted skeletonization of the upper eyelid (see section on Müller Muscle Repair).
EDITOR COMMENTARY
The author almost without exception performs aponeurotic surgery because it provides a physiologic repair and does not sacrifice conjunctiva. Some surgeons perform Müller muscle resections or the Fasanella-Servat procedure and combine such surgery with blepharoplasty (9,10). Others stage the blepharoplasty component as a secondary procedure after Müller muscle resection.Two such procedures may be difficult for patients who need to return to work and full activities. In rare cases, contact lens wearing may be hampered by the conjunctival approach used in minimal ptosis surgery. Despite sacrifice of substantial conjunctiva, dry eye has not been specifically reported after minimal ptosis surgery. Minimal ptosis surgery results in consistent, predictable, and reproducible results in most cases. The main disadvantage of minimal ptosis surgery is that late reoperations demonstrate extremely scarred eyelids. In the author’s experience, repairs on such eyelids risk recurrent ptosis and poor eyelid function with resultant dry eyes in susceptible patients.
Approach to the Brow and Forehead
This subject was discussed in Chapter 1 and the surgical techniques are considered in Chapter 4.6. Nonetheless, patients sometimes ask about brow lift, and all should be informed about the subject prior to undergoing cosmetic upper lid blepharoplasty.
EDITOR COMMENTARY
The author does not favor brow lifts unless there is asymmetry of the eyebrows. The brows frame the eyelids and face; therefore, changes in the brow may change the patient’s facial appearance. The author believes that cosmetic blepharoplasty is restorative and, therefore, should not change the overall shape of the eyelids and brow and thereby the entire facial appearance of the patient. In the author’s experience, brow surgery is unnecessary unless there are significant aging changes that require such rejuvenation. In addition, as stated earlier, raising the brow may create a hollow in the upper eyelid that is accentuated rather than camouflaged (1,2). This hollow is not restorative and may make the patient appear older or even distorted. Elevated brows may appear unnatural. Finally, brow surgery may ultimately lead to asymmetry of the upper eyelid folds especially if the brows descend after surgery. Furthermore, dry eye may become apparent only after upper eyelid surgery is combined with brow elevation.
Swift et al. (11) attempted to quantify the effects of endoscopic brow lifts. Of the 25 patients carefully followed for a minimum of 1 year after endoscopic brow lift, 25% of patients had small areas of loss of hair adjacent to the wounds and scarring and 15% had changes in sensation that were noted at 1 year. These latter problems are lessened by fixation of the sutures to bone tunnels to raise the brow rather than fixation of the brows to screw. Bone tunnels may be difficult to fashion at the ideal position. Although no patients had a surprised appearance, Swift et al. reported that, after surgery, the highest point was at the medial brow. The medial brow was elevated 2.4 mm, and the lateral brow was elevated 2.1
mm. Although the ideal shape of the female brow is such that its highest point is over the lateral brow (lateral slant), in the study by Swift et al., the least elevated portion of the brow, tangential to the lateral corneoscleral limbus, was lifted only 1.9 mm. Corrugator supercilii resection often is combined with the brow lift (12,13).
mm. Although the ideal shape of the female brow is such that its highest point is over the lateral brow (lateral slant), in the study by Swift et al., the least elevated portion of the brow, tangential to the lateral corneoscleral limbus, was lifted only 1.9 mm. Corrugator supercilii resection often is combined with the brow lift (12,13).
In the author’s experience, brow lifts are rarely necessary when upper and lower blepharoplasty is performed. Patients who wish to undergo a brow lift are offered a trial of Botox prior to any surgical elevation of the brow. In this manner, patients experience somewhat similar results without the permanent effects of surgery. Moreover, proper brow grooming performed by a skilled aesthetician at a spa or salon often can camouflage asymmetries.
Such patients generally do not opt for a brow lift. It is increasingly evident that botulinum toxin type A injections have a cumulative effect (14,15) (see Chapter 4). In the series of Swift et al., the scowl lines (vertical lines between the eyebrows) were not effectively removed. Again, these lines may be treated in the office with Botox injections with virtually no risk.
Three-Step Technique for Lower Lid Blepharoplasty
The fundamentals of lower lid blepharoplasty address the issues of orbital fat excision and repositioning, if desired; lateral canthopexy and horizontal eyelid tightening; and tightening of the anterior lamella. Avoidance of a “hollowed-out” or skeletonized lower lid appearance and lower lid retraction has been the impetus for several techniques (15, 16, 17, 18, 19, 20, 21 and 22).
Simple transconjunctival blepharoplasty does not address the anterior lamella or horizontal lower lid laxity. In the author’s experience, transconjunctival blepharoplasty alone is rarely indicated (Fig. 2.2). In a study of 41 patients, Carter et al. (23) prospectively compared patients who underwent transconjunctival blepharoplasty combined with immediate carbon dioxide (CO2) laser resurfacing to those who underwent transconjunctival blepharoplasty with CO2 laser resurfacing performed 2 months later. Transconjunctival blepharoplasty alone resulted in an improvement in lower lid bulging in 92% of subjects, whereas lower lid wrinkling worsened in 46%. When transconjunctival blepharoplasty was performed with simultaneous CO2 laser resurfacing or with CO2 laser resurfacing 2 months later, a
statistically significant improvement in wrinkles occurred. The timing of the procedures had no significant effect on final outcome. No patient developed lower lid retraction.
statistically significant improvement in wrinkles occurred. The timing of the procedures had no significant effect on final outcome. No patient developed lower lid retraction.
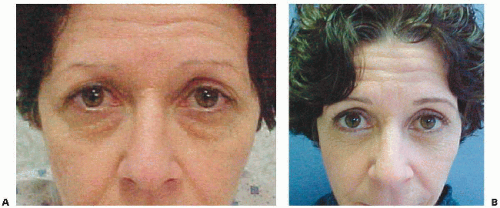
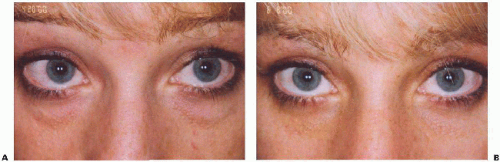 Figure 2.2. A: Patient prior to transconjunctival lower lid blepharoplasty. B: No change in longer eyelid position was evident 2 months after transconjunctival lower lid blepharoplasty. |
Although laser resurfacing corrects anterior lamellar rhytides, the author has found that anterior lamellar tightening is accomplished in a more controlled fashion and with less downtime using the three-step technique outlined below. This technique also corrects mild-to-moderate horizontal eyelid laxity. Skin rejuvenation is enhanced by a skin care program after surgery. Rarely is anterior lamellar tightening in the form of laser skin resurfacing or a medium-strength skin peel required. The three-step technique for lower lid blepharoplasty achieves all such goals in the following manner: (a) transconjunctival removal of unsightly orbital fat bulging that creates asymmetry, (b) “V” suture lateral lower eyelid horizontal tightening technique, and (c) resuspension of the orbicularis oculi muscle and, to some extent, the adjacent malar fat pad to the lateral orbital periosteum. Incisional surgery is optimally performed with a CO2 laser in a continuous mode in order to diminish intraoperative tissue distortion and thereby allow adequate intraoperative assessment of surgical manipulations and tissue draping at each of the subsequent stages. The laser also facilitates upper blepharoplasty and levator advancement. All skin incisions are made with a knife rather than the laser to prevent hypopigmentation of the wounds.
Step 1: Transconjunctival Fat Removal
A transconjunctival approach is the author’s preferred route to treat the orbital fat. The incision is extended medially below the caruncle in order to address the large medial fat pad. Conservative fat excision is performed to prevent a hollowed-out appearance to the eyelids. A central eyelid bulge is invariably due to fat just anterior to the inferior oblique muscle in the central portion of the eyelid. If desired, fat repositioning or grafting can be performed from the transconjunctival approach. The wound is closed with two or three interrupted 6-0 plain catgut sutures to restore eyelid anatomy and possibly to support the globe and present pyogenic granuloma on the raw conjunctival surgically incised edge.
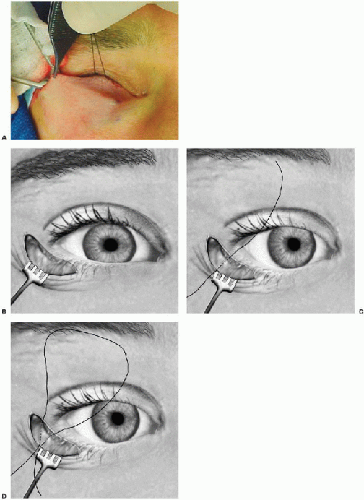
Once the fat portion of the procedure is complete, the “V” suture lateral lower eyelid horizontal tightening technique is performed using a mattress suture. A subciliary incision is initiated 5 mm medial to the lateral canthus and extends 5 mm lateral to it. The dissection involves skin only inferior to the level of the lower tarsal border in order to preserve pretarsal orbicularis muscle. The remaining inferior dissection is between the skin-muscle layer and the underlying orbital septum. Particular care is taken not to violate and thereby to preserve the orbital septum. Should the orbital septum be inadvertently incised and a large rent develops, the defect is sutured side to side to avoid vertical traction and to maintain a barrier to keep the fat in position posteriorly. The dissection extends inferiorly over the inferior orbital rim, laterally over the lateral orbital rim, and under the malar fat pad, the subcutaneous thickening of fat located above the malar eminence. This dissection is performed with the CO2 laser and has the effect of tightening the muscle and the overlying skin. Medially, blunt dissection with Steven scissors extends over the medial orbital rim (Fig. 2.3). The entire skin-orbicularis oculi muscle flap is raised with a portion of the malar fat pad. No effort is made to elevate the entire malar fat pad.
The appropriate amount of orbital fat excision can be visualized once the skin-muscle flap is elevated. When the skin-muscle flap is pulled superiorly and pressure is placed on the globe, residual fat that needs to be excised becomes evident. Similarly, the author also looks for bulges evident beneath the skin at the inferior orbital rim centrally. In this location, fat ensheathed by orbital septal extensions
just posterior to the inferior oblique muscle is apparent. The author does not generally perform a suborbicularis oculi fat (SOOF) or subperiosteal midface lift, orbital fat repositioning, or even fat grafting during primary blepharoplasty. Such procedures can be incorporated into the procedure at this time at the surgeon’s discretion. These procedures may complicate surgery unnecessarily.
just posterior to the inferior oblique muscle is apparent. The author does not generally perform a suborbicularis oculi fat (SOOF) or subperiosteal midface lift, orbital fat repositioning, or even fat grafting during primary blepharoplasty. Such procedures can be incorporated into the procedure at this time at the surgeon’s discretion. These procedures may complicate surgery unnecessarily.
Step 2: “V” Suture Lateral Lower Eyelid Horizontal Tightening Technique
The “V” suture technique helps to prevent inferior scleral show and a rounded lateral canthus and is performed as follows. Two bites of a double-armed horizontal mattress 5-0 polydioxanone (PDS) suture are made. These bites are vertically oriented with respect to the tarsus to form a “V” so that the lid margin is tightened more than the lower tarsal border (Figs. 2.3B and 2.3C). The first vertical bite creates the medial arm of the “V.” This first bite is taken approximately 4 to 5 mm medial to the lateral commissure and penetrates partial thickness tarsus by entering and exiting its anterior surface from inferior (at the tarsal base) to superior. This first bite exits 2 mm below the eyelid margin. Care is taken not to incorporate the superior skin edge of the subciliary wound. In order to assess and thereby correct lower lid horizontal laxity, the lower lid is distracted laterally from the superior edge of the tarsus where the first bite exits. If the lateral eyelid margin buckles, a lateral tarsal strip or full-thickness eyelid tightening may be necessary to obtain sufficient
horizontal tightening. The bite of the second arm of the suture is taken from superior to inferior through the anterior tarsus and lateral to the first bite to form the “V.” The distance between the open arms of the “V” is determined by the lateral distraction test and represents the amount of horizontal laxity to be corrected. This suture traverses partial thickness tarsus and exits adjacent to the initial bite of the first arm of the suture at the base of the tarsus to create the apex of the “V.” Angling this second bite inferiorly toward the lower tarsal border creates the modified “V.” When the arms of the suture are tied at the base of the tarsus, the superior arms of the “V” are closed. The eyelid margin just above the open arms of the “V” is tightened more than the base of the “v” at the lower tarsal border.
horizontal tightening. The bite of the second arm of the suture is taken from superior to inferior through the anterior tarsus and lateral to the first bite to form the “V.” The distance between the open arms of the “V” is determined by the lateral distraction test and represents the amount of horizontal laxity to be corrected. This suture traverses partial thickness tarsus and exits adjacent to the initial bite of the first arm of the suture at the base of the tarsus to create the apex of the “V.” Angling this second bite inferiorly toward the lower tarsal border creates the modified “V.” When the arms of the suture are tied at the base of the tarsus, the superior arms of the “V” are closed. The eyelid margin just above the open arms of the “V” is tightened more than the base of the “v” at the lower tarsal border.
A small upward puckering of the lateral lower eyelid margin is created when the suture is tied (Fig. 2.3E). The lateral eyelid, therefore, hugs the globe and avoids anterior distraction of the eyelid margin and effectively corrects mild-to-moderate horizontal eyelid laxity. The degree of correction is assessed as the suture is slowly tightened and the lateral eyelid margin is observed. If the second bite is too anterior, that is, on the anterior surface of the lateral orbital rim and not inside the rim, the eyelid margin will pull anteriorly off the globe and the suture is replaced. The suture ultimately is tied at the bottom of the “V” to prevent prolapse or erosion of the knot through the subciliary wound.
Step 3: Skin-Muscle Flap Resuspension
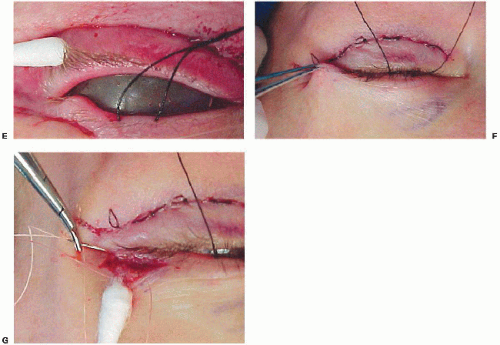
The previously undermined skin-orbicularis muscle and the attached malar fat complex flap are mobilized superiorly by grasping the superior edge of the flap. A horizontal bite of the orbicularis muscle from the superior edge of the flap is taken with a 5-0 polygalactin (Vicryl) suture. The location of this bite is critical because its placement will properly resuspend the entire flap and smooth the skin surface of the entire lower lid. The flap is suspended by a substantial bite of the periosteum at the appropriate position of the lateral canthus (Fig. 2.4). When this suture is properly placed, the skin appears flattened with minimal tension. The positioning of this flap is confirmed again with the patient looking up and mouth opened. The suture is replaced if necessary.
Because the pretarsal orbicularis muscle is intact from the initial skin-only dissection, any excess skin is excised from the superior edge of the skin-muscle flap. The patient looks up with the mouth open. Any small amount of redundant orbicularis muscle at the superior edge of the skin-muscle flap that now overlies the tarsal plate medial to the placement of the 5-0 Vicryl suture is then discretely excised. The skin edges are closed with an absorbable 6-0 plain catgut suture. The orbicularis oculi muscle and, to some extent, adjacent malar fat pad are resuspended and elevated. The so-called inferior arc of the orbicularis muscle contains interdigitations of the superficial musculoaponeurotic system (SMAS) at its inferior edge that bind the adjacent orbicularis oculi muscle (24). Hester and McCord suggest that check descent with age is partly due to ptosis of the orbicularis muscle. The three-step technique corrects the ptotic orbicularis oculi muscle and malar fat pad (24,25). It is important to distinguish the malar fat pad from a malar bag. The superior margin of the malar fat pad is at the same inferior margin of the malar bag.
EDITOR COMMENTARY
Lasering of the posterior surface of the orbicularis muscle serves to tighten the muscle and the overlying skin and obviates the need for significant lower lid skin excision. The contracture effect on the skin-orbicularis flap and the contour of the lower lid evolves 3 to 6 months after surgery due to the role of myofibroblasts in wound healing (25). The lasering and subsequent skin-muscle contraction eliminate the problem of excess skin in the lateral canthus.
Steri-Strips (3M, Maplewood, MN) are placed while the patient is recumbent and looking up in order to support the lower lid, effectively “damming” the fat back into the orbit and tamponading any postoperative edema. The Steri-Strips maintain the lower lid and cheek structures in a relatively superior position for 7 to 10 days after surgery. Intravenous corticosteroids administered the day of surgery and oral corticosteroids (prednisone 60 mg/day for the first 3 postoperative days) reduce edema and facial distortion. Arnica Montana pellets (Boiron, Newton Square, PA) as well as bromelain and papaya enhance the effect of oral corticosteroids by diminishing bruising and edema. Postoperative head elevation and liberal use of ice compresses allow the lateral canthus to heal in relatively upward position. Judicious horizontal tightening by the “V” suture lateral lower eyelid horizontal tightening technique further enhances the latter techniques. Tightening of the lower eyelid effectively supports and, to some extent, elevates the entire lower lid. This effect is enhanced by the skin-orbicularis oculi resuspension that also elevates the malar fat pad to some extent. Finally, in the eyelid region, orbicularis oculi muscle directly underlies skin. In contrast, elsewhere in the face, there is intervening subcutaneous fat between the mimetic facial muscles and the overlying skin. Because of this distinct anatomic feature of periorbital skin and muscle, both skin and orbicularis muscle may effectively be resuspended and fixated. Elevation and repositioning of this sphincterlike muscle provide support to the lower lid and reposit the orbital contents posteriorly. Anatomically, the malar fat pad is thickened subcutaneous fat.
EDITOR COMMENTARY
When the principles of this procedure are carefully applied, consistent symmetric results with improved lower eyelid position and malar fat elevation, to some extent, occur. Revisional surgery is rarely necessary for residual bulging of lower eyelid orbital fat and lower eyelid retraction. This technique is not optimal for patients with markedly shallow orbits and prominent eyes. Patients do not complain that their lower eyelids have a hollowed-out appearance. Fat repositioning is not necessary (Figs. 2.4, 2.5, 2.6 and 2.7).
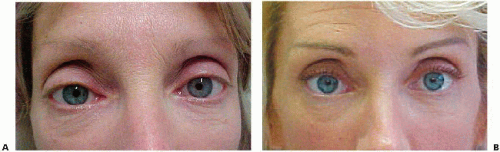
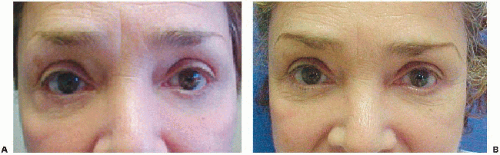 Figure 2.5. A: This patient, shown as a youth in Figure 2.1, underwent four-lid blepharoplasty 8 years ago. She is bothered by residual inferotemporal fat pad, lower lid retraction bilaterally, and upper lid nasal fat pads that create irregular bulges. Lower lid pulldown is evident 8 years after blepharoplasty. The cheek fat is depressed and residual fat is evident in the upper eyelids medially and in the right lower lid laterally. The upper eyelid creases medially are obliterated by the prolapsed fat and, notwithstanding the previous blepharoplasty, the crease is elevated compared to its lower location in youth (Fig. 2.1). The upper lids appear somewhat skeletonized. B: Six months after revisional four-lid blepharoplasty, note more elevated cheek and lower lid margin, especially laterally. More symmetric appearance is evident after surgery, especially after removal of right lateral lower lid fat prolapse. Residual fat is present in the right upper lid medially. The horizontal dimension of the palpebral fissure increases due to the use of the “V” lateral canthopexy. In addition, the lateral canthopexy has helped raise the lateral canthus and increase the fullness of the lateral aspect of the upper lid and creates the impression of a lowered upper eyelid crease. Overall, after surgery the lids appear more horizontal, less rounded and tired. |
Modifications of the Three-Step Technique
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree